Introduction
The articular hypermobility and its clinical manifestations that give rise to Articular Hypermobility Syndrome is one of the most frequent conditions in the medical consultation of Rheumatology (Martínez, et al., 2013). These patients present daily painful manifestations of the osteomioarticular system and orthopedic deformities, limiting the performance of their daily activities associated with a Hypermobility Spectrum Disorders.
When talking about hypermobility and hyperlaxity refers to the range of joint movements not considered normal for the functionality of the joint (Rodríguez, 2017). The lax joints cause an increase in tension in the adjacent soft tissues (muscles, ligaments, tendons) that stabilize them.
The Hypermobility Spectrum Disorders (HSD) are a group of diseases related to joint hypermobility and are distinguished from all other hypermobile syndromes because their scope is almost exclusively limited to the musculoskeletal system (Castori, et al., 2017).
Hypermobility Spectrum Disorders Localized (L-HSD): at single joints or group of joints plus one or more secondary musculoskeletal manifestations regionally related to the hypermobile joint(s) (Castori, et al., 2017).
HSD patients with frequencies have muscle weakness in the lumbar area due to lordosis in the lower back and resistance to muscular force in that area is affected. For this reason, resistance to muscular strength is one of the qualities of the trunk musculature that has aroused greater interest on the part of the physiotherapists, being primordial strengthen the lumbo-pelvic core muscle to facilitate stabilizing and motor control work for the individual.
The term Core etymologically means core, center or middle zone. Taking this concept as a basis, the term core stability arises, which has raised great interest in the last 20 years in different fitness, sport, research and injury prevention and rehabilitation fields (Wirth, et al., 2017, cited by López, 2017).
The stability of the Core system, which is nothing more than the capacity of the osseousarticulate and muscular structures, coordinated by the motor control system, to maintain or resume a position or trajectory of the trunk, when it is subjected to internal or external forces (Vera, et al., 2015). The joint action of these structures allows an adequate control of the body stability and the execution of tasks performed by the upper and lower limbs, in a combined or sequential way, enabling the body to adopt a stabilizing posture dominated by the Core muscles.
There are differences between physiotherapists, physical rehabilitators and Graduates in Physical Culture who carry out the rehabilitation work, and in turn, due to the scarcity in the development and implementation of physical exercise programs, training systems, methodological orientations of physical exercise aimed at these patients , both at a national and international level, on how to establish the density component - rest interval (RI) and recovery time (RT) - when planning the load during physical rehabilitation in this type of population spectrum. When prescribing physical exercises should pay attention to the components of dosage: volume, intensity, methodology, frequency, density and selection of exercises; integration enables favorable adaptive responses in patients to planned stimuli (Rodríguez, et al., 2017).
The importance of the density component was reflected in this study, which plays a decisive role in the planning of physical exercises. As Heredia, et al. (2012), the density should always be accompanied by the intensity of the stimulus (load to be dosed) and vice versa, so that the definition and relationship between the two allowed inferring possible responses and effects during the session (for example, rehabilitation class), in this feeling the density is nothing more than the RI and RT. Thus, the character of the density is conditioned by the replacement potentialities of the energy substrates involved in the stimulus, which represents the work-rest relationship, given by the RI and RT pause itself between the series (Rodríguez, 2017).
The dosage of shorter breaks (15 seconds to 30 seconds) will influence the organism to achieve adaptations in all osseous muscle articulate structures, since according to studies by (Kramer, 1987, cited by Del Castillo, 2014), they based the increase in density capillary and mitochondrial favors the patient to circulate a greater and better amount of blood through the capillaries, recovery will be faster with moderate and intense efforts, the ability to attenuate hydrogen and its transport out of the muscle is improved, a healthy benefit in the structures, their functions and better development of the patient before the activities of daily life.
Guaranteeing recovery pauses between 1 minute to 2 minutes ensures the completion of repetitions, series and work with the appropriate intensity, as well as an optimal recovery of the patient, providing them with favorable adaptive responses thanks to the increase in the total volume of repetitions performed in an exercise and to the muscular development achieved (Rodríguez, et al., 2017).
