INTRODUCTION
People with autism spectrum disorder (ASD) have a high risk of developing oral pathologies, either because of their dependence on others or because the disorder makes it difficult to provide adequate treatment.1,2,3 Several studies have been carried out to determine the oral health status of people with ASD, however, results are inconclusive. Some authors suggest that the prevalence of caries is higher in people with ASD,4,5 others report that it is similar,6,7 or even lower than in people without ASD.2,8,9,10,11
Most authors agree, however, that the oral hygiene of these patients is deficient, and that their oral hygiene index is higher than in people without ASD.3,6,7,12,13,14 In addition, the Gingival Index (GI),2,7,12,14,15,16 Sulcus Bleeding Index (SBI),16 Bleeding on Probing (BOP),16 Probing Depth,16 and Community Periodontal Index of Treatment Needs (CPITN)14,17 have been reported as higher in people with ASD than in people without this condition. Bruxism,5-7,9,18,19 Pica disorder,18,20 mouth breathing,10 and pouching,21 are some of the oral habits that have been frequently reported.
In order to formulate public policies, it is essential to perform oral diagnosis of the most vulnerable groups, such as people with ASD. Research on ASD is scarce in Chile, however, and this study would be the first to determine the need for dental care in a group of Chilean subjects with ASD.
The aim of this study is to describe the oral health status, hygiene practices and oral habits of a group of Chilean children, adolescents and adults with ASD.
METHODS
This is a cross-sectional and descriptive study of the oral health status, hygiene practices and oral habits of a group of people with ASD. The study was carried out in different institutions for people with ASD in the Bio-Bio region, Chile, during 2016-2017. This research is part of a larger quasi-experimental study, which evaluated the effectiveness of a psychoeducational intervention program to facilitate the performance of the ten steps of a dental examination. The intervention consisted of five psycho-educational sessions with a pre-intervention, post-intervention and maintenance tests. The number of steps in the oral examination and behavior using Frankl’s scale were measured using the abovementioned tests.
This study was approved by the Ethics Committee of the University of Concepción (218-2015). All the subjects who agreed to participate in the study were asked to provide written consent.
123 subjects with ASD from a population of 188, with ages ranging from 4 to 23 years, were included in the study. Of these, 55 subjects completed the ten steps of a dental examination procedure during the pre-intervention test, and 68 completed the ten steps in the post-intervention test, after having attended the psychoeducational intervention program.
Each parent or caregiver of a person with ASD responded to a questionnaire which was previously applied in a pilot study in two centers of people with ASD. The questionnaire collected socio-demographic information (age, sex, and health insurance status of the person with ASD, the educational level of both parents), dental history (previous experience and dental treatment), oral hygiene practices (frequency of brushing, type of toothbrush, type of brushing and product used for brushing), and oral habits (bruxism, oral breathing, sucking/biting objects, Pica disorder, onychophagia, pouching, finger suction, hand suction, and others). This questionnaire was applied by a social worker trained in the care of people with ASD. In order to determine the social maturity of participating subjects, their parents/caregivers took the Vineland Social Maturity Scale test, Chilean adaptation (E/C), administered by a psychologist.
Two previously calibrated dentists obtained the variables for oral health status. Inter-observer agreement on clinical assessments was optimal with respect to qualitative variables (Kappa values> 0.81); and substantial agreement was obtained for quantitative variables (Lin Coefficient> 0.95). A portable dental chair and lamp were used to carry out the dental examinations in a specific classroom at each institution, following the recommendations of the World Health Organization (WHO, 2013). The variables included were:
Caries experience: dmft index for temporary dentition, DMFT index for permanent dentition and the total dmft/DMFT index (dmft index plus DMFT index) were obtained following the WHO criteria.
Caries prevalence: proportion of individuals with one or more untreated decayed lesions (D> 0 and d> 0).
Oral hygiene: the Simplified Oral Hygiene Index (OHI-S) was obtained from Greene and Vermillón (1964).
Gingival status: Loe and Silness’s gingival index (GI), measured using a dental probe.
Dental trauma: condition and number of affected teeth were determined following the WHO criteria.
Deep/ogival palate: presence or absence was determined by direct observation of the hard palate.
Anterior open bite, anterior and posterior crossbite: their presence or absence was evaluated by direct observation of the patient during occlusion.
