INTRODUCTION
Craniofacial anomalies are a diverse group of congenital head-and-neck abnormalities, being the most common the cleft lip, palate, or both, which can present as a unilateral or bilateral occurrence1.
Cleft lip and palate occupy the third place of all malformations worldwide2,3. They are accompanied by anatomical, esthetic, and functional condition4,5. That is the reason why an early intervention by the specialist in charge of its correction is necessary.
The basic treatment protocol for patients with cleft lip and palate consists on the use of pre-surgical orthopedic appliances, surgical repair of the lip and palate, and treatment of associated complications such as speech difficulties, otology, and dental anomalies6.
Pre-surgical orthopedics (PSO) in the treatment of cleft lip and palate was introduced by the Scottish prosthetic Kerr McNeil in the 1950s6-8. This author was the first to consider moving the maxillary segments prior to dental eruption and performed the first pre-surgical alignments9.
In 1993, Grayson et al described the pre-surgical nasoalveolar molding (NAM), which addresses not only the alveolus but also the lip and the nose8,10. The NAM consists of an intraoral appliance with a molding plate attached with nasal stents to mold the lip, alveolus, and nasal cartilages1.
NAM focuses on maxillary alveolar alignments, nasal septum uprighting; it encourages unrestricted maxillary growth, improves curvature of alar cartilages, and approximates lip segments into desired positions7. The NAM is a custom appliance; it requires multiple adjustments as the treatment progresses and the infant grows1.
Lip adhesion surgery is another form of PSO undertaken prior to definitive lip closure1. It was introduced by Johanson and Ohlsson in 1961 as a step prior to definitive unilateral and bilateral complete lip repair11.
Lip adhesion is a surgical intervention that helps approximate the cleft segments and idealize nose position prior to final lip closure, requiring lip surgery to become a two-step process. This additional procedure reconstructs a complete cleft into an incomplete cleft, which, in bilateral cleft patients, can help control the protrusive premaxilla prior to definitive lip surgery1. The increase in the volume of the orbicularis muscle, as well as the increase in the vertical height of the lateral and medial elements of the lip, are other benefits of this procedure11.
In the Maxillofacial Surgery service of the Pediatric Hospital of Matanzas, the principles of Grayson´s orthopedic nasoalveolar molding technique have been used since the late 1990s, while lip adhesion was incorporated into the protocol in 2015, just after the Maxillofacial Surgery service specialist returned from training at Boston Children Hospital.
Although pre-surgical orthopedics is widely used in the world, its effectiveness is currently controversial due to the limited availability of scientific evidence2.
As there is no research in the province on the results of pre-surgical orthopedic treatment in pediatric patients with cleft lip-alveolus-palate, nor about the use of the labial adhesion technique in the country, nor orthopedic linear measurements, the authors propose the need to carry out the present study, assuming as a scientific research problem the following: Which are the results that have been obtained with the use of NAM and lip adhesion on patients with complete cleft lip-alveolus-palate in the Maxillofacial Surgery service of the pediatric hospital of Matanzas between 2010 and 2020?
Taking into account the above-mentioned research problem, the authors define as the objective of this work: to describe the results of the use of NAM and lip adhesion in patients with complete cleft lip, alveolus and palate, treated in the Maxillofacial Surgery Service of the pediatric hospital of Matanzas between 2010 and 2020.
METHODS
An observational, descriptive, prospective research was carried out, in a universe of 16 patients with a diagnosis of complete cleft lip, alveolus and palate, treated in the Maxillofacial Surgery Service of the Matanzas pediatric hospital, during the period from January 2010 to December 2020.
Seven of these patients were born with this clinical condition before 2015, and were treated first with the NAM technique and then definitive surgery was performed, using Millard´s rotation and the advancement technique modified by Mulliken. The second group was made up with those who were born after 2015, after one of the authors of this research, Dr. García del Busto, the specialist in Maxillofacial Surgery of our service, was trained at Boston Children Hospital of Harvard University and that made possible the incorporation of the lip adhesion technique. In this second group, NAM was combined with lip adhesion, before performing definitive lip surgery with the same surgical technique.
In all patients under study, pre-surgical orthopedics began during the first week of postnatal life. This initial procedure, based on the principles of NAM, consisted on the placement of an acrylic plate with a nasal extension to which certain adjustments were made as maxillary growth occurred. The activation of the tutor or nasal extension was carried out in each of the medical consultation sessions until a slight ischemia of the nasal wing was achieved.
To complete the orthopedic action of the device, an elastic band of Micropore tape was added externally, which in addition to contributing to the orthopedic action, improved the position of the soft tissues and helped feeding.
