Introduction
Since the introduction of dental implants, several advances have been made. To date, implant-supported complete dentures are frequently employed and the use of four implants to support complete mandibular or maxillary dentures has been described.1 No differences in force distribution when compared to dentures supported by five implants or improved force distribution resulting from angulated implants have been reported.2 The angulation of implants in the maxilla allows sinus grafting surgeries to be avoided, provides better implant distribution, and increases the resistance of the acrylic portion as a result of smaller cantilever extensions. This technique, named the “all-on-four treatment” concept, provides better biomechanics.3 In addition, the muscular activity when using this approach is similar to healthy dental patients.4
The success of implant-supported prostheses depends on successful osseointegration, which in turn is dependent on stresses transmitted by the prosthetic piece or by physiological stresses. Since the material used in the implant (i.e., titanium) is more rigid and resistant than bone, possible failure may occur at the bone or at the bone /titanium interface.5,6 Thus, a passive fit of implant-supported prosthesis is essential for the equilibrium of oral rehabilitation.7,8 In scenarios where passive fit of the prosthesis is not obtained, mechanical complications, including loosening or fracture of abutment components, loosening or rupture of the screw, or fracture of the metal framework may occur.9,10 Furthermore, biological problems resulting from a non-passive fit might result in adverse reactions in the implant-surrounding tissue such as pain, preimplant bone resorption, and complete osseointegration failure.11,12
A failure in passive fit can be the result of several factors during the clinical and laboratorial phases of the treatment, especially in the impression and pouring stages. Studies have assessed impression and pouring variables that would influence the passive fit of prostheses, including splinting or not splinting the transfers, the number and angulation of implants, the properties of impression material and stone, and the tray designs.13,14 Contrasting results are shown in the literature, and the best technique for an implant impression has not been clearly determined. It seems that splinting the transfers with acrylic resin has a positive influence on the accuracy of the impression.15 The type of tray might also positively influence the accuracy of the impression.16,17 In addition to all the previously referenced factors influencing the accuracy of implant impressions, the employment of the “all-on-four treatment” technique includes the angulation of two implants, and it is known that angulation of implants negatively influences the accuracy of the impression.18,19,20
Considering the lack of agreement in the accuracy of techniques for impression of multiple implants, the use of angled placement of implants in the “all-on-four treatment” technique, and the importance of obtaining a passive prosthesis fit, the aim of the present study was to evaluate different implant impression techniques in vitro for the impression of implants placed following the “all-on-four treatment” concept by assessing the passiveness of fit using a reference metal framework. The null hypothesis was that there would be no influence on the reference framework adaptation according to the different impression methods assessed.
Methods
The present laboratory experiment study used a reference metal model with a passive reference metal framework and multifunctional guide prior to the splinting and impression phases in the present in vitro study. The following variables were evaluated: precision and type of impression.
Fabrication of the reference metal model and the reference framework
A reference metal model was obtained from an edentulous maxilla cast (Fig. 1).
Perforations were performed, and four implants representing the regular platform and external hex (Conexão - São Paulo - Brazil) were placed. Two implants were placed parallel to each other at the premaxilla area (3,75 X 13 mm), while the other two (3,75 X 15 mm) were placed posterior to the canine fossa at a 45° angle, simulating rehabilitation based on the all-on-four treatment concept. Micro-Unit abutments (Conexão, São Paulo, Brazil) with 3 mm collars and a 30° angle were screwed on with 20 N.cm of torque. A framework was waxed over prefabricated Cr-Co calcinable cylinders, and a reference Cr-Co metal framework was obtained (Fig. 2).

Fig. 2 Metal model framework. Transfers and micro-unit abutments fixed with metallic bars (A). Metallic bars and transfers fixed to multifunctional guide using Pattern resin (B).
The metal framework was fixed with four sets of implants / abutments. Implants on the metal cast were screwed in at the lateral side on the medium third (Screw Allen) to certify the passive fit of the metallic framework and the stability of implants in the reference model. The lateral perforations of the reference metal model were fixed with a very hard GY 1109 / 943 epoxy resin (Hunstsman, São Paulo, Brazil).
Fabrication of the multifunctional guide
A complete denture was fabricated over the reference model. Artificial teeth (VIP, Pirassununga, Brazil) were assembled with nonspecific occlusion. The multifunctional guide was obtained using the impression of the complete denture with condensation silicone (Silicone Master, Curitiba, Brazil) and further PPR duplication.