Rest times greater than> 2 minutes should be established according to the type of exercise and muscle group to which it is directed, to the individual characteristics of the patients. For this reason, it is recommended to promote longer rest periods when planning loads for large muscle groups and in which several joints are involved and shorter rest periods for small muscles and involving one joint (Rodríguez, et al., 2017).
Materials and methods
A descriptive, pre-experimental minimum control investigation was performed for a single group with pre-test post-test. The study followed the recommendations of the Declaration of Helsinki and was approved by the Scientific Council of the University of Sciences of the Physical Culture and Sport “Manuel Fajardo”.
The selected sample consisted of 10 young men, five of the female sexes and five of the males with musculoskeletal complaints in the lumbar zone as a result of a marked lumbar lordosis and Beigthon Score (SB) of 7 points out of 9, hypermobility in the joints of the elbows, knees and phalanges or the fingers being classified with an L-HSD, data contributed by the clinical histories of the patients, with an average age of 17 years. Prior to the initiation of the investigation the participants were informed of the characteristics of the study and gave their approval with their informed consent to participate in the research.
They underwent a comprehensive rehabilitation treatment through the action of physical-therapeutic exercises for 3 months. The content was directed to the development of resistance to the muscular strength of the Core. The training sessions counted 45 minutes, 5 times a week in the hours of 8:30-9:15 am in the Center of Studies for Physical Activity, Sport and Health Promotion of the University of Sciences of Physical Culture and Sport “Manuel Fajardo”. Pain was evaluated using the Visual Analogue Scale (VAS) and the muscular strength resistance of the Core with the Isometric Prono Bridge (PP) test respecting the procedures described by Ambegaonkar, et al. (2016).
The measurements made in the pre-test and post-test:
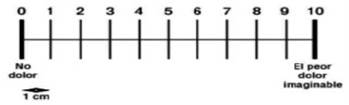
Visual Analogue Scale (VAS): the patient is instructed to represent the intensity of pain perception in a line of 10 cm. At one end is the phrase “no pain” indicating the number 0 and at the opposite end is the phrase “the worst pain imaginable” indicated by the number 10. The distance in centimeters from the point of “no pain” to The one marked by the patient represents the intensity of the pain (Fig. 1).
A value less than or equal to 3.9 means mild pain
A value between 4 and 5.9 means moderate pain
A value between 6 and 7.9 means severe pain
A value between 8 and 9.9 means severe pain
A value of 10 means very severe pain
The adolescents' perceived exertion was measured for the dosed load using the Scale for the measurement of infant perceived exertion (EPInfant) by Rodríguez & Manterola (2016), that they affirm “it is an instrument developed to quantify general perceived exertion in the child population” (p.31) children and adolescents under 18 years of age during physical exercise.
It was explained to the adolescents, for an adequate instrument measurement, they had to answer the following question: how tired do you feel during exercise? The question should be aimed at assessing the perception of global body effort, including leg fatigue and dyspnea.
Here is an example of an appropriate instruction proposed by Rodríguez & Manterola (2016):
Before, during and after exercise, I will ask you how tired you are.
You must use numbers, words or children to indicate your level of fatigue during the activity.
Observe the child at the beginning of the scale, if you feel like him, it means that you are not tired.
Observe the children located in the center of the scale (levels 5 and 6); If you feel like them, it is because you are tired, but you can continue doing the exercise.
Observe the child placed at the end of the scale; If you feel like him, it means that you are very tired and cannot continue exercising.
You can use any of the numbers, phrases, or pictures of children on the scale to tell me how tired you feel. There is no right or wrong answer.
Isometric Prono Bridge (PP) test to assess resistance to muscular strength of the Core and Lumbar Zone: the subject must maintain his body weight exclusively on the forearms and elbows and toes in a prone position, Maintaining at all times a neutral lumbo-pelvic (Core) alignment. The arms should be perpendicular to the floor and forming a 90º angle with the forearms. Elbows and forearms separated by shoulder width (Figure 2). The conclusion of the test happens when the subject loses the neutral positioning of the pelvis and it falls to the ground, acquiring a lumbar hyperlordosis by anterior rotation of the pelvis suggest that the time that the subjects evaluated should be supported by at least 60 seconds.
