Introduction
During the last decades, society has undergone drastic changes that have affected human behavior and lifestyle. Mechanization in the workplace, globalization of technology, lack of time and improvements in transportation are some of the aspects that have led to an increase in the consumption of fast food with a high caloric intake and sedentary lifestyle.1,2 In this sense, the notable increase in obesity goes in parallel with the increase in metabolic syndrome; it is currently considered a complex disorder related to adipose tissue dysfunction associated in most cases with its excessive accumulation in the body and that results in hyperglycemia. Currently, approximately 30% of the adult population has this syndrome, and this percentage has been increasing in recent years.3,4
The metabolic or cardiometabolic syndrome, also known as insulin resistance syndrome or syndrome X, is defined by the presence of obesity, fundamentally central, hypertension, diabetes, dyslipidemia, and a prothrombotic and proinflammatory state, which are risk factors for cardiovascular disease. Recently, fatty liver disease of non-alcoholic etiology (NAFLD) has been incorporated as the liver component of this syndrome. It is known that both genetic factors of susceptibility or resistance, as well as environmental factors such as diet, physical activity, aging, health care, education and socioeconomic status, among others, contribute to the development of the metabolic syndrome.
The genetics of these diseases is complex and can range from rare monogenic forms to the more common polygenic and multifactorial forms. It is important to highlight that the risk factors are those biological signs or acquired habits that occur more frequently in patients with a defined disease, in the case of those who intervene in vascular risk, they result in cardiopathy, peripheral vascular disease, cerebrovascular disease and diabetes mellitus due to the presence of insulin resistance. Smoking, dyslipidemia, followed by obesity, diabetes, high blood pressure and psychosocial factors are the risk factors associated with metabolic syndrome, which explain the high incidence of myocardial infarction (MI) and can be prevented and or treated with changes in lifestyle and, in some cases, adding pharmacological treatment.4,5,6
Therefore, it was a motivation to carry out the present study to characterize patients with metabolic syndrome from the clinical and epidemiological point of view; since apparently, this syndrome is being considered by the clinicians from a reductionist point of view, since diseases are treated separately and the notion of the syndrome is lost because the relationship between its components is not clearly known, and many of them are among the top ten causes of death in Cuba in recent years, being a true health problem in the adult population.
Methods
A descriptive and prospective study was carried out to characterize from a clinical and epidemiological point of view the behavior of patients with the metabolic syndrome admitted to the General Teaching Hospital Dr. Juan Bruno Zayas Alfonso of Santiago de Cuba in the period from January to December of the year 2019. The study group was constituted by the 640 patients with metabolic syndrome assisted in the Internal Medicine Service of this institution during the indicated period, who met the inclusion criteria within which there were: voluntariness to participate in the study, age over 18 years, both sexes, central obesity, history of dyslipidemias, diabetes mellitus and hypertension. Patients under 18 years of age, foreigners and those with disabilities which made difficult the study were excluded.
Throughout the research process, the four principles of bioethics were taken into account: beneficence, non-maleficence, autonomy and justice. Variables were operationalized and included: age, was represented in completed years, grouped in ten-years; biological sex; personal, family pathological history and toxic habits. They were analyzed according to the inquiry and the individual medical history. Regarding alcohol ingestion, patients were classified as social drinkers, risky drinkers, harmful drinkers, alcoholic dependent drinkers and current abstinent drinkers. Regarding smoking, the patient was considered not to smoke and in the case of smoking, it was classified as: light smoking, moderate smoking and severe smoking, the latter when he smoked more than 20 cigarettes or more than 6 cigars or pipes a day. In relation to ingested fat, it was defined as polyunsaturated when the presence of vegetable oil was identified excluding coconut butter and saturated when animal fat was identified, and none when fat was not used for food preparation.
Techniques and procedures were used to obtain the information, which included conducting an extensive bibliographic review on the subject at the Provincial Center for Medical Sciences using the MEDLINE and LILACS computerized systems, updated electronic bibliographies on the subject were reviewed (Infomed and Internet). The data were collected and the final results obtained. The information was processed and analyzed through the SPSS 11.5.1 System for Windows XP. For statistical analysis, percent was used as a summary measure for qualitative variables, which allowed presenting the results in containment tables and illustrative graphs.
Results
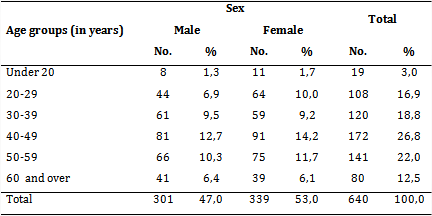
Table 1 highlights the predominance of patients between the ages of 40 and 49, 172 patients for 26.8%, and the predominance of women, 339 females for 53% of all cases. The extreme ages: under 20 and over 60, reported a lower percentage of patients (3% and 12.5%, respectively).
In table 2, diabetes mellitus and hypertension stand out within the personal history, 174 patients for 27.2% and 142 individuals representing 22.2%, respectively; similarly, in relatives diabetes mellitus predominated in 143 patients for 22.3% and hypertension in 110 patients for 17.2%. Ischemic heart disease, kidney, cerebrovascular diseases, hypercholesterolemia, and hyperthyroidism were reported in lower percentages.
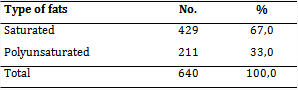
Table 3 shows the predominance of patients who consumed saturated fat, 429 representing 67.0%.
