Introduction
The outcome of different implant procedures depends on several variables including patient characteristics, surgical technique, implant stability, and implant design.1 Implant stability is defined as the absence of movement at the moment of measurement.1 This factor can be measured at the moment of implant placement (primary stability) or once the osseointegration process is in progress (secondary stability).2 Primary stability includes the mechanical attachment of an implant in the surrounding bone at the insertion, whereas secondary implant stability is the tissue response to the implant and subsequent bone remodeling processes.2 Some researchers2,3 have reported that early failure may be caused by poor implant stability, thus, primary and secondary implant stability are considered key factors for treatment success.
Several methods have been used to examine implant stability at insertion and during the osseointegration period.1,3 Despite the availability of a wide variety of stability quantifiers, only some of these have been validated. Currently, insertion torque and resonance frequency analysis (RFA) are seen as the gold standard for evaluating in vivo implant primary stability.4 Insertion torque is a mechanical parameter influenced by surgical procedure, implant design and bone quality. A high insertion torque means that the implant is firmly embedded in the bone and mechanically stable. Some authors3 have found that insertion torque values above 32 Ncm are an indication of adequate primary stability.
RFA is a method used to determine implant stability (level of osseointegration), it consists on sending magnetic pulses to a small metal rod temporarily attached to the implant. As the rod vibrates, the probe reads its resonance frequency and translates it into an ISQ value.5 The value produced is a combination of bone implant contact and bone density around the implants.5 RFA instruments perform a quick and simple measurement, which results are presented within a parameter called implant stability quotient (ISQ). The ISQ ranges from 1 (low stability) to 100 (high stability).5,6 It has been reported that ISQ values at implant insertion should be ≥ 60 to achieve sufficient implant stability.6
RFA measurements are used to assess the implant stability immediately after placement, as well as to measure the stability during the healing time.6,7 This helps the dentist determine if more healing time (osseointegration) is needed before the placement of the prosthetic tooth, as well as to identify patients with compromised bone tissue, or other risk factors.7
Primary implant stability is influenced by many factors including local bone quality and quantity, and implant macro-design. In this context, there is some controversy about which implant design achieves better implant stability.8,9 Implant macro- design plays a fundamental role in maintaining stability.10 Although many modifications have been developed over the years, most manufacturers still use two main implant macro- designs, tapered and cylindrical. Tapered implants have been shown to provide higher primary stability than cylindrical implants in many clinical and in vitro studies.11,12,13 Despite their advantageous stability, the use of tapered implants in the posterior mandible is usually not advised because of the microarchitecture of this region.10
Because of the design of conical implants, they are capable to expand the surgical bed performed by the surgeon, which in clinical practice gives a feeling of greater stability. However, it is highly subjective and operator-dependent. Considering this, it has been recommended to verify the stability by reproducible and standardized methods.
This study aimed to determine the influence of implant macro-design (tapered and cylindrical) on primary and secondary stability in type II and type III bones.
Methods
A clinical, longitudinal and prospective study was conducted in the department of Oral maxillofacial Implantology at the School of Dentistry of the University of Chile between April 2006 and June 2007. All patients gave their informed consent in writing to take part in the study (003/2004) by CEC/FOUCH.
The present study included 18 patients (4 males and 14 females) with a mean age of 48 years (maximum age 75 years and minimum age of 20 years). A total of 34 implants were placed in the maxilla and mandible, in type II and type III bones according to Lekholm & Zarb classification. Lekholm & Zarb classification: Type I, the entire bone is composed of very thick cortical bone; Type II, thick layer of cortical bone surrounds a core of dense trabecular bone; Type III, thin layer of cortical bone surrounds a core of trabecular bone of good strength; and Type IV, very thin layer of cortical bone with low density trabecular bone.14
The following implant trademarks were included in this study: Brånemark System® MK III (TiUnite); OSSEOTITE® Implant System (Acid-etched); LTX 3i (RBM); Restore® (RBM); B&W® (Acid-etched); Replace Select Tapered® (TiUnite).
Inclusion criteria were:1 Smokers consuming less than five cigarettes per day;2 Systemic diseases outlined (ASA I and ASA II);3 Minimum bone availability of 15 mm in height and 5 mm in width; and4 Periodontal health and adequate oral hygiene according Gingival Index.
Exclusion criteria were:1 Presence of active infection or inflammation;2 Presence of pathological lesions in the maxilla or mandible;3 Patients with previous history of head and neck radiotherapy treatment.