Once the patients were around three to six months of age and had achieved the necessary orthopedic correction (distance between the ridges less than 5mm), definitive surgery was applied to the first group and nasolabial adhesion was performed in the second group.
After the adhesion was completed, the nasal tutor is removed, subsequently forming a groove in the anterior part of the acrylic plate equivalent to the size of the alveolar ridge, which allowed it to slide in the opposite direction, and contact between both sides is achieved once the muscle insertions move toward the midline as a result of lip adhesion. Three months later, the definitive Millard rotation and advancement technique modified by Mulliken is practiced.
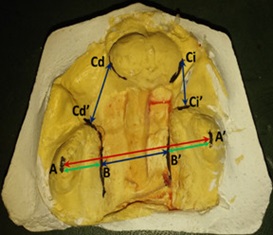
To verify the orthopedic changes that occurred as a result of the application of these techniques, a series of linear measurements were established on the study models of each patient based on reference points determined on the alveolar ridges and in the internal parts of the cleft, created for the purpose of this research by one of the authors, Dr. Calvo Pérez. These linear measurements precisely constitute the study variables. (Figure 1)
Points A and A’: most prominent points on the right and left alveolar ridge. Points B and B’: internal border points of the right and left palatine cleft. Points C: right and left lateral points of the premaxilla. Points C’: anterior points of the right and left lateral alveolar ridges.
It results in A-A’ being the linear distance that exists from the most prominent point of the upper edge of the right alveolar ridge to the left, coinciding with the maxillary width.
Distance from B-B’ is the linear distance from the inner edge of the right hemimaxilla to the inner edge of the left hemimaxilla, which corresponds to the width of the palatine cleft.
Distance from C-C’ is the linear distance from the right lateral edge of the premaxilla to the anterior edge of the right lateral segment and the linear distance from the left lateral edge of the premaxilla to the anterior edge of the left lateral segment, which corresponds to the width of the fissure in the alveolar area.
The measurements were taken by the examiner herself on study models at 2 and 3 different times, with and established interval between them. A marker was used permanently to locate the points and a caliper to take measurements.
The one-way ANOVA statistical test was applied to evaluate whether there are statistically significant differences for each type of operation at each of three stages (initial, with the use of NAM and one month after lip adhesion combined with NAM).
In addition, the Bonferroni test was subsequently applied, and that is the one that finally certifies the significance of the differences. That is, for there to be statistically significant differences with 95% reliability, the differences with ANOVA and Bonferroni must be significant.
First, all cases were evaluated regardless of the location and then the two fundamental locations were evaluated separately. In all patients, each of the moments or times, were assessed, coded as 0, 1 and 2.
The ethical principles were complied with during the research, and informed consent was given by the parents or guardians. An HP laptop was used, with a Windows 10 environment. The texts, tables and graphs were processed using the Office 2013 package, the SPSS statistical processor for Windows, version 15.
RESULTS
Three tables are presented to show the differences between the three measurement moments 0, 1 and 2 with respect to the study variables. In all cases, the ANOVA and Bonferroni statistical test were applied to determine the existence of statistically significant differences, presetting α=0.05.
When analyzing all patients (table 1), regardless of the location of the anomaly, as a result of the treatment a statistically significant difference was observed in the average width of the palatal cleft (B-B’) between the first (16.1mm) and second measurement moments (6.5mm), being it greater than 9.5mm. The third measurement moment applied to nine of them, showed a decrease in the mean of this variable of only 0.9mm.
Regarding the average alveolar cleft (C-C’), a statistically significant reduction was found between the first (8.6mm) and second measurement moments (3.6mm). The third measurement moment carried out in nine of these patients showed a reduction in the mean of this variable that reached 0.3mm.
The maxillary width (A-A’) and the right and left hemimaxillary A-B and A’-B’ respectively, experienced an increase in the average of their dimensions between the first and second measurement moments. At the third measurement moment, applied to nine of these children, there was also an increase in the mean magnitudes of these variables.
Table 1 Behavior of the variables in the three measurement moments in all patients
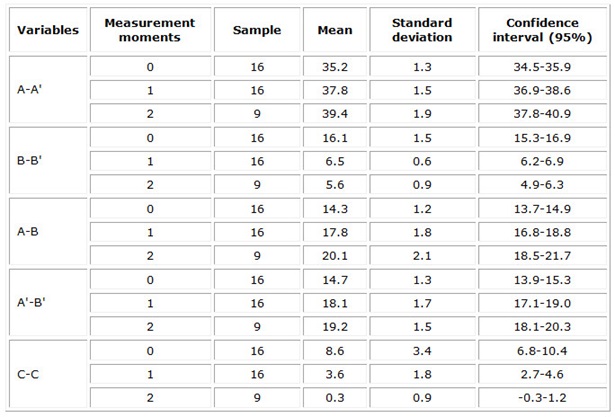
Legend: 0, 1, 2 measurement moments. 0 initial, 1 with NAM, 2 one month after lip adhesion + NAM.