Impression phase
A pilot study was accomplished to define the sample size. The initial 'n' used was based on previous studies in the literature. With the results obtained and considering a 95 % confidence interval and an alpha error of 5 %, the sample size was defined. After that the groups were created respecting the sample size obtained. Since the variables assessed in the present study were the method of fixation of transfers and the type of tray that was used (metallic or multifunctional guide), the groups (N = 30) were divided as follows:
Group 1 (n = 10): Impression with metallic open-tray without splinted transfer (MW)
Squared transfers were screwed into the reference metal model with a 1,17 external hex driver until resistance was noticed. Transfers were then screwed in with 10 N.cm with the aid of a manual torque wrench for standardization.21 The impression was performed with a metallic open-tray.
Group 2 (n = 10): Impression with metallic open-tray and metal-splinted transfers (MS)
Transfers were placed following the same steps described for Group 1. Next, the transfers were fixed with a circular metal bar (2,3 mm in diameter) and cyanoacrylate (Super-Bonder - Loctite - São Paulo, Brazil). The fixation was further strengthened with Pattern resin (GC - Japan) applied by the brush-on technique (Fig. 2A). The impression was performed with a metallic open-tray.
Group 3 (n = 10): Impression with multifunctional guide and metal splinted transfers (GS)
The same splinting procedures as in Group 2 were performed. Pattern resin was applied by the brush-on technique, fixing the metallic bars, transfers and the multifunctional guide (this last to the transpalatal bar) prior to the impression procedure (Fig. 2B).
For the three groups (N = 30), an additional cured silicone impression material was employed (ExpressTM XT, 3M / ESPE, Irvine, USA). The heavy body material was mixed according to the manufacturer’s instructions, and the light body material was mixed with the aid of a dispenser, syringe and tips provided by the manufacturer. Ten impressions were performed for each group.
For Groups 1 and 2, the light body silicone was injected over the areas surrounding the implant with a dispenser, a syringe and a tip, and the impression was continued using heavy body silicone placed inside the metallic tray. The amount of impression material was standardized by a stop fabricated on the reference model. For Group 3, the light body silicone was similarly injected over the areas surrounding the implant, while the heavy body was inserted into the multifunctional guide and pushed with digital pressure through the opening at the palatal area until it was full.
All procedures were performed under controlled room temperature (23 °C ± 2 °C) and humidity (50 % ± 10 %). After the impression material was set, the transfer screws were loosened and the impression and reference metal cast were separated. Analogs were then attached to the transfers prior to the fabrication of casts.
Fabrication of casts
Devices made of condensation silicone (Zetalabor, Zhermack, Badia Polesine, Italy) were fabricated for the purpose of standardizing the casts according to the amount of stone employed (Fig. 3).
Two hours after the impression material was set, type IV stone (Fuji Rock EP, GC America, Alsip, USA) was mechanically mixed under vacuum (EDG Equipamentos, São Carlos, Brazil) for 30 seconds according to the manufacturer’s instructions and poured into the impression in small portions. The stone was allowed to set for 60 minutes, after which the set impression / casts were separated. Casts were stored at room temperature for a minimum of 120 hours. A total of 10 casts were obtained in each group, with 30 casts in total. Both the impression and cast fabrication procedures were performed by the same operator, who was not the evaluator (RFA).
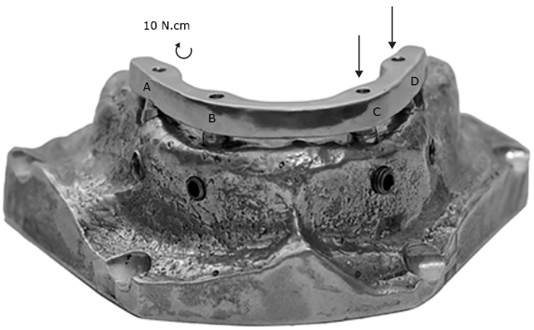
Misadaptation assessment
The four abutment analogs were sequentially named A through D, from left to right. The reference framework was seated over casts, and one titanium screw was tightened to analog A at 10 N.cm using a torque wrench. Misadaptation (gap) was assessed for the C and D analogs. The process was repeated with analog D receiving the screw and the misadaptation being assessed for analogs A and B (Fig. 4). The misadaptation assessment was performed with the aid of software (Leica Qwin, Leica Imaging System, Leica Biosystems, Wetzlar, Germany), and readings were performed on images with 100X magnification obtained from a camera (Model TK-C1380, JVC - Japan) coupled to a Leica stereomicroscope (Leica Stereomicrosystem, Leica Biosystems, Wetzlar, Germany).
The readings were performed by a blind evaluator who was not the operator (MEA). Marks on the reference framework were used in order to standardize the reading site for picture capture. Three linear readings of the gap-one mesial, one distal and one on the mark-were performed for each analog. A total of 12 readings were performed for each cast. A total of 120 readings were obtained in each group. Average misadaptation was calculated for each of the four tested analogs. The final misadaptation value for each cast was obtained using the average of the four analogs.
