Introduction
In the course of the development of contemporary medicine, surgical planning has passed through a variety of distinct phases, which have paralleled the development of diagnostic imaging technology. In conjunction with advancements in image processing, modern acquisition methods such as computed tomography (CT) and magnetic resonance imaging (MRI) provide the surgeon with detailed reconstructions of the patient's anatomy, as opposed to the simple radiographs of the early 1900s. Due to 3D printing technology, we can now go from the virtual to the physical world.1)
This rapidly emerging technology uses CT or MRI data to build 3D reconstructed images of graspable objects. Thus, efficient patient-specific anatomical models can be produced. These can enhance a surgeon's understanding of the pathoanatomy of a patient and facilitate precise preoperative planning. The 3D-printed patient-specific guidelines can also aid in achieving accurate bone cuts, precise implant placement, and great surgical outcomes. Implants, casts, orthoses, and prosthetics can be customized to a patient's anatomy.2 We intend to investigate the publishing trends in utility of 3D printing in orthopaedic.
Method
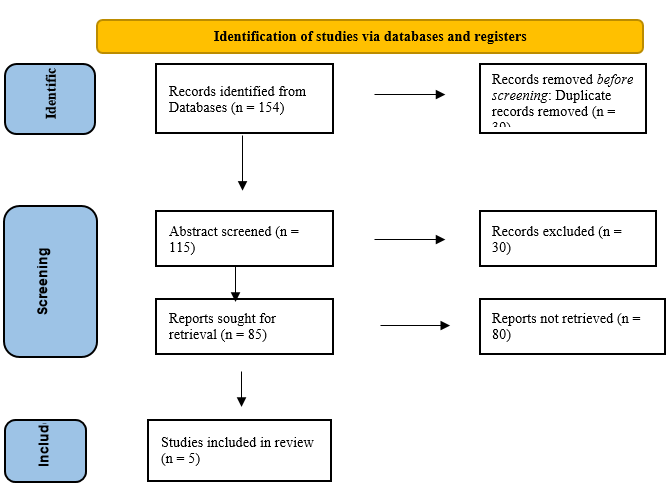
A literature search was performed on Google Scholar, NCBI, Clinical Key, Pubmed, and Science Direct. All articles pertaining to 3D Printing utilization in orthopaedics were extracted using appropriate search phrases ("UTILITY OF 3D PRINTING IN ORTHOPAEDIC" AND ("UTILITY, 3D PRINTING, ORTHOPAEDIC"). No time or evidence constraints were applied due to 3D printing in orthopaedics is still relatively new and the current evidence is primarily of low quality. The titles and abstracts of all duplicate and unrelated manuscripts were checked, and they were excluded.
| Study | Age | patient | Patology |
3D Printing primary application PRE-OP |
3D primary application INTRA-OP |
3D Printing Material | Pre-Op Imaging CT | Pre-Op Imaging MRI | Qualitative Outcome | Quantitatif outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
|
|
11.5 | 27 | Proximal femoral deformity (congenital/ acquired) | - | √ | Plastic polymer | √ |
-X-ray exposures -Radiography assessment: neck shaft angle, epidiaphysis angle, femoral anteversion |
||
|
|
6.6 | 11 | Developmental dysplasia of the hip (DDH), Neck of Femur (NOF) fracture | - | √ | Polylactic acid (PLA) | √ | Proximal femoral epiphyseal growth arrest |
-Operation duration -X-ray exposures -Radiography assessment: neck shaft angle, femoral anteversion |
|
|
|
10.9 | 25 | Developmental dysplasia of the hip (DDH) | √ | Polylactic acid (PLA) | √ | Proximal femoral epiphyseal growth arrest |
-Operation duration -X-ray exposures -Radiographic assessment: neck shaft angle, femoral anteversion |
||
|
|
16.0 | 1 | Distal radius malunion | √ | - | √ | - | Union radiography |
Clinical: ROM DASH score |
|
|
|
7,5 | 35 | Cubitus varus deformity (post-traumatic) | √ | Polylactic acid (PLA) | √ | Complications -Radiography union |
-Operation duration -Clinical: Elbow ROM, Deformity -Radiographic assessment: Carrying angle |
Results
From the five included research, it is evident that 3D printing has begun to be utilized intraoperatively in the orthopedic field. The majority of 3D printing components are Polylactic acid (PLA), while some research does not specify the constituents. Baskov et al.,3) Zheng et al.4) and Zheng et al.5) recorded usage for the femur, whereas Inge et al.,6 and Hu et al.,7 recorded use for the Radius and Humerus, respectively. The most frequently cited benefits of 3D printing are reduced operation times and x-ray exposure.
