Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 no.3 Pinar del Río mayo.-jun. 2023 Epub 01-Mayo-2023
Articles
Management of the acute febrile child in the ED
1University of Medical Sciences of Pinar del Río. Provincial Pediatric Teaching Hospital "Pepe Portilla". Pinar del Río, Cuba.
Introduction:
fever is a response to the release of endogenous pyrogenic mediators called cytokines (in particular, interleukin-1 [IL-1]). Cytokines stimulate the production of prostaglandins by the hypothalamus; prostaglandins reset and raise the temperature set point. Knowledge of fever is vital in pediatric practice.
Objective:
to describe the essential elements in the management of the acute febrile child in the emergency department.
Methods:
for this bibliographic review, 38 research studies on the subject were consulted, obtained from national and foreign medical journals indexed in SciELO, IMBIOMED, PubMed, Latindex, Google Scholar, DOAJ, Dialnet, Medline and Scopus and 29 were used as bibliographies, with a predominance of articles published during the last five years and others due to their relevance.
Development:
fever is one of the most frequent reasons for consultation in Pediatrics, especially between three -36 months of life, and up to 65 % of children under two years of age will consult for this reason. It accounts for 10-20 % of acute processes in Primary Care and up to 30 % in Hospital Emergency Departments, especially in winter, coinciding with epidemics of respiratory and gastrointestinal viruses.
Conclusions:
the possibility of a serious bacterial infection makes it essential to carry out an adequate assessment of each child with fever that we treat. For this reason, physicians should have an optimal preparation on the management and adequate treatment of the febrile child at any level of care.
Key words: FEVER; PEDIATRICS; DEHYDRATION; TREATMENT
INTRODUCTION
Normal body temperature varies from person to person and throughout the day. Normal body temperature is higher in preschool children. Several studies have documented that the peak temperature tends to be in the afternoon and is highest around 18 to 24 months when many normal healthy children have a temperature of 38,3° C (101° F). However, a core (rectal) body temperature ≥ 38,0° C (100,4° F) is usually defined as a fever.1
The significance of fever depends on the clinical context rather than the peak temperature; some minor illnesses cause high fever, whereas some serious conditions cause only a mild rise in temperature. Although fear of fever often interferes with parental assessment, a history of temperature recorded in the home should be considered equivalent to an office temperature determination.1
Fever is a response to the release of endogenous pyrogenic mediators called cytokines (in particular, interleukin-1 [IL-1]). Cytokines stimulate the production of prostaglandins by the hypothalamus; prostaglandins reset and elevate the temperature set point.1
Fever plays an integral role in fighting infection and, although it can be bothersome, does not require treatment in an otherwise healthy child. Some studies even indicate that lowering the temperature may prolong some illnesses. However, fever increases metabolism and places demands on the cardiopulmonary system. Therefore, it can be deleterious in children with pulmonary or cardiac compromise or neurological impairment. It can also be the catalyst for febrile seizures, a usually benign condition in childhood.1
Although infectious diseases are the most frequent cause of fever, other non-infectious processes can also present fever, even as the first and only symptom at the beginning of the picture: autoinflammatory diseases -including Kawasaki disease-, autoimmune, metabolic, neoplasias. Generally, the characteristics of fever, its duration, periodicity, and the appearance of other symptoms will allow differentiating these conditions.2
Fever is one of the most frequent reasons for consultation in pediatrics, both in outpatient and emergency departments. It generates a lot of concern and fear in parents, which leads to repeated consultations and sometimes excessive and unjustified treatment. Health professionals working for children know that in most cases the cause is either easily identifiable or may be a self-limited viral infection, so our job is mainly to reassure the family.
The possibility of a serious bacterial infection makes it essential to carry out an adequate assessment of each child with fever that we treat. For this reason, physicians must have an optimal preparation on the management and adequate treatment of the febrile child at any level of care. In view of the above, the aim of this article is to describe the main elements to be taken into account in the management of acute fever in the emergency department.
METHODS
The scientific literature related to fever in pediatric ages, etiology, epidemiology and treatment guidelines was studied by consulting national and foreign medical journals indexed in SciELO, IMBIOMED, PubMed, Latindex, Google Scholar, DOAJ, Dialnet, Medline and Scopus.