When analyzing the behavior of the variables as a result of the treatment in the group of patients with complete bilateral cleft lip-alveolus-palate (table 2), a statistically significant difference was found in the mean amplitudes of the cleft palate (B-B’) between the first (16.4mm) and the second measurement moments (6.7mm), which exceeded 9.5mm. While the third measurement moment applied to five of the patients showed a decrease in the mean of only 1mm for the abovementioned variables.
The mean of the alveolar cleft (C-C’) showed a notable reduction between the first and second measurement moments on the right side (from 6.3 to 2.5mm), while on the left side it experienced a statistically significant reduction (from 8.6 to 3.6mm). The alveolar cleft was reduced to zero mm in the five patients in this group who underwent the third measurement moment.
The behavior of the average maxillary width (A-A’) and of both right and left hemimaxillaries A-B and A’-B’ respectively, showed an increase between the first and second moment of measurement and between the second and third moments. The latter was applied to five of these patients.
In the group made up of infants with complete unilateral cleft lip-alveolus-palate (table 3), the behavior of the variables as a result of the treatment showed a statistically significant difference in the mean width of the cleft palate (B-B’) between the first (16.0mm) and second measurement moment (6.4mm). In four of these patients, the third measurement moment was applied, reporting a reduction in the mean of this variable of only 0.8mm.
In the case of the alveolar cleft (C-C’), statistically significant differences were observed when comparing the measurements at all moments.
Table 2 Behavior of the variables at the three measurement moments for patients with complete bilateral cleft lip-alveolus-palate
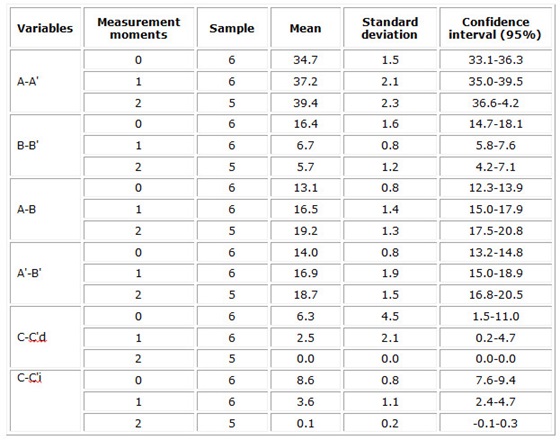
Legend: 0, 1, 2 measurement moments. 0 initial, 1 with NAM, 2 one month after lip adhesion + NAM.
The average dimension of the maxillary width (A-A’) and of both right and left hemimaxillaries A-B and A’-B’ respectively, showed an increase between the first and second moments of measurement and between the second and third moments.
Table 3 Behavior of the variables at the three measurement moments for patients with complete unilateral cleft lip-alveolus-palate
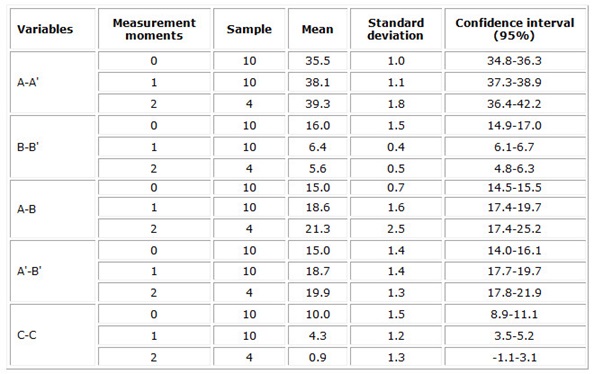
Legend: 0, 1, 2 measurement moments. 0 initial, 1 with NAM, 2 one month after lip adhesion + NAM.
Figure 2 illustrates the evolution of a patient with complete bilateral cleft lip-alveolus-palate after the use of the NAM and after lip adhesion combined with the intraoral device.

Fig. 2 Evolution of a patient with complete bilateral cleft lip-alveolus-palate after the use of the NAM and after lip adhesion combined with the intraoral device
a)Initial model of a patient with complete bilateral cleft lip-alveolus-palate, also characterized by the asymmetric position of the premaxilla. b) Changes produced by the use of NAM orthopedics (reduction of palatal and alveolar clefts, increase in hemimaxillary dimensions, and centralization of the premaxilla). c) Changes resulting from the combination of lip adhesion-intraoral acrylic plate (Retrusion of the premaxilla and total reduction of the alveolar cleft).
