Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 supl.1 Pinar del Río 2023 Epub 01-Jul-2023
Articles
Human papillomavirus infection and oral squamous cell carcinoma: a systematic review
1Universidad Regional Autónoma de los Andes (UNIANDES). Ecuador
Introduction:
squamous cell carcinoma (SCC) is the most common cancer in the oral cavity, it represents 5 % of all neoplasms and occupies number 12 of all malignant neoplasms, there is a relationship between the cervix, oral cavity and oropharynx.
Objective:
to argue the relationship between human papillomavirus (HPV) infection and oral squamous cell carcinomas.
Methods:
a systematic literature review was performed, 60 articles indexed in (Pubmed, Scopus, Cochrane Library, Google Scholar and SciELO) were reviewed. Only bibliographic and systematic reviews with less than 10 years of publication, based on human studies, published in English or Spanish and with the text available were included. All those studies that did not meet these parameters were excluded, leaving a total of 16 results.
Development:
squamous cell carcinoma represents 90 % of malignant neoplasms of the oral cavity and oropharynx. There are several HPV types among them 201 types that differ due to variations in the L1 DNA sequence. The literature deduces that 17,8 % of all cancers are stimulated by contagious type agents and 12,1 % belong to viruses, this forces to inquire more about HPV as a carcinogenic agent and its contribution in squamous cell carcinoma (SCC) in oral cavity and oropharynx.
Conclusions:
the carcinogenic mechanisms used by HPV for cell transformation are through E6 and E7 proteins as responsible for the malignization process.
Key words: HUMAN PAPILLOMAVIRUS VIRUSES; MOUTH NEOPLASMS; OROPHARYNGEAL NEOPLASMS; CARCINOMA, SQUAMOUS CELL
INTRODUCTION
Squamous cell carcinoma is the most frequent cancer in the oral cavity, it represents 5 % of all neoplasms and occupies number 12 of all malignant neoplasms in the world.1) It develops in flat stratified epithelia and it is in the cervix where its study has become more relevant in recent years. It has been detected that there is a close relationship between the cervix, the oral cavity and the oropharynx since they share one of the main risk factors (HPV), which may be related to carcinogenesis because this tissue shares the same histological characteristics as the mucosa of the cervix.2
Oral squamous cell carcinoma can originate in any mucosal location, but the most frequently affected sites are the tongue and the floor of the mouth. Genetic factors, diet and viral agents may play a role, since tobacco and alcohol are well-established risk factors, and 15-20 % of patients who tend to develop OSCC do so even in the absence of these factors.3) The association of all these effects causes a synergy that triggers an important alteration in the oral mucosa. In addition, the type of diet is still a controversial etiological factor.1
There are several types of HPV among them we have 201 types that differ due to variations in the L1 DNA sequence. Most of the different HPV types affect the skin producing warts. Only a small group of approximately 25-30 types are sexually transmitted and can cause cancer. Clinically they are classified according to their risk of malignancy in the cervix, into high-risk HPV and low-risk HPV.4
Squamous cell carcinoma (SCC) accounts for 90 % of all malignant neoplasms occurring in the oral cavity and oropharynx. The most affected sex is male, associated with a higher consumption of tobacco and alcohol, both in frequency and quantity. A total of 389,650 cases of SCC were registered in 2000, of which 266,672 were located in the oral cavity and 122,978 in the oropharynx.
In 2008, there were 263,900 new cases and 128,000 deaths due to this cancer. SCC of the oral cavity and oropharynx accounts for 5 % of all cancers in men and 2 % in women. Furthermore, it is the eleventh most common cancer in the world, with a high incidence in countries such as India, Australia, France, Brazil and southern Africa. There is little information collected in Latin America with few specific studies, which provide little data regarding SCC and more in relation to HPV.5,6
There is certain scientific evidence that demonstrates the causal relationship of HPV on oral squamous cell carcinoma, its percentage of causality remains controversial in the different anatomical regions.4 Therefore, in the present study we seek to evaluate the relationship between HPV infection and oral squamous cell carcinomas, and to estimate the incidence of this infection in these patients.
The present research was carried out because of the need to deepen the knowledge about HPV and its relationship with squamous cell cancer, it is of great relevance to disseminate this type of information to professionals in order to detect early a possible cell metastasis.
METHODS
In this review, the main aspects relating human papillomavirus to oral squamous cell carcinoma are presented. Articles indexed in English (Pubmed, Scopus, Cochrane Library, Google Scholar) and Spanish (SciELO, Google Scholar) were reviewed, with the aim of providing the general dentist and specialist with updated research on this topic, both in terms of its incidence and the mechanisms of carcinogenic action of the virus.