Of the 38 articles selected, 29 were used as bibliographic references, with a predominance of articles published during the last five years and others, due to their relevance, published in English or Spanish. The inclusion criteria of the articles to be selected were: studies and clinical cases performed on pediatric patients with multiple pathologies where the common denominator is fever.
DEVELOPMENT
Important definitions
- Fever
Increase in body temperature above the values considered normal, resulting from elevation of the set point of the hypothalamic thermostat, without a single value for its definition.3,4,5
The values to consider fever would be:
- Fever without focus (FSF)
Fever that lasts less than five days, although some authors extend this period up to 10 days, and whose etiology does not appear after an adequate clinical history or an exhaustive and thorough physical examination.
The presence of isolated pharyngeal or tympanic hyperemia or mild rhinorrhea does not exclude the criterion of fever without focus.
In many cases, it will be of recent onset, less than six-12 hours.2,7
Other types of fever that should be distinguished are:
hyperthermia (especially in infants): excess of shelter, high thermal environment, Prolonged or continuous fever: fever that appears every day without periods of normal temperature and lasts more than five days.
Recurrent or cyclic fever: alternating episodes of fever with normal temperature.
Fever of unknown origin (FUO): febrile process that meets:
Temperature ≥38 °C ascertained by healthcare personnel.
More than two- three weeks duration.
Absence of diagnosis after one week of study (outpatient or inpatient).
Physiologicallow fluid intake, hyperconcentrated feeding.2,5
Important concepts in relation to FSF
Invasive bacterial infection (IBI): isolation of pathogenic bacteria in sterile fluid (blood, cerebrospinal fluid (CSF), pleura, joint fluid).
Potentially serious bacterial infection (PSAI): potentially serious bacterial infections which are, in addition to IBI, urinary tract infection (UTI), which is the most frequent, and acute bacterial gastroenteritis in children under three months of age.
Occult bacteremia (BO): presence of a pathogenic bacterium in the blood, otherwise with good general appearance and causing no other signs or symptoms other than fever: FSF and a normal or stable Pediatric Evaluation Triangle (PET).2,9,10,11
Epidemiology
Fever is one of the most frequent reasons for consultation in Pediatrics, especially between three-36 months of life, and up to 65 % of children under two years of age will consult for this reason. It accounts for 10-20 % of acute processes in Primary Care and up to 30 % in Hospital Emergency Departments, especially in winter, coinciding with epidemics of respiratory and gastrointestinal viruses. Each child presents between four and six episodes of fever per year and most of them are benign and self-limited viral processes. However, about 7-11 % will present with GBI, which can be complicated and even lead to death. Approximately 20 % will not be found to have a focus after a thorough history and physical examination.
Although infectious diseases are the most frequent cause of fever, other non-infectious processes can also present fever, even as the first and only symptom at the beginning of the picture: autoinflammatory diseases -including Kawasaki disease-, autoimmune, metabolic, neoplasias. Generally, the characteristics of fever, its duration, periodicity, and the appearance of other symptoms will allow differentiating these conditions.12,13,14,15
Risk factors to consider in the febrile child with fever without focus
Given that the main cause of a febrile syndrome without focus is infectious etiology. Among the risk factors to consider are:
Age less than three months (especially less than 21 days).
Affectation of the clinical condition (PET, validated scales, assessment by an expert physician).
Incomplete immunization against H. influenzae type b and pneumococcus.
Risk of UTI:
Age <12 months for uncircumcised boys < six months for circumcised boys; and < 24 months for girls (in circumcised infants older than six months with fever without focus, the probability of presenting a UTI, provided they do not present other risk factors, is less than 2 %, so urine sampling would not be indicated at the outset).
Temperature ≥39ºC or any fever lasting more than 24 hours.
Personal history of UTI, predisposing nephro-uropathy and recent manipulation of the urinary tract.
Infection transmitted through the mother: in newborns the risk of neonatal infection increases in maternal fever, prolonged rupture of membranes, Group B Streptococcus culture (+) and maternal history of genital herpes.
Hospitalization in the last two weeks.
Preterm infants <32 weeks or weight <1500 gr.
Current or recent antibiotic intake, within the last two weeks.
Social, cultural or remoteness factors that prevent adequate follow-up.2,9,13
Etiology
The most frequent etiology of FSF is infectious and within this group viral infections such as respiratory, gastrointestinal and exanthematous infections.