DISCUSSION
The patients included in the analysis began pre-surgical orthopedics before reaching the first week of age, therefore, we agree with the review study that was carried out by Riveros et al.12 in 2022 where they state that the pre-surgical orthopedics is successful when performed from birth to three months of age.
The authors consider that achieving early care for children with cleft lip and palate in the province of Matanzas, Cuba, is due to a close coordination established between the Medical Genetics, Neonatology and Maxillofacial Surgery Service, which allows the start of treatment in the first hours after birth.
The Medical Genetics service of the province, once it prenatally diagnoses the case, refers it to the Maxillofacial Surgery service that is responsible for carrying out the first consultation with the pregnant mother. In turn, the neonatology team, once the birth occurs, whether or not there is a history of prenatal diagnosis, is responsible for its immediate reporting.
Carlson et al.1 and Riveros et al.12 state in their research that nasoalveolar molding is a pre-surgical orthopedics method that helps reduce the width of the fissure before performing cheilorrhaphy and palatorrhaphy, an aspect that is evident in the present study.
On the other hand, Jolly et al.13 propose the significant reduction of the alveolar cleft through the use of NAM. At the same time, Sharma et al.14 in their study Role of the orthodontist in cleft lip and palate in 2021, refer to the effective retraction of the protruded premaxilla as a benefit from the use of NAM. The researchers of the present paper agree with this opinion.
It is the authors’ opinion that the use of the orthopedic plate eliminates lingual interference in the fissure area, which allows, during growth, an approximation of the hemimaxillary segments towards the midline and therefore a reduction in the width of the cleft. This transverse growth takes place both towards the midline and outwards, so the approximation of these segments occurs by stimulation of growth and not by collapse of the structures.
The authors propose that orthopedics aims at achieving an anatomical relationship close to normal and significantly reduce the size of the alveolar and palatal cleft prior to surgery. This reduction facilitates the coping of the palatal tissues during the surgical procedure, so we agree with Arteaga et al.8 and Kumar et al.7 that pre-surgical orthopedic techniques avoid extensive surgeries and excessive tension during healing.
The examiner’s skill is an important requirement to obtain accurate measurements, as expressed by Alfonso et al.15 in their recent research entitled “Transverse growth of the maxilla with the use of a pre-surgical orthopedic plate in patients with complete cleft lip and palate”, a criterion with which the authors of this study agree.
In a review analysis carried out by Agüero, et al.2 in 2021, which included 14 systematic reviews, they concluded that it was not prudent to incorporate pre-surgical orthopedics into surgical protocols as part of the treatment of patients with cleft lip-maxilla-palate, due to lack of scientific evidence. The researchers of this study are in total disagreement with this statement.
The professionals who carried out this study consider the need to motivate parents about the positive impact of orthopedics and its results of great importance to guarantee an easier and more successful surgery. We agree with Jolly et al.13 that one of the contraindications of NAM is the lack of parental cooperation despite repeated instructions.
Mulliken et al.11 propose that lip adhesion minimizes lip tension at the time of definitive surgery and uses the anterior muscular ring to retropose the premaxilla and align it with the lateral segments, and also reduces the alveolar cleft. This reduction is observed in all cases of the study.
In the research carried out by Thierens et al.16 in 2017, based on a systematic review that covered the available literature of the last 50 years on lip adhesion, they found the reduction in the width of the alveolar cleft after treatment with labial adhesion between 60.9% and 100% of cases affected unilaterally, while in bilateral cases this figure was between 47.5% and 100%. In the present investigation, the result of this procedure was the reduction of the alveolar cleft in 100% of the patients.
On the other hand, Thierens et al.16 also found in their study a reduction in the width of the palatal cleft after lip adhesion, between 28.4% and 59.8% for those treated with unilateral cleft and between 37.5 and 50.5% in bilateral ones. In the present study, minimal changes occurred in the width of the palatal cleft after labial adhesion. The authors consider that labial adhesion exerts direct action on the cleft at the level of the alveolar process, but not on the palatal cleft.
In the opinion of the authors of this research, the labial adhesion technique combined with the intraoral acrylic plate achieves closure of the cleft in the alveolar area because the former guarantees the coping of the soft tissues and the traction of the phrenic insertions and muscles towards the midline, while the custom-designed intraoral device with an internal channel in the alveolar area allows the sliding and coping of the alveolar processes that are pulled by the action of the soft tissues.
The researchers agree with Arteaga et al.8 and Saskianti et al.17 that PSO, as the initial treatment of complete cleft lip and palate, greatly improves facial aesthetics and minimizes the scope of surgery and surgical procedures.
NAM and lip adhesion used together result an effective combination in the treatment of complete cleft lip, alveolus and palate.