The following keywords were used in English: HPV, Oral Cancer, Oropharyngeal Cancer, Squamous Cell Carcinoma, and in Spanish: HPV, Cáncer Oral, Cáncer Oropharyngeo, Cáncer Orofaríngeo, Carcinoma de Células Escamosas. A total of 60 articles were obtained. For the sole purpose of assessing the current state of the art, only bibliographic and systematic reviews with less than 10 years of publication, based on human studies, published in English or Spanish and with the text available were included. All those studies that did not meet these parameters were excluded, leaving a total of 16 results.
DEVELOPMENT
Human Papillomavirus (HPV)
Human papillomavirus (HPV) represents a family of small double-stranded DNA viruses that infect the stratified flat epithelium of the skin and mucous membranes. There are about 100 types of papillomaviruses that are capable of infecting humans, and with types that have a high oncogenic risk.7
In 1995 the International Agency for Research on Cancer (IARC) classified HPV types 16 and 18 as human carcinogens due to the presence of oncoproteins encoded in their DNA that deregulate the cell cycle.5
With type 16 being the most frequent (six cases), followed by genotypes 18 and 33 (eight samples each), 31 and 45 (two samples each) and 14 were low risk, with the most frequent types being six (10 cases) and 11 (eight cases).8
HPV 13-32-31-1 has a higher oral incidence; malignant lesions at oral level are: squamous cell carcinoma, erythroplasia, erythroleukoplasia and leukoplakia; in patients whose ages range from 30 to 70 years.9 The worldwide prevalence of HPV infection reaches 45,8 % in oropharynx and 24,2 % in oral cavity and HPV-16 is the most prevalent.5
A higher survival was detected in the group of patients under 55 years of age (p<0.05).10 Dental students should be aware of the importance of early detection of cancer, so it is very important that they become familiar with the risk factors and clinical manifestations for treatment. It is essential that health teams and especially dentists have updated information on HPV in order to thoroughly investigate the current situation of the virus in these carcinomas, since the main neoplasm associated with HPV is oropharyngeal cancer that occurs more and more frequently in young patients that have little or nothing to do with known predisposing factors such as alcohol or tobacco.11
In a study conducted with a total of 17 patients, the average age was 62,9 years with a range of 37 to 89 years, the prevalence of HPV obtained in patients with squamous cell carcinoma of the head and neck was 17,64 % (3/17). The biopsies positive for p16INK4 antibody corresponded to two men aged 53 and 89 years, and one woman aged 75 years, one of whom had a history of smoking and alcoholism, and the other two had an unknown history. The sites of the positive biopsies were two oral mucosa and one vocal cord.12
Carcinogenesis and HPV in the mouth
The viral oncoproteins involved in oncogenesis are E6 and E7, which cause cell immortalization.13 The E6 protein acts on the tumor factor p53, which affects cell apoptosis. In parallel, the E7 protein intervenes in the inactivation of retinoblastoma, which has the tumor suspensory activity (Graph 1).
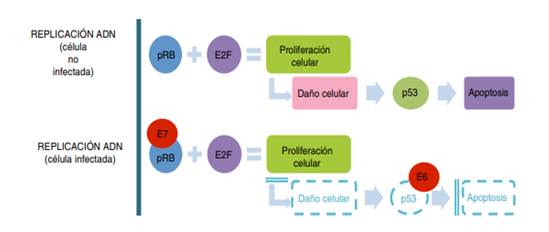
Graph 1 Comparative scheme between normal deoxyribonucleic acid (DNA) replication and the mechanism of human papillomavirus in the oncogenic process.14
HPV types in the oral cavity, especially, are of the non-oncogenic type. The HPV types that are considered unique to the mouth are: HPV 13-32. However, HPV 16-18 are mentioned to cause oral cancer. Benign and malignant HPV-induced lesions are represented in Table 1.
Table 1 Classification of oral lesions according to HPV genotype in the mouth
| Study | Oral injuries | Types of HPV that cause it |
|---|---|---|
| oral papilloma | 6-11 | |
| common wart | 4-6 | |
| Cháirez et al. (2015) | Condyloma acuminata | 11 |
| Focal Epithelial Hyperplasia With low incidence of malignant progression | 13-32 | |
| Leukoplakia and Carcinoma | 16-18-31-33-35 |
Note: HPV genotypes that cause lesions in the mouth are generally not carcinogenic, although there are lesions that can end in neoplastic processes.