Classically, patients with FSF have been classified into three groups, since the immune response of the host and the infectious etiology of the process are different.
These groups are:
FSF in the less than 1 month old.
Higher risk of IBG, developing in 20-28 % of infants <28 days with FSF, favored by the greater immaturity of their immune system. However, viral infections can also be severe, with important sequelae such as meningoencephalitis due to herpes simplex virus (HSV), or sepsis-like pictures due to enterovirus.
As for bacteria, we will generally find those coming from the birth canal by vertical transmission, such as group B streptococcus (GBS) or S. agalactiae, E. coli, enterococci and L. monocytogenes. With the current approach to GBS colonization, the number of infections caused by GBS and, secondarily, by Listeria, which has almost disappeared by VT, has decreased. Currently, E. coli is the most frequently isolated bacterium in blood (60 %) and urine (87 %), with increasing rates of penicillin resistance in relation to the use of maternal antibiotherapy and its duration. GBS remains the most frequently isolated in CSF, causing more serious conditions such as meningitis (39 %), non-meningeal foci of infection (10 %) and early sepsis (7 %). Enterococcus and pneumococcus are very rare but serious causes; pneumococcal pneumonia at this age has a mortality rate of 14 %.
FSF in the one-three month old infant
The prevalence of IBG is 9-14 %. E. coli is the most frequently isolated bacterium, GBS is less frequent and Listeria is very rare. UTI is the most frequent GBI (75-84 %), mainly caused by E. coli, followed by BO (6-13 %), caused by E. coli (42 %), GBS (23 %) and pneumococcus (6 %).
FSF three -36 months
Various immunological and epidemiological factors mean that children in this age group have a non-negligible risk of GBI, especially if the rectal temperature is above 39°C (risk of occult bacteremia 3-5 %). This risk increases by 11% if the patient is not fully immunized. A patient who has received two doses of pneumococcal conjugate vaccine (PCV13) and two doses of pneumococcal conjugate vaccine (PCV13) and two doses of pneumococcal conjugate vaccine (PCV13) is called fully immunized. The most frequent etiologies of IBG are: S. pneumoniae, N. meningitidis and Salmonella pp.(2, 9,16,17,18)
Important considerations
In children older than 36 months (three years) the possibility of finding the focus of fever is greater because they cooperate more in the anamnesis and physical examination.
In the current pandemic context we should consider SARS-COV2 (COVID -19) infection as a probable cause in any patient with FSF and therefore test especially in unvaccinated patients or those wi th incomplete vaccination schedules.
The risk of occult bacteremia increases with increasing fever intensity. Most authors report that this risk is significantly higher if the patient's rectal temperature exceeds 39,5°C (axillary greater than 39°C) at any time. The response to antipyretic treatment or changes in the patient's clinical appearance after administration are not related to the risk of GBI, so they should not be taken into account in decision making. Regarding the site of measurement of body temperature, rectal temperature is preferable to axillary temperature; since, it correlates better with core temperature and most diagnostic-therapeutic algorithms are based on it.
The introduction of the pneumococcal conjugate vaccine (not present for the moment in our vaccination schedule) in recent years has produced a decrease in invasive disease due to S. pneumoniae, especially occult bacteremia due to vaccine serotypes. This fact has substantially modified the management of patients with FSF, and should therefore be a factor to be taken into account in its evaluation in countries where this vaccine is available.2,9,19,20
Clinical manifestations
Symptoms and signs will depend on the stage of evolution of the fever, which are:
Prodromal or Shivering Phase:
In this phase thermogenesis predominates, there is an imbalance between body temperature and the thermoregulatory center of the hypothalamus with predominance of the latter, manifesting as follows: shivering, shivering, piloerection, hyperesthesia, myalgia, arthralgia, pallor, cyanosis, lipothymia or dizziness.
Plateau or Crisis Phase
In this phase a balance is reached between thermogenesis and thermolysis, it manifests as follows: Flushing, increased heart rate, increased respiratory rate, thirst, headache, dry lips, delirium.
Defervescence phase
In this phase thermolysis predominates over thermogenesis, presenting the following symptoms: tachycardia, flushing, sweating, headache, tachypnea, constipation, dark urine, transmucosal burning, arterial hypotension.
