INTRODUCTION
Solitary plasmacytomas are monoclonal proliferations of plasma cells that can arise in the bone or soft tissue, with normal bone marrow study, without bone lesions and absence of damage to the target organ.1 They represent less than 10% of plasma cell neoplasms and are classified as solitary bone plasmacytomas (PBS) and extramedullary plasmacytomas (EP). (2,3,4
Intracranial solitary plasmacytoma is very rare, representing lesser than 1% of head and neck tumors. 5 It can occur in the sellar and parasellar region, originating in the bone or mucosa surrounding the rock, sphenoid or clivus. (1
Its clinical presentation and imaging findings are similar to those of other regional tumors and often result in erroneous diagnoses such as pituitary macroadenoma,6) meningioma or chordoma in the spheno-clival region, being subsequently modified based on biopsy and immunohistochemistry; which delays its diagnosis.1,4,7,8
The solitary plasmacytoma of the skull usually has a good prognosis if the surgical removal is complete, not requiring radiotherapy; 50 to 60% of the PBS evolve to multiple myeloma (MM) and achieve a 10-year survival of 16%. 2,9,10,11
Plasmacytoma originated in the base of the skull is an extremely rare tumor and very few cases have been described in the literature. In this article we present the case of a patient with an initial diagnosis of pituitary macroadenoma who subsequently concluded in clivus solitary plasmacytoma by biopsy and immunohistochemistry.
CASE REPORT
A 47-year-old woman with a history of transsphenoidal adenectomy for sellar, parasellar and suprasellar tumor (pituitary macroadenoma) 2 months ago, admitted to the hospital due to moderate intermittent holocranial headache for 2 weeks, occasional nausea and vomiting, right hemifacial paresthesia and right eye diplopia. Physical examination showed cushingoid by steroid user, paralysis of the sixth cranial nerve of the right eye with no evidence of alterations in acuity or visual field.
Magnetic resonance of the brain showed a perintense tumor isointense in T1 and hyperintense in T2 of 58 x 35 x 34 mm within the clivus with exophytic growth extending to the sphenoidal, ethmoidal and cavernous sinuses, surrounding the internal carotid arteries. (Fig. 1)
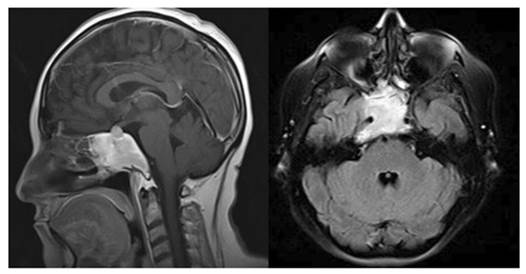
Fig. 1 Hyperintense tumor in T2 of 58 x 35 x 34 mm located in clivus that displaces the pituitary gland (A). Tumaor invading ethmoid sinuses and surrounds the internal carotid arteries (B).
The patient underwent to a spheroclonal tumor resection by transsphenoidal endoscopic route; histological examination showed abundant immature plasma cells in the periosteal and fibroconjunctival bone tissue (Fig. 2A). Immunohistochemical staining was positive for CD38 and kappa light chain, positive focal for CD20 and a ki67 proliferation index 5% (Fig. 2). In addition, the review of slides from the previous surgery was performed; concluding with the diagnosis of plasma cell neoplasia.
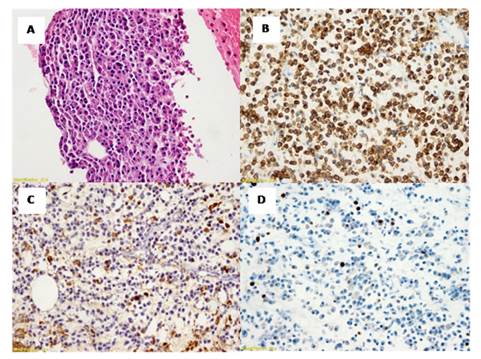
Fig. 2 Tumor of plasma cells with mild pleomorphism (A). Immunohistochemistry CD38 positive diffuse (B). Kappa light chain positive (C). Cell proliferation index with Ki 67 5% of tumor cells (D).