In Ecuador, from 2006 to 2010, the prevalence of cancer was 8,423 cases per 100,000 people, which represents a rate of 34 and 43 cases per 100,000 inhabitants. In Ecuador there is no conclusive research on the incidence of oropharyngeal cancer associated with HPV. Research has been conducted between 2000 and 2019 in the main cities of Ecuador: Quito, Guayaquil and Cuenca. In addition, in the city of Ambato they conducted a study in the health sub-center, which included 99 patients older than 35 years, who were found to have potentially malignant lesions associated with HPV.
Malignant lesions were found in; eight patients with leukoplakia, four patients with erythroleukoplakia, and finally three patients with erythroplakia. While a study conducted on 108 healthy non-smoking patients in 2015 and 2016 in the city of Quito determined that HPV+ patients had microRNA predisposing to develop squamous cell carcinoma.
In the province of Manabí, there is not much statistical data on patients with malignant oral lesions produced by HPV. However, a study conducted at the pathology center of the San Gregorio University in Portoviejo, bulk samples of 37 HPV subtypes were analyzed in 2019. Resulting in 13 cases of patients with oropharyngeal or non-oropharyngeal head and neck cancer, between the ages of 13 to 68 years. Forty-six percent of the patients presented oncogenic HPV genotype; while in the remaining 54 % there was no presence of the virus DNA or it was not sufficiently detectable. The most common genotype was HPV11-31-61-71.9,15
There is one study showing a 28 % reduction in the risk of death and a 49 % reduction in the risk of disease recurrence for patients with HPV-positive OPC (oropharyngeal cancers) compared to those with HPV-negative OPC. Key biological differences that may explain this data are why HPV-related OPC responds better to treatment than non-HPV OPC: In cancers caused by HPV, the virus silences p53 but leaves the gene that produces it "intact"; by contrast, in HPV-negative cancers, the gene is mutated, probably through exposure to carcinogens such as tobacco or alcohol, and produces an "ineffective" version of the protein. Chemotherapy or RT can somehow reactivate p53 in HPV-positive cancers, re-activating the powerful tumor-fighting protein. Numerous studies have reported an inverse correlation between HPV DNA and p53 mutations.12,16
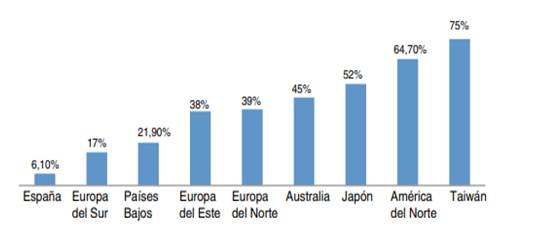
Graph 2 Geographic variations of human papillomavirus-associated oropharyngeal squamous cell carcinoma cases) between 2000 and 2015.14
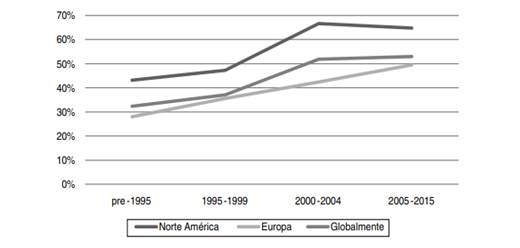
Graph 3 Epidemiological trends of human papillomavirus-associated squamous carcinomas of the oropharynx in North America, Europe and globally during the last two decades.14
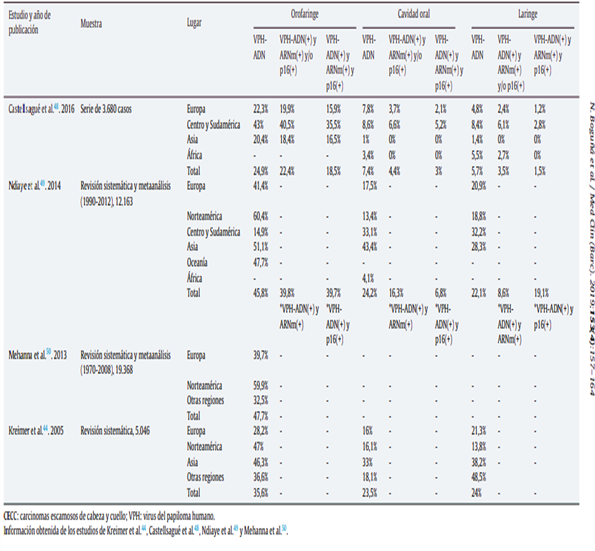
Table 2 Epidemiological data on head and neck squamous cell carcinomas attributable to human papillomavirus according to different studies, detection technique, geographic area and location of head and neck squamous cell carcinomas.11
The literature deduces that 17,8 % of all cancers are stimulated by contagious type agents and 12,1 % belong to viruses, this forces to inquire more about HPV as a carcinogenic agent and its contribution in squamous cell carcinoma (SCC) in the oral cavity and oropharynx.5
The carcinogenic mechanisms used by HPV for cell transformation are through E6 and E7 proteins as responsible for the malignization process. Once the viral DNA integrates with that of the host cell, the E2 protein of the virus (responsible for transcriptional regulation) is lost and as a result the E6 and E7 oncoproteins are overexpressed. These two proteins are synthesized with the aim of blocking checkpoints in the cell cycle, thus evading endogenous quiescence or apoptosis mechanisms that are carried out by tumor suppressor proteins (Graph 4).