Likewise, a series of symptoms that are part of the febrile syndrome but that do not depend directly on the thermoregulatory mechanisms but are mediated by the systemic effect of pyrogens may also present: drowsiness, nightmares, confusion, convulsive crises, cold sores, restlessness, anorexia, weight loss, photophobia, sonophobia.
In the evaluation of the child with FSF, a detailed anamnesis and physical examination should be performed; in some cases, it will be necessary to complete the evaluation with complementary explorations, since the clinical evaluation will not be sufficient to detect children at risk for IBG.2,8,9,13)
Alarm signs to be specified in an infant with fever in the emergency department:
Age less than three months.
Affectation of the general condition.
Convulsions.
Meningeal signs (older than 18 months).
Signs of neurological focalization.
Persistent vomiting and/or diarrhea.
No oral tolerance.
Tachypnea or Apnea.
Signs of respiratory distress: retractions, nasal flaring, whining (normal appearance + increased work of breathing).
Signs of respiratory failure (abnormal appearance + increased work of breathing).
Signs of tissue hypoperfusion: mottling of the skin, pallor, coldness, cyanosis, weak pulse, etc.
Generalized petechial rash.
Complementary examinations
Hemogram
Not generally recommended at baseline, except in <three months, vaccinated children with moderate-severe general condition, fever ≥40,5 °C, unvaccinated or immunocompromised.
Leukocytosis: It is the increase in the total leukocyte count. The most frequent leukocytoses are neutrophilic, followed by lymphocytosis.
Neutrophilia: A total neutrophil count above 10,000/mm3 after the neonatal period is most frequently associated with bacterial infection.2,9
Acute Phase Reactants (APR)
The most commonly used markers at present are C-reactive protein (CRP) and procalcitonin (PCT). The sensitivity of PCT is slightly higher than CRP in predicting IBG, but, above all, it is useful because it rises more rapidly. Both have more specificity than leukocytosis for detecting GBI, but lack sufficient sensitivity on their own or even in combination to rule it out, so it is necessary to put the value in the clinical context of the patient.2,9,13,21
The erythrocyte sedimentation rate (ESR) present in our environment should be less than 30 mm in the first hour. It is a slow marker that requires more than a week to reach its maximum value and its elevation can be maintained for a longer time than the infection itself. It is sensitive but non-specific. It can only be given value at large increments: 80-100 mm.22,23
- Blood culture
Extraction is recommended in case of suspicion of:
Bacterial meningitis.
Endocarditis.
Osteoarticular infection (arthritis/osteomyelitis).
Severe pneumonia.
Complicated pneumonia (necrotizing, abscess, pleural effusion, empyema, pneumatocele...).
IPPB: deep IPPB (pyomyositis, necrotizing fasciitis) and complicated superficial IPPB (secondary to trauma, surgical wound infection, ulcer, burn or bite, immersion wound, pericatheter, prosthetic material, need for surgery, extensive involvement, or suspected gangrenous ecthyma).
Urinary tract infection in infants < three months.
Infants < three months with any localized infection requiring admission.
Infections in immunocompromised and venous catheter carriers.
Consider removing in:
Infants aged three -36 months with FSF >39 ◦C and incomplete pneumococcal vaccination.
Routine removal is not recommended: infants > three months with FSF with adequate general condition and complete pneumococcal vaccination.2,24
- Urine culture
It is the initial test in most guidelines and algorithms, to rule out UTI as the most frequent bacterial cause of FSF, and it is more readily available and easy to perform. It is generally recommended: in girls under two years of age and children under one year of age, with fever ≥39 °C, in those with previous uropathies or nephropathies or in case of UTI lasting more than 48 hours, even if the fever peak is less than 39 °C.2,13,25
- Chest X-ray
Recommended in suspicion of occult pneumonia, with fever >39-40 °C (depending on the author) and leukocytosis ≥20 000/mm3.2
- Lumbar puncture
Indicate in children with altered PET and/or clinical or examination suggestive of meningitis or encephalitis, or in any infant younger than 3 months who does not meet low-risk criteria (this group would include infants <21 days).2,13,26
- Other microbiological tests
The polymerase chain reaction of pneumococcus and meningococcus or enterovirus in blood allows rapid results in non-invasive samples (respiratory, stool), the influenza or respiratory syncytial virus (RSV) test, especially in epidemic season, although they do not allow ruling out IBI, can avoid other more invasive tests in children at low and moderate risk.