The patient underwent bone scan studies, complete blood count, serum calcium level, Bence Jones protein, urine electrophoresis proteinogram, myelogram and bone marrow biopsy, all normal; as a discard studies of multiple myeloma.
The electrophoretic proteinogram in serum gave a diminished gamma fraction with a faint band in its proximal third and by immunofixation an IgA class monoclonal band, lambda type, was visualized.
To confirm the diagnosis of clivus solitary plasmacytoma, positron emission tomography (PET-CT) was performed, finding a hypermetabolism in the solid lesion at the level of the cavernous sinus in relation to active tumor disease and no lytic or blastic lesions associated were found (Fig. 3).
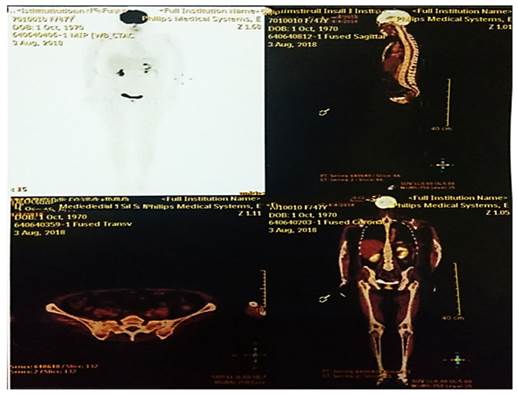
Fig. 3 PET CT18-FDG study in the maximum intensity projection does not show hypermetabolic areas at the level of the axial and appendicular skeleton.
It was treated with conformal 3D external radiotherapy by linear accelerator in doses of 45Gy/25F and is currently under follow-up.
DISCUSSION
Plasma cells tumors of the skull base remain asymptomatic for a long time, until their considerable size causes symptoms by compression of cranial nerves and headache, when they are located in the clivus the main symptom is diplopia by compression of VI cranial nerve and is an infrequent location within the base of the skull.11
The most common symptoms found in solitary intracranial plasmacytoma were headache, vomiting, convulsions, unilateral vision, visual field defects, diplopia, bone destruction or mass in the scalp or paranasal sinuses. (9, 11) The findings of a solitary lesion, bone marrow biopsy with less than 5% plasma cells, M protein minus 2 g/dL, absence of Bence Jones protein in urine, anemia, hypercalcemia or renal failure support the diagnosis of solitary plasmacytoma.9,11,12
Plasmacytomas originating in the sellar region are usually misdiagnosed as an adenoma due to their rarity and limited clinical experience in this location. The imaging differential diagnostic includes nasopharyngeal carcinoma, chordoma, meningioma, osteosarcoma, lymphoma, pituitary adenoma, metastatic carcinoma and multiple myeloma,10,11 making it difficult to diagnose by this means and requiring pathological and immunohistochemical assistance.4,6-9
About one third of the cases were initially diagnosed as meningioma; but, the correct diagnosis was not made until the biopsy or surgical resection.9) The main treatment is the total extirpation of the lesion; but when it invaded the cavernous sinus it is limited only to partial resection of the tumor and adjuvant radiotherapy due to its difficult access.4,9
In solitary plasmacytoma located in skull base, radiotherapy is the treatment of choice because it is a radiosensitive tumor and it has been shown that adjuvant chemotherapy in this pathology does not have a beneficial impact. However, it is the therapy of choice in cases of multiple myeloma and it should be taken into account that adjuvant and prognostic therapy differs from multiple myeloma, so a meticulous examination should be performed to rule out progression to this disease using PET-CT and regular follow-up after radiation therapy. 4,8-12
Intracranial solitary plasmacytoma is a rare illness and its location in clivus is unusual; it has a non-specific symptomatology and diagnostic helps images are not clear, so it tends to be confused with others diagnoses such as chordoma, pituitary macroadenoma, meningioma and other intracranial tumors, being difficult the diagnostic and requiring the help of immunohistochemistry in biopsy .
Early diagnostic, extensive extirpation of the tumor and adjuvant treatment with radiotherapy, are the keys to managing these cases. Due to the high risk of progression to multiple myeloma, a complete study and careful follow-up is required.














