INTRODUCTION
The umbilicus is a unique physiologic scar; considered a vestigial organ resulting from the healing process of the umbilical cord ligated at birth.1,2,3) Its shape differs from person to person and it is located in the anterior abdominal wall, at the level of the highest points of the iliac crests, opposite the disk between L3-L4 vertebrae or L4 vertebra.1,4
Usually, it is a round to oval depressed structure with an average diameter of 1,5-2 cm that greatly contributes to the aesthetic appearance of the abdominal wall.2) The physical characteristics that contribute to an ideal umbilicus include size, shape, and location in the abdomen.5) Sadly, there is no consensus on what an appealing umbilicus looks like, but the critical components of the aesthetically pleasing umbilicus include small size, T-shape or vertical orientation, and superior hooding.1,3,6,7) Although, it is important to remember that the elliptical type of the umbilicus is more common than the round type, and males has slightly larger horizontal diameters while females has slightly larger vertical diameters.1
Despite it has no function, its absence leads to an unnatural abdominal appearance, and an abnormally shaped or misplaced umbilicus may draw undue attention to the central abdomen and can cause psychological and social complexes.1,2) In 1939, Thorek states that “an abdomen without a navel is like a face without a nose”.3) However, the umbilicus can be lost due to many causes, such as: older techniques of umbilical hernia or incisional hernia repair, after abdominoplasty, urachal cyst repair, omphalocele repair, gastroschisis repair, some tumor excisions, and mobilization of bipedicle or bilateral flaps for breast reconstruction.1,2)
Special mention deserves dermatological lesions because of the presence of many embryological remnants in which cases total or partial omphalectomy is mandatory.4,8) In such cases, neoumbilicoplasty is necessary due to the navel’s aesthetic importance to the abdominal wall its reconstruction most be considered a key aspect in the treatment planning.1,8
This article aims to present a case of neoumbilicoplasty with vertical island pedicle flap for a large pigmented umbilical nevus.
CLINICAL CASE
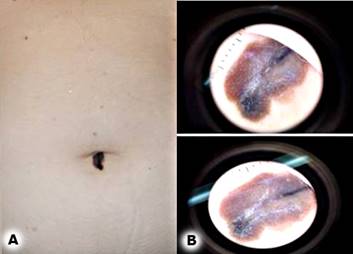
A healthy 50-year-old female patient with a history of a pigmentated nevus on the umbilicus since childhood was received in Dermatology´s consult complaining of changes in size and color of skin lesion. She also referred notice a lump in the upper umbilical region. On physical examination she presented an umbilical hernia and a dark-brown pigmentated umbilical macule with sharp irregular borders and 1 cm diameter in hour 6 of the clock (Fig. 1).
Due to the highly suggestive evidence of malignancy of the nevus and the umbilical hernia, the case was consulted with a multidisciplinary group. The consensus was to performed an omphalectomy with oncological margins, an umbilical hernia repair and a neoumbilicoplasty. A circumferential omphalectomy with 1 cm of oncological margin was performed (Fig. 2A); once the umbilicus was disinserted of the abdominal wall (Fig. 2B), a Mayo’s umbilical hernia repair was conducted and the central suture was reserved for the neoumbilicus fixation. Then the vertical island pedicle flap was made using the same diameter than the specimen. The subcutaneous tissue was dissected fallowed the same skin island diameter keeping its continuity with the anterior abdominal wall. Once the island flap was ascended to the umbilicus defect, it was fixed to aponeurosis with the prior reserved suture. Then several (start with fourth cardinal sutures) simple stitches were used to the closure of the neoumbilicus and intradermic for the closure of vertical incision (Fig. 2C).
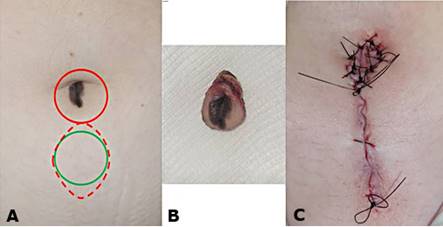
Fig. 2 A: Omphalectomy (red circle), vertical island pedicle flap (red dashed dots) and neoumbilicus (green circle). B: Specimen. C: Neoumbilicoplasty completed.
The patient was discharged 24 hour later without complaining. Pathology reported a Clark’s nevus with total excision. On day 6th of post-operatory a seroma was evacuated without any other complications. On 3 months consult the patient presented a total healing scar (Fig. 3) and she referred being satisfied with the outcome of surgery.
COMMENTS
Generally, umbilical lesions demand meticulous investigation; as such lesions may reflect serious hidden underlying disorder or malignancy. Detecting such lesions at the earliest is crucial for preventing complications. Umbilical benign tumors are most common, constituting 57% of all umbilical tumors. Primary malignant umbilical tumors are very rare, constituting only 17% of cases and the spectrum includes melanoma, basal cell carcinoma and adenocarcinoma.4)
Umbilical reconstruction or neoumbilicoplasty is performed, as previously commented, after abdominoplasty, abdominal flap surgery for breast reconstruction or in those cases when the umbilicus had to be removed.1 Commonly used methods include purse-string sutures for a small loss, and local flaps for a large loss, but these techniques do not yield cosmetically satisfying results.1)
Specifically, the components of umbilicoplasty can be broken down into umbilical incision, abdominal incision, suturing of the umbilicus to the rectus, stalk plication, periumbilical defatting, and skin suture.6 The variations of umbilical incision include round, round with superior excision, round with inferior excision, vertical ellipse, and inverted-U.6) Variations of abdominal incision include similarly round, vertical ellipse and inverted-U along with vertical line, Y-shaped, inverted-V chevron, double-opposing Y, inverted-V, and vertical oval.6) The goal of reconstruction for umbilical loss/absence is to obtain an umbilicus with a natural three-dimensional appearance and sufficient depression.5
A major concern in umbilical reconstruction is whether the structure is likely to flatten over time.1,5,7 Other complications included: plasty necrosis, infections, hematomas and scar hypertrophy.2,8) Moreover, in some cases, patients report hypo- or insensitivity around the neo-umbilical scar.2)
Despite the current body of literature regarding neoumbilicoplasty, there has yet to be written a reliable technique with a simple learning curve that achieves consistent and reproducible results in a wide variety of patients with different body habitus.6) Given the importance of the umbilicus as the central aesthetic unit of the abdomen, being able to achieve reproducible, cosmetically acceptable results is of upmost important.6
Neoumbilicoplasty with vertical island pedicle flap can be performed in the same surgical time than omphalectomy and its cosmetics results are adequate.8) Although it is a well-known technique used for facial defects reconstructions has been relatively unknown for the umbilical area.8)
This technique advantages are: the color, texture and depth´s tissue similitude also it does not compromise another anatomical areas.8) It is a plasty with a generous vascular pedicle and a low-tension closure which prevents graft necrosis and suture dehiscence; it also doesn’t require a long recovery time.8) This neoumbilicoplasty allows to cover moderate size defects like oncological omphalectomy and it can be made in the same surgical time with local anesthesia and excellent aesthetic results.8) Although various methods have been used for umbilical reconstruction, the ideal method has not yet been defined.5)
This case is a rare one not only because the umbilical skin lesions are uncommon but the neoumbilicoplasty technique is rarely used. The author couldn’t locale more than one previous reported case.