Given the current circumstances, the performance of rapid tests for active SARS-CoV-2 infection should be taken into account especially in children without vaccination for COVID-19 or with incomplete vaccination schedule or severe acute respiratory symptoms and always remembering that a positive result neither rules out IBI nor should limit the study of FSF in those children who present alarm or risk data.
Likewise, any child with FSF with or without epidemiological link will be considered as a suspected case of dengue by performing a Dengue IGM on the 6th day of symptom onset or earlier if severity criteria as established in our country (repeated again if necessary).
Treatment
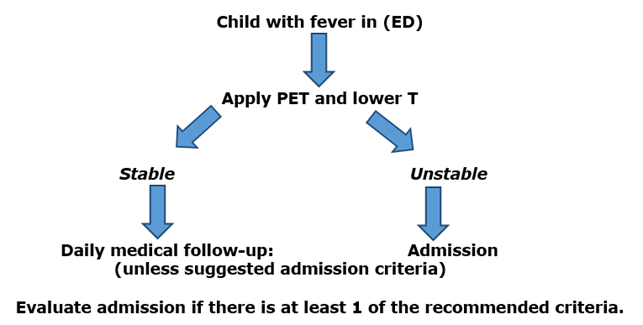
All patients should be evaluated in the Emergency Department (ED) with the PET tool and the flowchart recommended by the Guide for pediatric evaluation of emergencies in Cuba.26
Suggested criteria for the admission of a child with fever in the ED
Any febrile syndrome in the newborn.
Infants younger than three months with proven GBI.
Infants younger than three months with analytical alterations in the leukogram/urine examination or even without them and even if they present stable PTE.
Unstable PET (alteration of at least one side).
Presence of alarm signs in any system.
Infants and children of other ages: when the suspected cause requires assessment and/or hospital treatment.
All patients presenting with IBI.
Underlying chronic decompensated illness.
Anxiety and/or family concern.
Repeated attendance to health services without resolution of the reason for the child's consultation.
Poor family socio-economic conditions or impossibility of home observation: "unreliable parents".
Domicile far from the hospital or impossibility of rapid access to the hospital.
Cases under epidemiological surveillance or due to behaviors established in specific protocols (dengue, COVID-19).2,13
Any other criterion that in benefit of the child's health is decided by the attending physician for hospitalization is also considered valid.
Table 1 shows a comparison of the most commonly used antipyretic drugs in our environment.
Table 1 Antipyretic medications.
| Paracetamol | Dipyrone | Ibuprofen | |
|---|---|---|---|
| Therapeutic effect | analgesic Antipyretic | Antipyretic, analgesic | Antipyretic, analgesic, anti-inflammatory |
| Dosage | 10 -15 mg/kg/ Dose | 10 - 30 mg/kg/ Dose | 5 -10 mg/kg/ Dose |
| Intervals | Every 4, 4-6 hours, | Every 4, 4-8 hours, | Every 6, 6-8 hours, |
| Maximum dose | 60 - 90 mg/kg/day (4 g/24 h). | 40 mg/kg/day (4g/24h) | 40 mg/kg/day (2,4 g/24h) |
| Toxic dose | 150mg/kg in children and 6.5g in adults. | > 10g | > 100 mg/kg |
| Temperature drop: | 1-2ºC | No evidence of greater effect than other antipyretics. | 1-2ºC |
| Onset of effect | < 1 hour | 30-60 min (oral administration) Intramuscular route is fast (less than 30 min) < 1 hour | < 1 hour |
| Peak effect | 2-3 hours | 1 - 1,5 hours | 2-2,5 hours |
| Duration of effect | 4-6 hours | About 10 hours | 6-8 hours |
| Minimum age: | From birth | Under 3 months or 5 kg | From 6 months onwards |
To the question of when to combine antipyretics - joint administration of the two drugs - or alternate: the mechanism behind this recommendation is the synergy of both drugs, which have different mechanisms of action. In the studies, the combination or alternation is more effective when it comes to reducing the febrile peak. However, this fact is clinically irrelevant, since malaise, which is the main symptom to be treated, does not improve. Although no significant increase in undesirable effects has been found with the combination or alternation of antipyretics, there could be misunderstandings with the dosage (maximum dose, interval between doses). Therefore, and in general, combination or alternation is never recommended.26,27
Special care is recommended when administering any of them in patients with pre-existing chronic conditions, such as liver or kidney disease, diabetes, heart disease or severe malnutrition.13
Non-pharmacological measures
Warm cloths or baths are not routinely recommended as they may increase general discomfort. Excessive warmth should be avoided -but do not undress-, and liquids should be offered. There are studies that support the decrease in temperature even without antipyretics with adequate hydration of the patients.4,6,26
We recommend applying non-pharmacological measures based on our experience and the individual analysis of each patient. The scientific validity of each measure to be used should always be evaluated, followed or certain.