The patient’s medical charts were filled out registering personal data, medical health and buccodental status. Extra-oral and intraoral pictures and periapical and panoramic radiographs were taken. Sites with inadequate bone volume were evaluated clinically and with CBCT before surgery by three professionals previously calibrated. All surgeries were performed by two surgeons previously calibrated lifting a full-thickness flap and performing the full sequence of surgical drills. Two different implants macro-design were used in the study: Cylindrical shaped implants and tapered shaped implants. The cylindrical implants have an average contact area of 237 mm2 including 2 sizes (diameter of 3.75 mm and a length of 13 mm and 15 mm). The tapered shaped implants have an average contact area of 226 mm2 including 2 sizes (diameter of 4.3 mm and a length of 13 mm and 16 mm). The contact area was possible to quantify through a simplified method.15
After implant placement, implant primary stability was measured by insertion torque (Ncm) and ISQ value (ISQ1). The insertion torque was measured through the digital reader provided by the OsseoSet® machine. When starting to insert the implant, the insertion torque was reduced and then increased until it was fully seated, this last value was considered. Resonance frequency measurements were recorded using Osstell™ Mentor, using a transducer screwed to the implant called Smartpeg®, which is connected wirelessly to a minicomputer that transforms the RFA records into ISQ units. Each implant was measured from two different angles, around 90 degrees apart and parallel to the crestal line. Secondary implant stability (ISQ2) was recorded at the moment of implant connection, between 4 to 6 months after implant placement.
Statistical analysis
Implant design (tapered or cylindrical) was compared with the primary and secondary stability values of resonance frequency (ISQ) and insertion torque (Ncm). When comparing the two groups, the non-parametric Wilcoxon test was used for insertion torque values, while the unpaired T-test was used for ISQ values. (SPSS 21.0,IBM,NY,USA).
Results
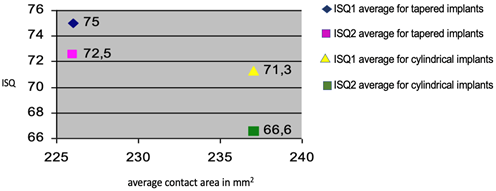
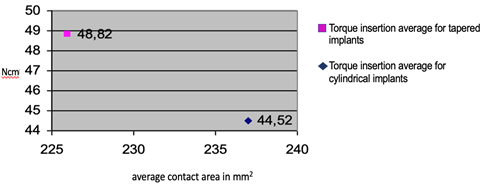
For cylindrical implants, the ISQ1 average value was 71,3, the ISQ2 average value was 66,6 and the insertion torque average value was 44,52 Ncm. For tapered implants, the ISQ1 average value was 75, the ISQ2 average value was 72,5 and the insertion torque average value was 48,82 Ncm. When comparing the two different implants macro-design, a significant difference was found in terms of ISQ1, ISQ2 and insertion torque average values. Average ISQ1: p = 0.0473 and Average ISQ2: p = 0.0039 Unpaired T-Test and Insertion Torque (p = 0.0031 Wilcoxon Test) (Graph N° 1 and N° 2).
Discussion
Implant geometry can significantly increase initial stability and the biomechanical fixation of the implant after the healing process.14 Therefore, dental implant stability is a prerequisite parameter to promote the process of osseointegration, consequently ensuring the success of an implant treatment.14 Depending on bone quantity and quality, the degree of implant anchorage may also be affected directly by the condition of bone itself as well.16
In the present study, insertion torque values were higher in tapered implants (48,82 N/cm) than in cylindrical implants (44,52 N/cm) (p = 0.0031). These higher values for primary stability in tapered implants show the importance of macro-design in achieving superior primary stability. This may be due that tapered implants apply more lateral compressive force on the bony walls surrounding the implant. Similarly, to our results, Sakoh et al.17 found significantly higher insertion torque values in tapered implants than in cylindrical implants. Additionally, they reported that the procedure of under-dimensioned drilling seemed to increase primary stability for both types of implants; however, the effect was only observable using insertion torque. RFA and Periotest, the noninvasive clinical methods tested, did not clearly demonstrate this difference. In another study, Menicucci et al.18 compared conical and cylindrical implant designs, finding higher insertion torque values for tapered implants (31.5 Ncm), compared with cylindrical implants (25.5 Ncm) (p = 0.05). Rokn et al.19 proposed that tapered implants apply more lateral compressive force on the bony walls, so in areas with inadequate bone quality and quantity, the use of tapered implants is recommended to achieve better primary stability.
Regarding RFA analysis, in the present study ISQ1 and ISQ 2 values were higher in tapered implants than in cylindrical implants. Likewise, some studies20,21 performed with implants placed in artificial bone blocks showed that conical implants show significantly higher ISQ values compared to cylindrical implants.
The results obtained in this research could open an important field to ensure the clinical effectiveness of osseointegrated implants. Despite the limitations of this study (in vitro stusy, low sample size, i.e.), the data obtained are significant and could result in new lines of research related to stability and macrodesign.