Results
The null hypothesis was rejected. There were statistically significant differences in the misadaptation (p < 0,001) of the reference passive framework according to the type of impression procedure used (Fig. 5). The use of a multifunctional guide (GS) for making impressions of the implants resulted in a similar yet smaller misadaptation of the reference framework compared to the open metallic tray with splinted implants (MS, p = 0,994). The use of an open metallic tray and non-splinted transfers (MW) resulted in greater gap when compared with the other impressions (p < 0,001).
Discussion
Several variables may interfere with the adaptation of the framework to implants for complete denture rehabilitation: mainly, the type of impression material employed, the amount of stone poured to fabricate the cast, the angulation of implants, the splinting method of transfers, and the use of different types of trays for impression.15,22,23 The use of standard amounts of stone during cast fabrication and the use of a single impression material allowed the influence of those variables to be avoided in order to specifically evaluate the implant impression techniques.
In addition to the previously referenced factors influencing the accuracy of implant impression, the employment of the “all-on-four treatment” technique includes the angulation of two implants, and it is known that angulation of implants negatively influences the accuracy of the impression. (19,20,22) The benefits of using the “all-on-four treatment” concept would be missed if the metal framework were not well-adapted with a relatively passive fit. The information present in the implant impression technique literature regarding the misadaptation of reference framework is somewhat similar to the present data.16,20,22) One study that evaluated the tapered and splinted impression techniques with plastic and metal trays with the same methods used in the present study showed a misadaptation between 32 ± 2 µm and 164 ± 58 µm, and the use of metal trays resulted in less misadaptation than the plastic trays.16 In the present study, the metal and multifunctional guide made with acrylic resin was more rigid than the plastic trays, and could produce results similar to the metal trays. Another important difference was that the trays in the present study were completely open, which may have benefited the impression technique with the metallic tray and multifunctional guide.
The splinted technique improves the accuracy of the impressions by preventing movement of the transfer during the impression making procedure, maintaining a more accurate relationship between the dental implants, as confirmed by the present study. However, the efficacy of these techniques is still controversial.24,25) One study that compared the accuracy between splinted and non-splinted impression techniques showed that the non-splinted technique produced a gap between the abutment and the framework of 205,86 µm while the splinted technique group presented a gap of 99,19 µm.26) Another study showed that the splinted technique produced a smaller gap size between the abutment and framework than the nonsplinted implants in angled implants (25º) specifically, but this difference did not occur in straight implants.25) Conversely, a study that compared the accuracy of seven impression techniques showed that the splinted impression technique did not improve the accuracy of the implant´s impression.27) The different results obtained from the present study could be due to the use of partially opened plastic trays that may have impaired the effect of transfer splinting on the reduction of gaps.
The decision to test the multifunctional guide in the present study was based on the fact that this device is already fabricated for the planning / placement phases of implants and would also serve as a customized tray for the impression procedure. The use of a multifunctional guide during implant planning / placing procedures allows for more precise implant positioning and angulation, and also gives an idea of the vertical dimension for planning clinical cases.28,29) Thus, the use of multifunctional guides for the impression as described in the present study, do not include an extra procedure, which would probably discourage the presently proposed technique.
The type of tray chosen in the present study was based on the fact that trays do not seem to influence the adaptation of the metal framework fabricated for implant supported oral rehabilitation.1,16 The metal tray was chosen due to clinical considerations since it is often used for this purpose. Additionally, transfers were splinted because this implant impression technique is proven to positively influence the process.5,14,26) Even when transfers are splinted with materials of different rigidity, the misfit is reported to be different10,30) with better adaptation for metal-splinted impression techniques. In the present study, the results are in agreement with observations in the literature, since the non-splinted method presented the worst misadaptation results at close to 110 µm.1,26) Both the multifunctional guide and the open metal tray with splinted transfers gave similar results, possibly due to the splinting method used.
The idea of using the multifunctional guide was to facilitate the impression procedure with a custom device already used during the phases of case planning and placement of implants. The real influence of the misfit on the mechanical and biological aspects of oral rehabilitation should be assessed in future clinical studies employing this impression procedure. Within the limitations of the in vitro present study, like absent of saliva and muscle that can difficult and alter the process, it was concluded that the MW group presented the worst mean values. The MS and GS groups were considered more precise methods, resulting in higher accuracy and fidelity in transferring implants. The use of a multifunctional guide with splinted transfers might be a clinical alternative for implant impression, reducing the clinical steps with precision.