Introduction
Oral lichen planus (OLP) is a chronic inflammatory disease affecting the oral mucosa with a variety of clinical presentations, including reticular, papular, plaque-like, atrophic, and ulcerative lesions.1,2 Clinical, histological, immunological, immunohistochemical and genetic investigations have not identified the initial trigger and pathogenic pathway that leads to the formation of lesions.3
The pathogenesis is believed to involve a T-cell-mediated response. However, the mechanisms triggering the T-cells to enter the oral epithelium and to accumulate in the superficial lamina propria, as well the triggering mechanisms behind basal keratinocyte apoptosis, are not fully understood. Also, it may involve both, antigen-specific and non-specific mechanism.4) Some general diseases, such as hypertension, diabetes, chronic liver disease and genetic predisposition have been associated with the etiology of the disease.5) OLP is currently classified as a potentially malignant disorder, but there are still conflicting reports on this potential.2,6,7
OLP affects middle-aged and elderly, and is more prevalent in women.3,4,8) The lesions are mostly bilateral and symmetrical, affecting predominantly the buccal mucosa, gingiva and tongue. It may appear isolated or associated with cutaneous lichen planus, the last develops by short-term outbreaks which usually respond well, and OLP tends to be chronic, relapsing and difficult to treat.2
In symptomatic OLP, patients normally complain of a burning sensation or pain when eating or swallowing hot or spicy food that affects their quality of life.5,9 High-potency topical steroids are considered to be effective drugs for palliative treating symptomatic OLP.10,11 Because of the chronic nature, completely healing the lesions is very difficult.1
Thus, the aim of this manuscript is to report a clinical case of OLP in gingiva whose removal was carried out by the de-epithelialization technique of the affected areas.
Case report
A female patient, 56 year-old, caucasian, presented to the clinic of a specialization in Periodontics, with the main complaint the "removal of a white spot on the jaw. The patient reported food accumulation in this region that made it uncomfortable.
At clinical examination, white plaques were not removed by scraping into the attached and papillary gingiva (Fig. 1). The diagnostic hypothesis was OLP. In addition, the patient had gingivitis. As a treatment plan, it was established that the same surgical procedure would be performed biopsy and removal of the white plaques, by the technique of de-epithelialization.12
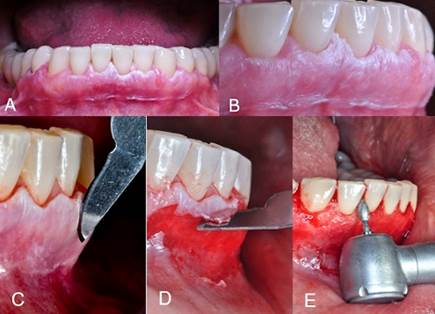
Fig. 1 (A) White plaques in the region of attached gingiva. (B) Lateral view of gingiva. (C) Beginning of the process of removing white plaques. (D) Removal of epithelial tissue and connective tissue exposure. (E) Use of a flame shape diamond bur in high rotation.
To perform the procedure, extra-buccal antisepsis with 2% chlorhexidine digluconate followed by intra-buccal antisepsis with 0.12% chlorhexidine digluconate. The infiltrative local anesthesia was performed from the mandibular second right premolar to the second left premolar with 2% mepivacaine with adrenaline 1:100.000 in a volume of approximately 1.8 ml. The technique consisted of removing the white plaques with a blade 15c along with the epithelial tissue from the gingiva, leaving the connective tissue exposed (Fig. 1C and 2D).
In the intrapapillary region, this process was performed with a flame shape diamond bur in high rotation (with constant and abundant irrigation with saline solution) (Fig. 1E).
This procedure does not require suturing. As post-operative medication prescribed was: amoxicillin 500 mg, every 8h for seven days, nimesulid 100 mg, every 12 h for five days, and paracetamol 750 mg, every 6 h for five days). After 24 h mouthwash was recommended every 12 h with 0.12% chlorhexidine digluconate.
The clinical follow-up of the patient was performed at three and 10 days, and then in two, three and 15 months. At the third postoperative day, a scar pattern was observed within the expected period with epithelization of the gingival tissue. After 10 days, the patient reported an improvement of the main complaint and improvement of esthetics.