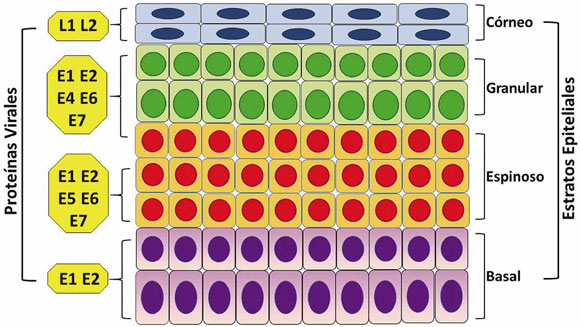
Graph 4 High-risk HPV proteins and corresponding site of action in the epithelium. Site of action in the stratified squamous epithelium.5
Epidemiology of oral and oropharyngeal SCC
Squamous cell carcinoma (SCC) accounts for 90 % of all malignant neoplasms in the oral cavity and oropharynx. The male sex is the most affected, which is associated with a higher consumption of alcohol and tobacco, both in frequency and quantity. In 2000, 389,650 cases of SCC were reported, of which 266,672 were located in the oral cavity and 122,978 in the oropharynx. In 2008, there were 263,900 new cases and 128,000 deaths due to this cancer. Oral cavity and oropharyngeal SCC accounts for 5 % of all cancers in men and 2 % in women.5
CONCLUSIONS
In the articles reviewed all agree that HPV is a highly contagious disease from oral sexual practices, this disease was associated with SCC (oral squamous cell cancer). Furthermore, that squamous cell carcinoma (SCC) comes to occupy the majority of all malignant neoplasms in the oral cavity and oropharynx, with the male sex being the most affected, associated with tobacco and alcohol consumption.
BIBLIOGRAPHIC REFERENCES
1. de la Fuente Hernández J, Muñoz Mújica P, Patrón Bolaños CE, Ramírez Trujillo M de los Á, Rojas Mercado HJ, Acosta Torres LS. Aumento de la incidencia de carcinoma oral de células escamosas. Salud ciencia (Impresa) [Internet]. 2014 [citado 21/11/2022]; 201. (6):1. 636-42. Disponible en: Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/lil-796464 1. [ Links ]
2. Contreras W, Venegas B. Virus Papiloma Humano en Cáncer Oral y Orofaríngeo: Revisión de la Literatura. International journal of odontostomatology [Internet]. Diciembre de 2015 [citado 11/11/2022]; 9(3): 427-35. Disponible en: Disponible en: http://www.scielo.cl/scielo.php?script=sci_abstract&pid=S0718-381X2015000300012&lng=es&nrm=iso&tlng=es 2. [ Links ]
3. Melo BA de C, Vilar LG, Oliveira NR de, Lima PO de, Pinheiro M de B, Domingueti CP, et al. Human papillomavirus infection and oral squamous cell carcinoma - a systematic review. Braz J Otorhinolaryngol [Internet]. 2021 [citado 13/11/2022]; 87(3): 346-52. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/33339760/ 3. [ Links ]
4. Ontañón AV, Losa JH, Haro RSL de, Paricio BB, Agüeras SRC, Atín SB, et al. Impacto del virus papiloma humano en pacientes afectos de carcinoma escamoso de cavidad oral y orofaringe. Medicina clínica [Internet]. 2019 [citado 11/10/2022]; 152(5): 174-80. Disponible en: Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=6805242 4. [ Links ]
5. Office of the Chief Dental Officer of Canada1. Human papillomavirus and oral health. Can Commun Dis Rep [Internet]. 5 de noviembre de 2020 [citado 11/11/2022]; 46(1112): 380-3. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/33447158/ 5. [ Links ]
6. Ding Y, Ma L, Shi L, Feng J, Liu W, Zhou Z. Papillary squamous cell carcinoma of the oral mucosa: a clinicopathologic and immunohistochemical study of 12 cases and literature review. Ann Diagn Pathol [Internet]. Febrero de 2013 [citado 13/11/2022]; 17(1): 18-21. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/22672806/ 6. [ Links ]
7. Howard A, Agrawal N, Gooi Z. Lip and Oral Cavity Squamous Cell Carcinoma. Hematol Oncol Clin North Am [Internet]. Octubre de 2021 [citado 11/11/2022]; 35(5): 895-911. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/34274176/ 7. [ Links ]