Discussion
The most important conclusion from the five studies is that intra-operation 3D printing reduces surgical operative time, fluoroscopic exposure, and blood loss. This outcome is consistent with adult population data collection.8 The most important quantitative outcomes were surgical operating time, fluoroscopy exposure, intraoperative blood loss, and radiographic data. Clinical examination indicators (such as joint stability, activity level, and discomfort) and surgical sequelae (such as avascular necrosis) were evaluated as qualitative outcomes. The comparative analysis did not identify a statistically significant effect in the pre-implementation study. However, improvements in qualitative results in terms of clinical assessment and complication rate have been documented.9
Three-dimensional scanning or 3D scanning is the process of retrieving data in the form of the geometry of an object to reconstruct the shape and 3D modelling of the object. The resulting 3D model is a collection of points arranged in the 3D space of the scanned object.10 The way 3D scan works is similar to a camera but uses more laser scanning, periphery projection, and photogrammetry (aerial mapping) methods. In many sectors, this leads to a 3D measurement approach and a virtual reconstruction of item surfaces. Generally, 3D scanning technologies function best on white or brightly colored object surfaces, which reflect light strongly. The 3D scan tool emits a laser to the object being scanned, then records the laser light reflected off the object's surface, and then the reflected light is processed into a collection of dots that make up the object being scanned.11
3D Printing, also known as additive manufacturing, is the process of creating or fabricating three-dimensional items using 3D models based on electronic data. Object models are 3D-printed using an additive process in which successive layers of material are added under computer control. 3D models (STL format) of the required objects are essential for this process.12
Utilization of 3D printing and additive manufacturing is anticipated to increase in the medical business. The utilization of technology in the production of orthosis prostheses and even human organs is becoming increasingly standardized. This market is still in its infancy, but it is anticipated that the usage of 3D Print in the medical field will expand. The 3D Print machine requires computer-aided design (CAD) data from the patient's anatomy to be realized in a physical model, so it needs to be preceded by the data acquisition process. Data acquisition is carried out by scanning the patient's anatomy using a 3D scanner or high-resolution medical imaging technology such as CT, MRI, etc. Then the acquired data will be processed in the form of image processing to create virtual models through dynamic and interactive simulations using CAD applications. Then the model is converted into a CAD .STL (stereolithography) file format. This G-code will then create .STL file to operate the 3D Print machine to produce shapes according to the model on the computer.13
Widely recognized are the advantages of 3D printing in comprehending complex abnormalities and gaining a better understanding of the treatment conditions.14 In pre-operative studies, surgeons can mimic 3D use procedures and better comprehend the 3D anatomy of the patient while deciding the appropriate size.9
In the diverse systematic study conducted by Levesque et al. in 2020, the application of 3D printing for pre-operative planning was the most prevalent, affecting a considerable proportion of the adult population.8
Conclusion
Orthopaedic use and utilization of 3D printing technologies are developing. Despite the relatively small evidence pool, these results imply the benefits of 3D printing technology in various deformity correction applications, particularly when applied "intraoperatively." To determine the potential benefits of 3D assessments, additional orthopaedics-specific high-quality research is required.