HSD patients performed the following system of physical-therapeutic exercises with the dosage:
Hip flexion: the subject is lying supine. Perform a hip flexion until reaching the position of 900 in correspondence to the hip, patellofemoral and ankle joints (Fig. 3).
2.
Dorsal bridge: The subject is lying supine, supporting the hands and feet on the mat, with the trunk completely straight with its posterior muscle chain (lower limbs and spine extended). The hands were placed with an approximate separation of the width of the shoulders and the feet together (Fig. 4).
Ventral flexion with knee flexion without weight: the subject is in a standing position to perform a ventral flexion of the trunk (forward) with the back as straight as possible until there is contraction in the lumbar muscles (Fig. 5).
1st month (1st and 2nd week: 4 sets of 7 to 10 repetitions, 30s of rest between sets) (3rd and 4th week: 4 sets of 12 to 15 repetitions, 30s of rest between sets)
2 month (1st and 2nd week: 5 sets of 10 to 12 repetitions, 40s of rest between sets) (3rd and 4th week: 5 sets of 12 to 15 repetitions, 40 s of rest between sets)
3rd month (1st and 2nd week: 5 sets of 15 to 17 repetitions, 60s of rest between sets) (3rd and 4th week: 5 sets of 17 to 20 repetitions with 60s of rest between sets)
The training system considers the following principles cited by Rodríguez (2017):
Accessibility Principle: loading requirements of easy accessibility were planned for patients, always respecting their potential to dose work from the simple to the complex, from the known to the unknown, and from the easy to the difficult.
Principle of Active and Conscious Participation in Training: the selected physical-therapeutic exercises allow patients to be able to function adequately; they knew the task to be carried out and were consciously familiar with what they are doing, how they are doing it and what they are doing it for.
Charge Versatility Principle: the dosed charge is prescribed from global or analytical practice; variable or constant; guided or free; with slight degrees of fatigue or without fatigue, varying the intensity and its prescription, complying with the adaptation to it by the patients.
Principle of affordability and individualization: it is explained to patients that the planned activity requires that the teaching be understandable and possible according to their individual characteristics, it is based on the optimal correspondence of the tasks, on the means and methods applied and on proper handling of the dosage of the load. This principle requires the observation of the physiotherapist to the possibilities of the patients to avoid methodological errors arising, since the demands must correspond to the capacities of the patients in order to achieve later development. On the basis of this principle, the scientific level of the physical rehabilitation process and the individual learning of each patient are determined.
Principle of systematicity: it is conceived by the systemic nature in the planning of physical-therapeutic exercises, where the physiotherapist takes into account the system approach, that is, it requires a system of the integral physical rehabilitation process, its continuity and the optimal alternation of loads with rest in the same rehabilitation session.
Principle of dynamic and gradual increase in demands: in the process of comprehensive physical rehabilitation it is necessary to constantly renew tasks, increase their difficulty, gradually increase the volume and intensity of loads to ensure the elevation of functional variations in the body, and on this basis continue the development of conditional and coordinative capacities, it is necessary to systematically renew the load, increasing its volume and intensity. This principle depends on the one hand on the magnitude and the qualitative characteristics of the load, and on the other on the individual adaptation possibilities. Dosing the loads upwards and on the parameters and possible limits of each patient allows you to achieve urgent adaptations, in the medium and long term.
Promote active participation: the physiotherapist, through her professional and pedagogical skills, provides the patient with verbal actions to encourage her motivation and participate in the activity in a leading way, facilitating her to start the exercises by herself to a lesser or greater degree and her development before the planned tasks are profitable and satisfactory.
Repeat the exercises without variation and with it: it is based on the fact that the nervous system has a great capacity to get used to or adapt to repetitive activity and especially when it may seem useless. Treatment sessions will never be exactly the same, making quantitative and qualitative variations to the activities according to the development of each patient, preventing the possibilities of adaptation and avoiding routine activity. In this principle, the appropriate selection of exercises and their dosage plays a preponderant role.
Achieve that the usefulness of the activity is understood: it is decisive, patients achieve the expected results to the extent that they understand the benefits of the planned physical-therapeutic exercise system, are actively inserted in the process, see their progress and development, their quality of life improves and the different activities of daily life are useful before.
