Introduction
In the 1980s, Wellen and colleagues1 described an electrocardiographic pattern with negative T waves in the right precordial leads associated with a severe lesion of the proximal anterior descending artery (LAD) (left anterior descending coronary T-wave syndrome). Years later, this new association was called Wellens syndrome (WS). Since the first published series, this syndrome has been associated with an unfavorable prognosis, especially in those patients who do not receive percutaneous coronary interventional treatment.
Approximately 14-18 % of patients seen in emergency departments with non-ST-segment elevation acute coronary syndrome (NSTEACS) present with SW.2 Two electrocardiographic patterns have been described: type 1 with biphasic T waves and initial positive component in leads V2 and V3, sometimes up to V4; and type 2 with negative, symmetrical and deep T waves in the same leads; both with relatively high sensitivity and specificity.
Although this syndrome represents a high-risk variant of NSTEACS, other causes that provoke the same electrocardiographic pattern such as cocaine consumption, myocardial bridging, and pulmonary embolism, among others, have been identified 3. Thus, this pattern is not exclusive to coronary artery disease. The objective of this presentation is to provide considerations on the pathophysiology of Wellens syndrome in a particular case.
Case report
A 66-year-old male patient with a personal history of smoking more than a pack a day presented with retrosternal oppressive pain, radiating to the neck and accompanied by vomiting and fatigue. An electrocardiogram was performed in the emergency service of his health area, showing biphasic T waves and initial positive component in leads V2, with ST-segment elevation of approximately 1 mm in leads V2 and V3, in addition to negative T waves in leads DII, DIII, aVF, V4-V6. (Figure 1). He was transferred to our hospital where he underwent an echocardiogram that reported: signs of ischemia at rest, and preserved left ventricular systolic function, with no evidence of myocardial necrosis.
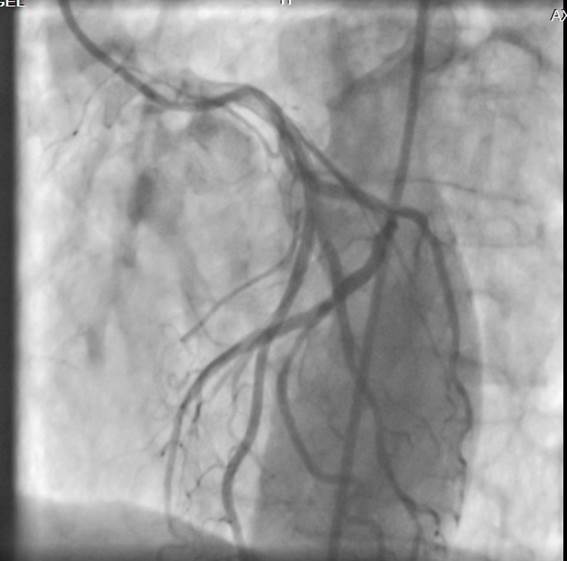
Within 30 minutes of admission, treatment for NSTEACS was administered with: dual antiplatelet therapy, anticoagulation with low molecular weight heparin, beta-blockers and statins. Coronary angiography was performed, which showed 80 % stenosis in the first diagonal artery (proximal location) and 50 % stenosis in the circumflex artery (distal location). (Figure 2). Stent implantation was performed in the first diagonal artery without complications. (Figure 3) The patient evolved favorably and was discharged on the 5th day, without manifestations of angina and with stable hemodynamic parameters.
Discussion
The presence of this syndrome as a high-risk variant of acute coronary syndrome in patients with chest pain and intermittent electrocardiogram abnormalities represents a diagnostic challenge at present. Its risk factors are shared with the traditional ones for coronary heart disease: obesity, arterial hypertension, diabetes mellitus, dyslipidemia, and smoking. On the other hand, the association of this syndrome with cardiovascular complications and reduced survival has been demonstrated in current studies, hence the individualized treatment of these patients is of paramount importance.4
During an acute coronary event, whether due to partial or total occlusion of an epicardial coronary artery, numerous alterations in the T wave and QRS complex occur. However, the presence of inverted and symmetrical T waves in contiguous leads are the result of a post-ischemic state of the cardiac muscle. In the particular case of SW this electrocardiographic alteration generally disappears, while the values of markers of myocardial necrosis are within normal or slightly elevated ranges.
Although the genesis of this syndrome is currently the subject of much conjecture and controversy, the effect of occlusion and subsequent spontaneous restoration of coronary flow in LAD is the most widely accepted hypothesis. This stunning of the cardiac muscle would trigger alterations in myocardial thickening and a transient state of left ventricular dysfunction. A current study that evaluated patients with SW by cardioresonance imaging found the presence of cardiac muscle edema during the acute event.5
Regardless of whether this pattern is associated with severe LAD occlusion, other causes and severe stenosis have been identified in other locations. The combination of a significant occlusion in an epicardial coronary artery, its spontaneous reperfusion and the added vasospasm caused by the effect of the atheromatous plaque on the vascular endothelium produce ST-segment and T-wave changes. Thus, a negative or biphasic T-wave pattern could be produced in the right precordial leads, without its origin being necessarily related to LAD occlusion.
Occlusion of the first diagonal branch, responsible for perfusion of the upper left septum and the anterior-superior aspect of the left ventricle, is expressed in the electrocardiogram as ST-segment elevation in leads DI, aVL and V2.6 Spontaneous occlusion and lysis of an atherosclerotic plaque in this vessel, as well as intermittent coronary vasoconstriction phenomena, lead to the formation of transmembrane potentials. These <<defective>> potentials manifest on the electrocardiogram as ST-segment deviations; if the ischemia is significant enough to affect the subendocardium, then ST-segment elevations and negative T waves may occur.7 If this occlusion is transient and the affected area recovers its perfusion, an electrocardiographic pattern similar to the Wellens pattern may be generated.
Conclusions
Regardless of the numerous advances in the identification of risk factors, diagnosis and treatment of ischemic heart disease, the management of patients with this syndrome has not been standardized. A group of patients only receive pharmacological treatment while others are revascularized by percutaneous intervention. An in-depth study of this syndrome and its inclusion in the guidelines on the diagnosis and treatment of NSTEACS would contribute to the knowledge and adequate management of this syndrome.