8. Medina MG, Marinic K, Medina ML, Sorrentino A, Giménez MF, Merino LA. Detección de papilomavirus humano en mucosa oral en hombres con verrugas anogenitales. Memorias del Instituto de Investigaciones en Ciencias de la Salud [Internet]. Agosto de 2021 [citado 10/11/2022]; 19(2): 41-8. Disponible en: Disponible en: http://scielo.iics.una.py/scielo.php?script=sci_abstract&pid=S1812-95282021000200041&lng=en&nrm=iso&tlng=es 8. [ Links ]
9. Mendoza WAV, Robles JLM. Virus del Papiloma Humano y su relación con el cáncer orofaríngeo. Revista San Gregorio [Internet]. 31 de diciembre de 2021 [citado 12/11/2022]; (48): 123-48. Disponible en: Disponible en: https://revista.sangregorio.edu.ec/index.php/REVISTASANGREGORIO/article/view/1771 9. [ Links ]
10. Maraboli-Contreras S, Adorno-Farías D, Maturana-Ramírez A, Rojas-Alcayaga G, Fuentes-Alburquenque M, Espinoza-Santander I, et al. Sobrevida de carcinoma oral de células escamosas: reporte de la Universidad de Chile. Revista clínica de periodoncia, implantología y rehabilitación oral [Internet]. Diciembre de 2018 [citado 12/11/2022]; 11(3): 147-51. Disponible en: Disponible en: http://www.scielo.cl/scielo.php?script=sci_abstract&pid=S0719-01072018000300147&lng=es&nrm=iso&tlng=es 10. [ Links ]
11. Verano Gómez NC, Escobar Urcuango A, Romero Fernández AJ, Verano Gómez NC, Escobar Urcuango A, Romero Fernández AJ. Conocimientos de los estudiantes de odontología sobre el virus del papiloma humano asociado al cáncer orofaríngeo. Conrado [Internet]. Octubre de 2021 [citado 12/11/2022]; 17(82): 240-8. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S1990-86442021000500240&lng=es&nrm=iso&tlng=es 11. [ Links ]
12. Valdez-Flores AI, Garnica-Núñez C, Urías-Barreras CM, Rafael E, Batiz-Salazar DM. Virus del papiloma humano en carcinoma de células escamosas de cabeza y cuello. Rev Med UAS [Internet]. 2016 [citado 10/11/2022]; 6(3). Disponible en: Disponible en: https://hospital.uas.edu.mx/patologia/Articulos/14.pdf 12. [ Links ]
13. de Abreu PM, Có ACG, Azevedo PL, do Valle IB, de Oliveira KG, Gouvea SA, et al. Frequency of HPV in oral cavity squamous cell carcinoma. BMC Cancer [Internet]. 27 de marzo de 2018 [citado 12/11/2022]; 18(1): 324. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/29580212/ 13. [ Links ]
14. Boguñá N, Capdevila L, Jané-Salas E. Relationship of human papillomavirus with diseases of the oral cavity. Med Clin (Barc) [Internet]. 16 de agosto de 2019 [citado 10/11/2022]; 153(4): 157-64. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/31109717/ 14. [ Links ]
15. Johanning Cordero JC. Carcinoma escamoso de cavidad oral y orofaringe asociado a virus del papiloma humano: características epidemiológicas, histopatológicas y la importancia de las pruebas inmunohistoquímicas y moleculares en su diagnóstico [Internet]. Universidad de Costa Rica, San José, Costa Rica; 2020 [citado 30/12/2022]. Disponible en: Disponible en: https://kerwa.ucr.ac.cr/handle/10669/82332 15. [ Links ]
16. Berman TA, Schiller JT. Human papillomavirus in cervical cancer and oropharyngeal cancer: One cause, two diseases. Cáncer [Internet]. 15 de junio de 2017 [citado 12/11/2022]; 123(12): 2219-29. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/28346680/ 16. [ Links ]
Received: April 28, 2023; Accepted: April 29, 2023











 texto en
texto en 