Antibiotic therapy
Some recommendations of the Latin American Consensus on sepsis:
Start antibiotic treatment as soon as possible, within the first three hours after diagnosis in pediatric patients with sepsis with organ dysfunction, but without shock data.
Initiate empirical broad-spectrum antibiotic treatment within the first hour of diagnosis in all cases of septic shock, basing the choice and dosage on local antimicrobial resistance patterns.
Obtain samples for blood culture (volume according to age and weight) and other sites according to the clinical suspicion of the infectious focus before starting antibiotic treatment.
Empirical antibiotic treatment should be broad-spectrum. It should be chosen based on local epidemiological data, age, host type (underlying diseases), invasive procedures, site of infection, history of previous antibiotic treatment and infection or colonization by multiresistant microorganisms.
Once the etiological agent has been confirmed, the definitive treatment will be adapted to the one with the lowest possible spectrum and toxicity, according to the type of infection, microorganism and confirmed sensitivity.3,13,28
Note:
It is important to be clear that these recommendations are not intended to replace individual clinical judgment in the care of children by the treating physicians, as the consensus itself establishes.
Flowchart of recommended actions for the febrile child in emergency (Fig. 1)
CONCLUSIONS
Fever is undoubtedly the most frequent cause requiring medical attention in children. Its study, therefore, is vital in current pediatric practice. It is necessary to perform a complete anamnesis and physical examination in order to determine the etiology of each acute febrile child in order to follow the most appropriate diagnostic and therapeutic path. Most infections will be self-limited viral infectious processes. It is recommended that this article be reviewed by students or physicians involved in pediatric care.
BIBLIOGRAPHIC REFERENCES
1. Consolini Deborah M. Fever in infants and children. MSD Manual. Thomas Jefferson University Hospital [Internet]. 2022 [citado 17/01/2022]. Disponible en: Disponible en: https://www.msdmanuals.com/home/children-s-health-issues/symptoms-in-infants-and-children/fever-in-infants-and-children 1. [ Links ]
2. García Soto L, Callejas Pozo JE. Fiebre: ¿cómo medir la temperatura?, ¿cuándo y cómo tratar la fiebre? Guía-ABE. Infecciones en Pediatría. Guía rápida para la selección del tratamiento antimicrobiano empírico [Internet]. 2022 [citado 17/01/2022]. Disponible en:Disponible en:https://www.guia-abe.es/anexos-fiebre-como-medir-la-temperatura-cuando-y-como-tratar-la-fiebre- 2. [ Links ]
3. Bruno M, Ellis A. Consenso para el uso adecuado de antibióticos en el niño menor de 36 meses con fiebre sin foco de infección evidente. Arch Argent Pediatr [Internet]. 2017[citado 17/01/2022]; 115(2): 27-37. Disponible en:Disponible en:http://dx.doi.org/10.5546/aap.2017.205 3. [ Links ]
4. José Pitoli P. Febreem crianças: procura de país por serviços médicos de emergencia. Ciência& Saúde Colet [Internet]. 2021 [citado 17/01/2022]; 26(2): 445-454. Disponible en: Disponible en: https://doi.org/10.1590/1413-81232021262.40782020 4. [ Links ]
5. Fernández-Cuesta Valcarce MA, Grande Tejada A, Morillo Gutiérrez B. Fiebre sin foco en el menor de 3 años (v.1/2018). Guía-ABE. Infecciones en Pediatría. Guía rápida para la selección del tratamiento antimicrobiano empírico [Internet]. 2018 [citado 07/01/2023]. Disponible en:Disponible en:https://www.guia-abe.es/temas-clinicos-fiebre-sin-foco-en-el-menor-de-3-anos 5. [ Links ]