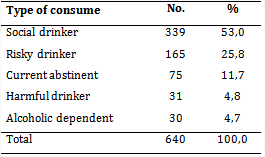
In table 4, social drinkers lead the results: 339 representing 53%; followed by high risk drinkers, 165 for 25.8%, and a lower percentage was revealed in alcoholic dependents.
Table 5 shows the prevalence of smokers with severe smoking, 301 for 47.0%. Only 41 patients (6.4%) were not smokers.
Discussion
The metabolic syndrome has been considered one of the epidemics of the 21st century, due to the alarming increase that it has had in recent years. It constitutes an emerging public health problem and affects broad sectors of the population, both children and adults. It is the result of a positive energy balance maintained over time, which is mainly characterized by an excessive deposit of fat in adipose tissue.7,8 In this research, patients between the ages of 40 and 49 predominated, an aspect that denotes how with the increase in age, metabolic disorders also increase, it is observed that this result was followed by the age group of 50 to 59 years, which coincides with different authors consulted.9
Other inquiries agree with the results of the present study, outlining that the prevalence of high blood pressure increases with age in all groups, ethnic groups and sex. It constitutes a serious problem in the geriatric age, since 65% of the population between 65 and 74 years suffers from it. In the non-Caucasian population the prevalence increases and in men up to the age of 50, then this latter pattern is reversed, as is known by the influence of estrogens on the female sex, which occurs with menopause.10,11
The metabolic syndrome comprises a group of risk factors for diabetes mellitus type 2 and for the cardiovascular disease, characterized by the presence of insulin resistance and compensative hyperinsulinism, associated with metabolism disorders of carbohydrates and lipids, high figures of hypertension and abdominal obesity.11 It is considered that insulin resistance is one of the main etiopathogenic factors of the metabolic syndrome, which may appear decades in advance and it is a predictor of its development. Personal and family associated diseases of the patients under study reflect the predominance of diabetes mellitus and hypertension. These results show the closed relationship existing between these disorders and the metabolic syndrome; in the same way it is good to highlight the family history related to the syndrome, as it is frequent that in same family chronic diseases are inherited, such as diabetes mellitus and hypertension.12,13
The blood pressure increases according to obesity degree. It has been proved that for each 10 kg of weight excess, systolic blood pressure increases 3 mmHg and diastolic by 2 mmHg. (NHANES III) it was observed with the opinion poll of North American health that the prevalence of hypertension, adjusted for age, increases parallel with body mass index (BMI). In Spain, in a study of almost 6 000 hypertensive patients older than 65 years, the 36.6 % had a BMI>30.13,14,15 Another investigations have shown that insulin resistance, associated to factors of genetic susceptibility condition a series of clinical alterations: hypertension, glucose intolerance, which ultimately leads to type 2 diabetes mellitus, arteriosclerosis as a consequence of the decrease in HDL cholesterol (high density lipoproteins), elevation of LDL (low density lipoproteins) and triglycerides.15
This research showed that the majority of patients consumed more saturated fat and a minority polyunsaturated fat. These results are related to lifestyle, where the consumption of fat is common in the diet of the study population, increasing the risks of suffering from different diseases such as metabolic syndrome. Recently, there is an excessive influence of aesthetic patterns expanded by fashion, while promoting a diet dominated by products which are youth's likes, such as so-called fast food (fast food), rich in saturated fats and simple carbohydrates and low in fiber that favor a high calorie intake. Different authors agree that the first therapeutic approach to mention in the patient with metabolic syndrome is lifestyle changes (diet and exercise).15,16 Some authors show results similar to those of this investigation.
In recent decades, the consumption of alcoholic beverages has been consciously incorporated into the lifestyle of most population groups, in various countries, and it can be affirmed that humanity has been linked to alcohol, from almost immemorial time. Toxic habits were valued in this research, demonstrating that patients who were social drinkers and severe smokers predominated, which infers that this population is susceptible to community intervention studies on these issues that affect metabolic stability and facilitate metabolic syndrome. Nine modifiable risk factors are described in the INTERHEART study, as predictors of acute myocardial infarction in 90%. These risk factors include smoking, dyslipidemia, high blood pressure, diabetes, obesity, diet, physical exercise, consumption alcohol and psychosocial variables (such as stress and depression).17
Women have a significant 25 % increase in risk of developing cardiovascular disease conferred by smoking compared to men.18 Other authors agree in their studies with the present results and point out that smoking is one of the most common drug addictions rooted in the population and the relationship between smoking, ischemic heart disease and hypertension demonstrated through coronary angiography. Others report that the damaging effect of nicotine contributes to the release of norepinephrine in the sympathetic nerve endings, also producing an increase in the secretion of adrenaline, a hormone that reduces arterial volume, which leads to hypertension as it causes spastic contractions of peripheral arteries favoring the emergence of complications, including metabolic syndrome, by joining the other risk factors previously studied.19,20
It is concluded that females prevailed between 40 and 49 years of age, with diabetes mellitus and high blood pressure, directly related to poor eating habits, alcohol intake and severe smoking, as modifiable risk factors. The aforementioned prompts consideration of education and health promotion aimed at patients with metabolic syndrome in primary care, as well as the verticalization of medical care for this group of patients in hospital institutions, for the prevention and control of risk factors for metabolic syndrome.