Achieve full motivation of the patient: good development during the rehabilitation process is achieved to the extent that the patient feels motivated; the physiotherapist is responsible for providing support to achieve full motivation and integrate into physical-therapeutic exercises.
The non-parametric Friedman analysis of variance test was used by ranges (k related samples) multiple comparisons by pairs of variables (pre-test and post-test) that calculates the degree of significance at (p=0.05) of the changes that occur between the measurement moments for the variables Socore of Beighton, Visual Analog Scale of Pain and Prone Bridge.
The T test of samples related to the variables training loads and perceived effort was applied to statistically know the association between both for decision making, we established two statistical hypotheses:
Ho: The variable training load and perceived effort in hypermobile patients present a strong association.
Ha: The variable training load and perceived effort do not present a strong association because they differ in some hypermobile patients.
Results and discussion
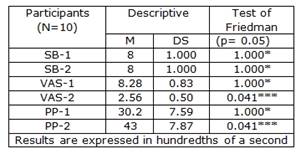
Table 1 presents the results between the pretest-1 and osttest-2 measurement moments. The descriptive statistics showed low results in the pretest in the indicators evaluated. The SB did not change and showed no significant levels (p=1.000), which means that the patients’ hyperlaxity did not change during the rehabilitation treatment, being similar to those found by Verity, et al. (2013).
This is not the case for the pain test which decreased significantly, showing significant changes (p=0.043). The Prono Bridge Isometric Test showed improvements in the time variable being significant (p=0.043).
Legend: SB: Beighton Score. VAS: Visual Analog Scale. PP: Isometric Test Prono Bridge to assess resistance to core muscle strength and Lumbar Zone. M: Mean. DS: Standard deviation. *** Significant changes * Not significant changes. Valuable time acceptable 60s for the PP test.
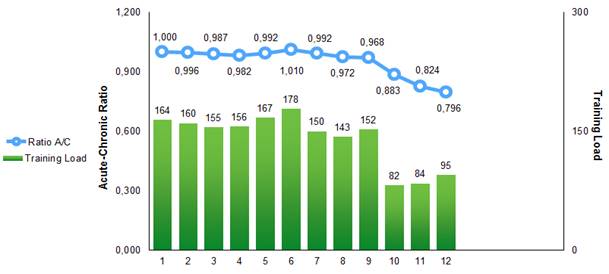 Leyend: Ratio A/C: Ratio Acute/Chronic
Leyend: Ratio A/C: Ratio Acute/ChronicFig. 6 - Control of training load and risk of injury Ratio Acute-Chronic
Chronic training load is analogous to a state of fitness and acute training load is analogous to a state of fatigue, in this sense it is important to use the terms chronic workload for long periods of time and acute workload for immediate periods (Gabbett, 2016).
Regarding the acute/chronic burden ratio, as the name suggests, the ratio describes the average between acute and chronic burden. Acute and chronic loads can have various positive and negative influences on the risk of injury in athletes, systematic practitioners of physical activity and in patients who undergo comprehensive physical rehabilitation using physical exercise as a determining way to improve their health. Various authors indicate that, if the chronic training load is high and the acute load is low, the athlete will be well prepared for competition. On the other hand, if the acute load exceeds the chronic one, the player will be poorly prepared, increasing the risk of injury (Gabett, 2016).
To minimize the risk of injury, patients should maintain the acute-chronic work ratio in an approximate range of 0.8-1.3 sweet spot. However, if the workload ratio exceeds the 1.5 danger zone, the risk of injury will increase (Gabett, 2016).
Figure 6. Provides us the Control of the training load and the risk of injuries Acute-Chronic Ratio in hypermobile patients during the 3 months of treatments. A varied and wavy behavior of the training load is observed in the different physical rehabilitation sessions per weeks. The control made it possible to adjust the load taking into account the potentialities of the patients and allowed them to cope adequately with the selected exercises.