6. Barros D. Febre aguda: orientações da Socieda de Brasileira de Pediatria [Internet]. 2021 [citado 05/01/2023]. Disponible en: Disponible en: https://pebmed.com.br/febre-aguda-orientacoes-da-sociedade-brasileira-de-pediatria/ 6. [ Links ]
7. Dorney K, Bachur RG. Febrile infant update. Curr Opin Pediatr [Internet]. 2017 Jun [citado 05/01/2023]; 29(3): 280-285. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/28323666/ 7. [ Links ]
8. Fever in under 5s: assessment and initial management. London: National Institute for Health and Care Excellence (NICE) [Internet]. 2021 Nov [citado 05/01/2023]; 143: Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK552086/ 8. [ Links ]
9. Udaondo C, López R. Fiebre. Síndrome febril agudo. En: Guerrero-Fernández J, Cartón Sánchez A, Barreda Bonis A, Menéndez Suso J, Ruiz Domínguez J (directores). Manual de Diagnóstico y Terapéutica en Pediatría [Internet]. 6ª. ed. Madrid: Editorial Médica Panamericana; 2018. p. 247-58. Disponible en: https://librosmedicospdf.com/book-manual-de-diagnostico-y-terapeutica-en-pediatria-libro-verde-6ta-edicion9. [ Links ]
10. Chiappini E, Bortone B,Galli L, et al. Guidelines for the symptomatic management of fever in children: systematic creview of the literatura and quality appraisal with AGREE II. BMJ Open [Internet]. 2017[citado 05/01/2023]; 7(7): e015404. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/28760789/ 10. [ Links ]
11. Mintegi Raso S, Gómez Cortés B. Lactante febril. Protoc diagn ter pediatr[Internet]. 2020[citado 05/01/2023]; 1: 141-151. Disponible en: Disponible en: https://www.aeped.es/sites/default/files/documentos/11_lactante_febril.pdf 11. [ Links ]
12. Barra G,et al. Síndrome febril sin foco y sospecha de infección bacteriana en niños entre 6 semanas y 36 meses. Rev Chi Pediatr [Internet]. 2008 [citado 05/01/2023]; 79(4): 388-392.Disponible en: Disponible en: https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0370-41062008000400006 12. [ Links ]
13. Barbi E, Marzuillo P, Neri E, Naviglio S, Krauss BS. Fever in children: Pearls and pitfalls. Children (Basel) [Internet]. 2017 [citado 17/01/2023]; 4(9): 81. Disponible en: Disponible en: https://www.mdpi.com/2227-9067/4/9/81 13. [ Links ]
14. Unger M, Karanikas G, Kerschbaumer A, Winkler S, Aletaha D. Fever of unknown origin (FUO) revised. Wien Klin Wochenschr [Internet]. 2016 [citado 17/01/2023]; 128(21): 796-801. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5104815/ 14. [ Links ]
15. Gómez B, Mintegi S. Fiebre sin foco. Pediatr Integral [Internet]. 2018 [citado 17/01/2023]; XXII(5): 211-218. Disponible en: Disponible en: https://www.pediatriaintegral.es/publicacion-2018-07/fiebre-sin-foco-2/ 15. [ Links ]
16. Lafolie J, Labbé A, L’Honneur AS, Madhi F, Pereira B, Decobert M, et al. Assessment of blood enterovirus PCR testing in paediatric populations with fever without source, sepsis-like disease, or suspected meningitis: a prospective, multicentre, observational cohortstudy. Lancet Infect Dis [Internet]. 2018[citado17/01/2023]; 18(12): 1385-96. Disponible: Disponible: https://pubmed.ncbi.nlm.nih.gov/30389482/ 16. [ Links ]
17. Han X, Yu H, Toledo-Romaní M. Vacunas antineumocócicas conjugadas: una revisión de las consideraciones éticas e impacto socio-económico. Revista Habanera de Ciencias Médicas [Internet]. 2021 [citado 09/01/2023]; 20(4). Disponible en: Disponible en: https://revhabanera.sld.cu/index.php/rhab/article/view/3867 17. [ Links ]