Descriptive analysis of qualitative variables was performed using frequency tables (absolute frequency and percentage), and measures of central tendency (mean and median) and dispersion (± standard deviation) were used for quantitative variables. Results were organized by age groups (Group 1: 4-5 years, Group 2: 6-12 years, and Group 3: 13-23 years), and totals. ANOVA and Tukey’s comparisons methods were used to compare means, and a Kruskal-Wallis test to compare the medians. The chi-square test was used to compare proportions between groups. Tests were considered significant at 5 %. Infostat 2017 was used for data analysis.
RESULTS
Data was obtained from 123 people with ASD: 28 young children between 4-5 years old (Group 1), 73 children between 6-12 years old (Group 2), and 22 adolescents and adults with ages ranging from 13 to 23 years (Group 3). Details of the socio-demographic variables, dental history and the Vineland test are presented in table 1.
The higher their age, the higher also the total score, and the score for each dimension of the Vineland test. A statistically significant difference was observed in the total scores for the Vineland test by age group (p< 0.0001).
Most subjects had public health insurance. A high percentage of their parents reported having higher education. The older subjects had greater percentages of experience and previous dental treatments, resulting in statistically significant differences with values of p= 0.001 and p< 0.0001, respectively.
Oral hygiene practices: Only one of the 123 subjects with ASD had never brushed their teeth. The most common brushing frequency was twice a day (48.0 %), followed by three or more times a day (35.7 %), and once a day (15.4 %). Of the 122 subjects with ASD who brushed their teeth, 98.4 % used a manual toothbrush, and only 1.6 % used an electric toothbrush. Subjects with ASD who brushed their teeth but had never used toothpaste accounted for 10.7 %, and 84.4 % had never used a mouth rinse. Subjects with ASD who brushed their teeth without assistance accounted for 32.0 %, and 68.0 % depended on another person (table 2). The need for assisted tooth-brushing decreased as age increased, and statistically significant differences were obtained (p< 0.005).
Oral habits: 94.3 % of the 123 subjects with ASD had oral habits, 26 (92.9 %) in Group 1, 70 (95.9 %) in Group 2, and 20 (90.9 %) in Group 3. Bruxism and oral breathing accounted for the highest percentages of oral habits in the total sample (table 3). Statistically significant differences were found between age groups only for finger suction (p= 0.01).
Oral health status: The prevalence of caries in the 123 subjects was 33.3 % (41 subjects). The prevalence of caries in Group 1 was 10.7 % (3 subjects), 52.1 % (38 subjects) in Group 2, and in Group 3 no subjects had untreated decayed teeth; a statistically significant difference was observed between the age groups (p< 0.0001).
The total dmft/DMFT index for the 123 subjects was 2.6 ± 3.3; figures by group are presented in table 4. As age increased, the mean and the median of the total caries index also increased; however, no statistically significant differences were found (p= 0.42). When the medians are compared, however, the difference increases (0.0, 1 and 3.5 in Groups 1, 2 and 3, respectively). A greater difference is observed, and is statistically significant (p= 0.056).
Table 4 Mean scores (standard deviation) for decayed, missing and filled teeth, and dmft, DMFT and dmft/DMFT indexes for permanent and deciduous teeth by age group

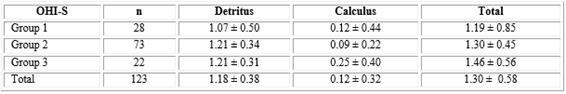
The OHI-S for the 123 subjects was 1,30 ± 0,58; figures by group are presented in table 5. The gingival index for the 123 subjects with ASD was 1,07 ± 0,43; 0,74 ± 0,48 for Group 1; 1,09 ± 0,32 for Group 2; and 1,40 ± 0,42 for Group 3. Statistical significance was only found in GI (p< 0,0001) when comparing OHI-S and GI by age groups.
Table 5 Mean scores (standard deviation) for Simplified Oral Hygiene Index (OHI-S) of subjects with ASD by age group
Twenty-five (20.3 %) of the 123 subjects with ASD had dental trauma, of which 7 (25.0 %) were from Group 1, 11 (15.1 %) from Group 2, and 7 (31.8 %) from Group 3. All the affected teeth were anterior; the upper permanent central incisors had the highest frequency (54.6 %). Enamel fracture was the most prevalent dental trauma (76.0 %).
The presence of deep/ogival palate was observed in 64 (52.0 %) of the 123 subjects with ASD: 18 (64.3 %) children in Group 1; 31 (42.5 %) children in Group 2, and 15 (68.2 %) adolescents and adults in Group 3.