In the second month the condition was stabilized with no change in the color and texture of the gingival epithelium. Also, it was verified through pathological anatomical examination the diagnosis of lichen planus chronic lichenoid mucositis with thickened squamous epithelium, hyperkeratosis compact and without atypical. Presence of acute inflammatory infiltrated chronic with many plasma and outbreaks of fibrosis. The basal membrane shows normal pattern (Fig. 2).
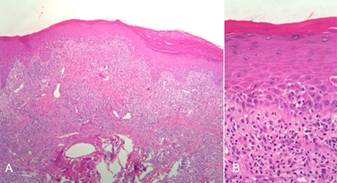
Fig. 2 (A) Histological aspect of the lesion removed. (B) Absence of cellular atypical and presence of inflammatory infiltrate.
After three months of follow-up, a new white plaque focus was observed. The option was to perform an excisional biopsy of the lesion and, again, the diagnosis found was OLP. After the last surgical procedure, the patient returned for follow-up (Fig. 3A).
Patient returned after 15 months to evaluate the clinical aspect. It was possible observe that until this moment there was no recurrence of the lesion (Fig. 3B).
Discussion
OLP is a chronic inflammatory disease of difficult treatment, with persistent manifestations for years, alternating periods of quiescence and exacerbation.2,13) It usually affects mouth, skin, nails, and may be involved with systemic diseases such as diabetes, hypertension and anxiety.3) It presents several clinical forms including papule, reticular, plaque, atrophic, erosive and bullous, each one showing specific characteristics and appearing in either isolated or associated forms.5
In this case report the patient presented manifestations in the skin, scalp and buccal mucosa. The disease manifested in the oral cavity were white plaques involving attached and papillary gingiva, and also striae in the bilateral jugal mucosa.
The clinical form of white plaques and the striae usually do not present painful symptomatology5) as in the present case, referred by the patient only as an aesthetic complaint. The patient stated that she was getting more embarrassed without smiling and being unable to socialize. She also complained that her hair was falling. A dermatologist also did a biopsy on the scalp and the diagnose was lichen planus.
The clinical aspect of patients affected by OLP with the erythematous and ulcerative type often suffer from severe oral mucosal pain, including burning and itching sensations, particularly in relation to the intake of spicy and acidic food, which may have a negative impact on oral functions as well as the patients’ quality of life and wellbeing.4,8
The diagnosis of OLP is based on the clinical appearance of the lesions and is subsequently confirmed by histopathological study, mainly to exclude the presence of epithelial dysplasia or even signs of malignancy. Also, there are controversies regarding the potential of malignancy of the OLP.2
The biopsy and total surgical removal of the gingival lesions, using a de-epithelialization technique12) were performed due to the aesthetic complaint and to rule out the possibility of cellular dysplasia. The surgical technique, here used, aimed to remove any affected epithelium and removal of melanocytic spots in patients who present aesthetic complaints due to gingival staining.12
In the researched literature, one case of excision of OLP by removal of epithelium was found in Contin et al.,14 which performed dermabrasion in the zygomatic region of a female patient followed by cosmetic protocol. There was an improvement in the clinical aspect, but after 12 months of follow-up, the melanocytic spots recurred. In the present case, after six months, the lesions returned to a lesser extent, but without aesthetic complaint. A new excisional biopsy was performed, again with diagnosis of OLP.
Even though there is no specific treatment for OLP, symptomatic treatment is indicated. Corticosteroids provide relief and are the first choice of drug.3) In the case reported by Sharma et al.,8) after surgical therapy for the control of gingival hyperplasia associated with erosive OLP, the authors indicated the topical use of corticosteroids with satisfactory results.
Due to the use of corticosteroids and the possibility of development of fungal lesions, some studies regarding the use of topical herbal medicines to control the lesions, such as curcumin and aloe vera, seem promising, but their effectiveness needs monitoring.13) Nosratzehi5 compared the use of corticoid with curcumin, showing the positive effects of the herbal product and no adverse reactions.
Despite the discussion about conservative treatments, the option in this case was the surgical intervention, with no prior medication attempt.
It was possible to observe that the clinical aspect of the gingiva after 15 months was satisfactory, but a long-term follow-up is necessary to be evaluated the conditions and to be analyzed a possible recurrence of the lesion. New therapies may be used in the patient if the lesion returns.
In conclusion, the technique de-epithelialization was resolutive from the aesthetic in this case. However, researches and new clinical cases must be carried out in order to achieve the use of this treatment.