The total volumes of the weekly load range from 178 to 82 repetitions with an acute/chronic ratio of 0.82-1.01, the risk of injury to patients being minimal, the acute/chronic ratio is at the right point 0.8-1.3. It should be noted that it is the first study that controls the training load and the risk of injury in patients with musculoskeletal disorders in the lumbar area, lumbar lordosis and Localized Hypermobility Spectrum Disorders.
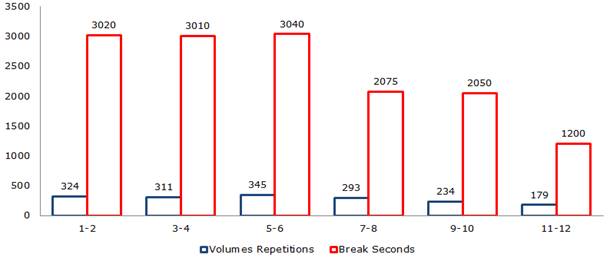
During the 3 months of rehabilitation, the patients underwent stimuli of considerable volumes with a wavy character in the dosage, allowing them to generate positive responses to physical-therapeutic exercises. An example of this is evidenced by figure 7, the volumes of loads during the first month were 635 repetitions for 48 series with 6030 seconds of recovery, at the end of the month the patients reported feeling comfortable and at ease with the planning. In the second month, the volumes for the four weeks were 638 repetitions for 60 series with 5115 seconds of recovery, in this period the patients performed 8 repetitions for 12 series and 915 seconds more than in the previous month.
It should be noted how decisive the dosage was in planning the organization of the loads in weeks 7 and 8, the volumes decreased compared to weeks 3 and 4 (as they were weeks of the second cycle of the month) in 18 repetitions with 935 seconds of recovery, those 18 repetitions of less that the patients performed allowed them to achieve neuromuscular and functional recovery to be able to assimilate the loads in the following weeks and continue with the adaptations achieved.
In these patients, it is essential to ensure that they achieve full recovery at the planned loads and do not incur phases of fatigue, since it is detrimental to their health. The established dosing system was based on providing unloading periods, the patients performed the activity but with less volumes of dosed loads. The unloading period was conceived from week 7 to 12; the patients assimilated better the performance of physical-therapeutic exercises, without the manifestation of symptoms and signs of fatigue, musculoskeletal ailments and arthralgias. In the third month, the dosed volumes were 413 repetitions for 60 series with 3250 seconds of recovery to conclude the period of unloading and physical rehabilitation.
The training system with its dosage enabled patients to develop empathy, socialize with their partner and acquire adequate technical skills to perform physical-therapeutic exercises and resistance capacity to muscular strength in the SOMA, in the lumbo-pelvic region and in the Core area.
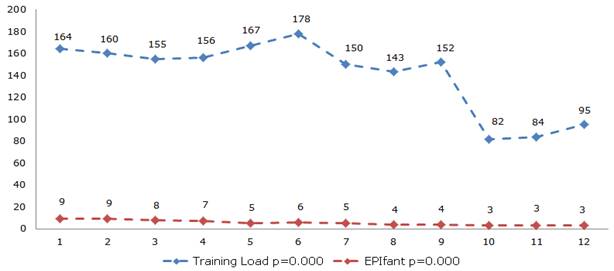 Legend: EPIfant: scale for measuring perceived exertion, results are expressed in points. The results of the volumes are expressed in repetitions. The confidence interval was 95%
Legend: EPIfant: scale for measuring perceived exertion, results are expressed in points. The results of the volumes are expressed in repetitions. The confidence interval was 95%Fig. 8 - Control of the subjective perception of effort in correspondence to the volumes of loads dosed per week.
The perceived effort at the loads dosed during the 12 weeks was evaluated through the EPIfant, obtaining a direct and proportional relationship to the established volumes. Figure 8 shows how the trend in patients in the first two weeks is linear and rises, not decreases, this is due to the fact that there are still no signs of adaptation to load and effort. From week three is where the patients showed adaptive traits to the dosage and the perceived effort tends to decrease as their body gets used to the stress caused by the volumes of repetitions performed.