18. Martínez Osorio J, García García JJ, Moraga Llop F, Díaz A, Hernández S, Solé Ribalta A et al. Enfermedad neumocócica invasiva en niños menores de 60 meses, antes y después de la introducción de la vacuna conjugada 13-valente. Anales Pediatría [Internet]. 2022 [citado 09/01/2023]; 96(6): 501-510. Disponible en: Disponible en: https://doi.org/10.1016/j.anpedi.2021.05.018 18. [ Links ]
19. Greenhow TL, Hung Y, Herz A. Bacteremia in Children 3 to 36 Months Old After Introduction of Conjugated Pneumococcal Vaccines. Pediatrics [Internet]. 2017 [citado 09/01/2023]; 139(4): e20162098. Disponible en: Disponible en: https://doi.org/10.1542/peds.2016-2098 19. [ Links ]
20. Milcent K, Gajdos V. Use of Procalcitonin Assays to Predict Serious Bacterial Infection in Young Febrile Infants-Reply. JAMA Pediatr [Internet]. 2016 [citado 09/01/2023]; 170(6): 623-624. Disponible en:Disponible en:https://jamanetwork.com/journals/jamapediatrics/article-abstract/2513201 20. [ Links ]
21. Sanz F, et al. Sindrome Febril sin foco en pediatria. An Pedatri Contin [Internet]. 2009[citado 09/01/2023]; 7: 196 -204. Disponible en: Disponible en: https://www.elsevier.es/es-buscar?cmbBuscador=16962818&txtBuscador=Sindrome+Febril+en+pediatria 21. [ Links ]
22. García García S, Rubio Sánchez-Tirado M. Síndrome febril en el niño (I). Formación Médica [Internet]. 2007 [citado 10/09/2022]. Disponible en: Disponible en: http://2011.elmedicointeractivo.com/docs/documentos/fiebre.pdf 22. [ Links ]
23. Hernández Bou S, Álvarez Álvarez C, et al. Hemocultivos en urgencias pediátricas. Guía práctica de recomendaciones: indicaciones, técnica de extracción, procesamiento e interpretación. An Pediatr (Barc) [Internet]. 2016 [citado 10/11/2022]; 84(5): 294.e1-294.e9. Disponible en: Disponible en: https://www.enfermeriaaps.com/portal/wp-content/uploads/2016/05/Hemocultivos-en-urgencia-pediatrica.pdf 23. [ Links ]
24. Alperi García S, Martínez Suárez V. Infección del tracto urinario y reflujo vesicoureteral. Pediatr Integral [Internet]. 2022[citado 09/01/2023]; XXVI (8): 460-470. Disponible: Disponible: https://www.pediatriaintegral.es/wp-content/uploads/2022/xxvi08/01/n8-460-470_SAlperi-VMtnez.pdf 24. [ Links ]
25. Sánchez Cabrera YJ, López González L del R, Marquez Batista N. Guía de valoración pediátrica de urgencias en Cuba. Rev Cubana Pediatr [Internet]. 2022 [citado 18/01/2023]; 94(4): e2013. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S0034-75312022000400017 25. [ Links ]
26. Kliegman RM. Nelson Tratado de Pediatría 21ª ed. [Internet]; 2020 [citado 08/01/2023]. Disponible en: Disponible en: https://booksmedicos.org/nelson-tratado-de-pediatria-21a-edicion/ 26. [ Links ]
27. Trippella G, Ciarcià M, de Martino M, Chiappini E. Prescribing Controversies: AnUpdated Review and Meta-Analysison Combined/Alternating Use of Ibuprofen and Paracetamol in Febrile Children. Front Pediatr [Internet]. 2019 Jun [citado 08/01/2023]; 7: 217. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6560148/ 27. [ Links ]
28. Fernández Sarmiento J. Consenso Latinoamericano de manejo de sepsis en niños: TaskForce de la Sociedad Latinoamericana de Cuidados Intensivos Pediátricos (SLACIP). Acta Pediatr Mex [Internet]. 2022 [citado 08/01/2023]; 43 (1): 51-69. Disponible en: Disponible en: https://doi.org/10.18233/APM1No1pp%p2480 28. [ Links ]
Received: January 01, 2023; Accepted: April 24, 2023











 texto en
texto en