3.3 %; 5.7 % and 8.1 % of the 123 subjects with ASD had posterior crossbite, anterior open bite, and anterior crossbite, respectively.
DISCUSSION
There have been many studies on oral health status and oral hygiene practices of people with ASD, but few include oral habits. Most of the studies use very wide age ranges as reference, mixing populations of children and adults,9,14,18,19,20,21,22,23 which makes it difficult to make comparisons between populations of people with ASD.
Only one subject in the present study did not brush their teeth; this figure was similar to that reported by Vajawat and Deepika,14 but much lower than that observed by other authors18,23 in subjects with ASD of similar ages. The highest brushing frequency was twice a day, similarly to that observed by other authors.18,23,24 In both groups of children (4-12 years old), however, we observed that the highest brushing frequency was twice a day, disagreeing with other authors who reported brushing only once a day as the highest frequency in their subjects.2,5,20 In the present study, 68.0 % of the subjects needed assisted tooth-brushing, a figure that is similar to the 70 % observed by Marshall et al.,22 but lower than the 75 %, 83.3 % and 88 % reported by Marshall, Sheller, Mancl,23Mansoor et al.24 and Klein and Nowak,21 respectively. There was greater autonomy in brushing with older ages; a figure that is similar to that reported by Marshall et al.22 All this suggests that as the age increases there is greater autonomy in performing daily routine activities, such as oral hygiene. 89,3 % of the subjects used toothpaste, similar to the 91 % observed by Marshall, et al.,22 15.6 % used mouth rinse, and 9.0 % only used water. These findings suggest that it might be difficult for these patients to get accustomed to new toothpaste or mouth rinse flavors, as these can produce sensory disturbances.
A high percentage of our subjects had oral habits. Bruxism was the most commonly reported by parents/caregivers (57.7 %), similar to the 60 % reported by Orellana, et al.6 in a group of adults, but higher than the 21.4 %, 32 % and 44 % observed by other authors in groups of children and adults.9,18,19 The prevalence of Pica disorder in the present study was higher than the 11.3 % observed by Subramaniam and Gupta20 in a group of children, but lower than the 46.4 % reported by Kamen and Skier18 in a group of children and adults with ASD. The percentage of pouching observed was higher than the 14 % reported by Klein and Nowak21 in a group of children and adults. The prevalence of both Pica disorder and pouching decreased in the present study, as the subjects' age increased; however, no statistically significant differences were observed.
The prevalence of caries in all subjects with ASD in the present study was similar to that reported Kopycka-Kedzierawski and Auinger,9 but lower than that reported by other authors.25,26 The prevalence of caries was lower in the group of 6-12 year-old children with ASD than that observed by other authors,2,8,27 however, the total dmft/DMFT index was 2.6, lower than the 3.7 reported by Marshall, Sheller, Mancl23 in a similar age group. We observed a lower DMFT index than other authors when comparing the 6-12 year-old group.4,8,16 According to the severity assessment of the WHO, the DMFT index found in all the subjects with ASD was very low (< 1.2). The prevalence of caries and the DMFT index increased with age, as reported by other authors.2,7,25,27 The highest score in the DMFT index was for caries, then for fillings, and last for missing teeth (D> F> M), which is similar to reports of other authors.6,11,17 This suggests that these patients lack access to dental care, and that their decayed teeth are not restored.
The OHI-S obtained in this study was lower than that reported in other studies,20,27 but according to the criteria proposed by Greene and Vermillón (1964), this figure could be considered regular (1.30-3.0). We observed that as the age increased, OHI-S worsened in people with ASD, agreeing with the findings of Vajawat and Deepika.14 The high percentage of deep/ogival palate found in our study is noteworthy, as it was higher than the percentage reported by Onol and Kırzıoğlu12 and by Orellana et al.6 in groups of 6-14 year-old and 20-41 year-old subjects, respectively.
In conclusion, most subjects with autism spectrum disorder in this study required assistance with tooth-brushing and brushed twice a day. Bruxism and oral breathing were the most prevalent oral habits. A low prevalence of caries, a very low DMFT index and a regular OHI-S were observed in the 123 subjects with autism spectrum disorder.
The main limitations of this study included the lack of a control group and the small number of subjects; therefore, it was not possible to further subdivide the sample by age groups.
Being aware of their oral health status and knowing the needs of the population with ASD at different ages is essential in order to prioritize public policies that focus on early preventive treatments in highly vulnerable groups. A poor oral health status can affect the quality of life of people with ASD, and their families.

