At the end of week 6 with the highest volume planned, the patients perceive an effort at the load of 6 points, a notable decrease compared to those of the previous weeks and leads us to think that between weeks four and six is where patients they achieve the best development of resistance to muscular strength with a notable decrease in the subjective perception of effort. From week 7 to 12, as the volumes of the load decreased, the perception of perceived effort was lower, being very significant (p = 0.000)
The results of the Friedman test (p=0.05) for all variables indicate that not all the results at the moments of measurement are the same and the results of the posttest report that the action of the physical-therapeutic exercises and their dosage during The 3 months led to positive adaptive responses to the load by the evaluated subjects. This confirms lumbar zone pain relief between measurements. VAS1 was 8.28 DS ± 0.83 and VAS2 was 2.56 SD ± 0.50 for (p=0.043) being significant. The resistance to the muscular force of the Core behaved with improvements between the measurements.
The results of PP-1 were 30.2s SD ± 7.59 and PP-2 43s SD ± 7.87 (p=0.043) are congruent and significant. These results show that although there were improvements in the time of supporting the force of gravity for a static position where the muscular force exerts its action by means of an isometric contraction in all the stabilizing muscles of the posterior chain of the trunk involved before the planned task the results do not Reached the 60s.
Notwithstanding the 12.8s reached more, they judge that the lumbo-pelvic muscles were strengthened and managed to resist better isometric loads for longer periods of time, the results coincide with those obtained by Vera, et al. (2015); Rodríguez, et al. (2017); and Rodríguez (2017), in their study. It is considered appropriate to continue working with exercises that activate all the Core muscles to continue improving the results achieved.
The planned stimuli induce relief of musculoskeletal ailments in the lumbar area and improve the stability of the lumbar spine in hypermobile patients, adapting to the demands of physical-therapeutic exercises. Manipulating the intensity, volume, density and frequency of training generally conditions the organism to produce an urgent adaptive response of its somatic, physiological, endocrine and functional structures and with it an improvement in performance, benefiting them to be more functional in the daily life activities.
There are studies that relate to the manipulation of the ID between sets and (Rodríguez, et al., 2017) there have been rest of no less than 1 to 1.5 minutes fir small muscle groups (upper body segments) and 2 to 3 minutes for large muscle groups (lower body segments). If few attempts are made the ID are scheduled in 10, 15 and 20 seconds. The available literature suggests that periods of 1 minute should be sufficient to allow adequate recovery between sets. Recovery times and ID are self-regulating depending on the potentialities and individual characteristics of the patients.
Previous research has shown an increase in core muscle activation while increasing endurance and torque (Saeterbakken, et al., 2015). Therefore, it can be speculated that an adequate manipulation of the load (isometric contraction time and / or repetitions performed) in correspondence with a low subjective perception of pain and the effort perceived by the patient are determining elements for the body to generate adaptive responses urgent and efficient when faced with posture in stability exercises.
The present study has the limitation of not establishing an adequate verification of the results obtained with the results of studies in populations and similar intervention protocols, since no scientific evidence was found that prescribes physical exercise for the stabilizing muscles of the lumbar spine with variations in Dosing of RI and RT between series in adolescent patients with musculoskeletal pain and Localized Hypermobility Spectrum Disorder.
In a general, the prescribed physical-therapeutic exercises allowed practitioners that the perception of pain was less intense and more bearable as they performed the oriented task more freely without complaining about pain.
Conclusions
The study variables determined the importance in the dosage of physical-therapeutic exercises, considering the individual characteristics of the patients.
Physical-therapeutic exercises can be valued as an alternative for the relief of musculoskeletal ailments in the lumbar area, in the Core and significantly improves resistance to muscular force in the affected area of hypermobile patients.
The authenticity of the results obtained to establish an adequate biological, morphological and functional response of the patients to the planned physical loads, the harmonic and adequate integration of the dose components (volume, intensity, methodology, frequency, density and selection of exercises).
The isometric prone bridge test generates the activation of the core musculature activating the lumbar and paravertebral area, influencing the development of resistance to muscular strength at low or moderate intensity and can be used as an exercise to improve the stabilization capacity of the spine and gain resistance to muscular strength.
With a view to promoting quality of life and promoting favorable adaptive responses in patients, it is necessary to estimate recovery times that affect complete recovery and rest pauses between series that they can assimilate.