Introduction
Intertrochanteric fracture is the extracapsular proximal femur fracture between greater and lesser trochanter, which is commonly seen in elderly age group because of osteoporosis. The aim of treatment being achieving stability of fracture and early mobilisation, various treatment options was tried from extramedullary to intramedullary fixation.1
Treatment of proximal femur fractures continues to be major challenge, because of osteoporosis in elderly.2 Initially, Dynamic Hip Screw (DHS) was considered as stable fixation for all intertrochanteric fractures. Later with better understanding of biomechanics, DHS was preferred only for stable intertrochanteric fractures, based on the controlled collapse at the fracture site.
In case of unstable intertrochanteric fracture, Proximal femoral nail is better fixation to DHS alone, because of short lever arm that resists the bending force.3,4 DHS can’t be used alone and will require additional stabilisation with either trochanteric stabilisation plate or SS wire.5
Although proximal femoral nail (PFN) is superior to extramedullary implants, complications such as screw cut out, back out continued to exist. This was overcome with the advent of PFN A, as the helical blade system cuts through the cancellous bone and provides better anchoring, especially in case of osteoporosis.6
In the attempt to attain stable fixation, advancement in fixation methods continued starting from DHS to present day PFNA2 and InterTAN nail. Although there has been an increase in PFNA2 fixation over last decade, not much has been researched about the various parameters helpful in attaining stable fixation and overall results following usage of PFNA2.
Methods
This was a prospective study included 43 patients who presented with intertrochanteric fracture. All the patients with intertrochanteric fracture, treated with closed reduction and PFNA2 fixation in a tertiary care centre were included in the study.
Fractures with subtrochanteric extension, previous implants in injured hip, pathological fracture and age < 65 years were not included in the study. Patients underwent preoperative workup and x-rays at standardised distance. Based on AO classifications 12 patients belong to type A1 (stable) and 29 patients belong to type A2, A3 (unstable). All the patients underwent surgery within 7 days, based on their general condition.
The patients underwent closed reduction and PFNA2 fixation by experienced surgeons. Surgery was done under spinal anaesthesia, in fracture table. Fracture was reduced with the help of fluoroscopic imaging. Incision of size 5cm was made proximal to greater trochanter. Entry point was made 5mm medial to greater trochanter for all the patients with the help of awl and guide wire was passed. After reaming the entry point, long (16 patients)/short PFNA2 (24 patients) was used in the study, since both long and short nail behaved biomechanically similar.7,8 Distal locking was done in static/ dynamic mode which was decided based on the fracture pattern.
Postoperatively rehabilitation was started on day1 and weight bearing mobilisation was started from 1 week to 4 weeks postoperatively, depending on fracture fixation. Patient was followed up at 1 month, 3 months, 6 months and 1-year, functional outcome was studied using Harris hip score and Parker’s score.
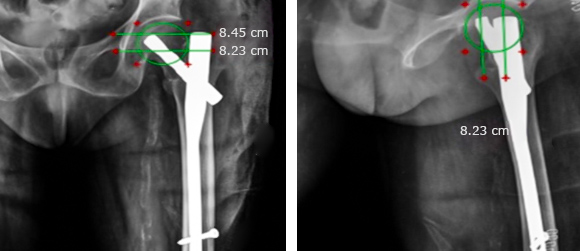
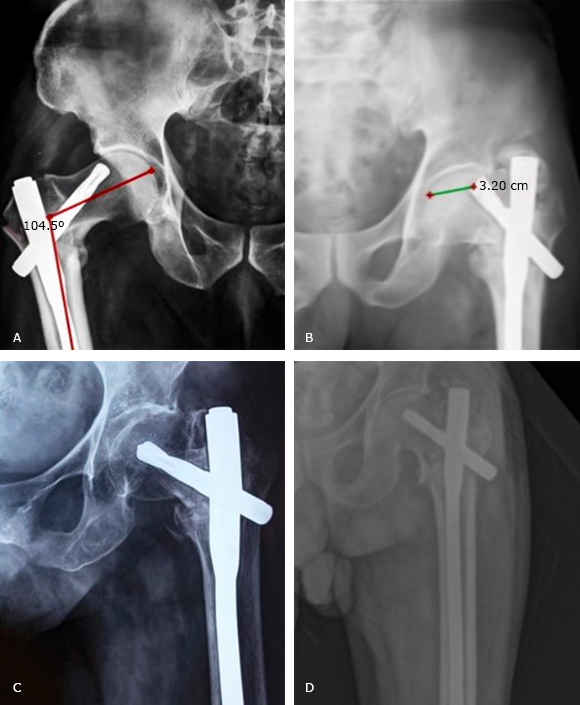
Fig. 2 In AP & lateral view, femoral head split into 3 equal quadrants & position of tip of helical blade was determined.
Data analysis was done by chi square test and Fischer exact test. Statistical analysis was done using SPSS res 17.0. It was decided that, p value less than 0.05 shall be considered significant.
Results
Out of 43 patients included studied, 2 patients died during the follow up. Average age of the patients was 72 years. Based on the AO classification system, 12 patients had stable (A1) and 29 patients had unstable fracture pattern (A2,3). About 80 % of the patients have grade III or below osteoporosis, as per Singh’s index. The mean duration for the surgery was 30.20 mins, with mean blood loss as 51 ± 23 ml. The average hospital stay was 6.31 ± 0.734 days. Out of 41 patients operated, 4 complications were noted, Screw backout in 1, cut out in 2 and absent radiological union in 1 patient (table 1).
Table 1 Demographic characteristics
| Characteristics | Parameters | Value |
|---|---|---|
| Sex | Male Female |
15 (36.58%) 26 (63.414%) |
| Mean Age | 72±345 years | |
| Fracture type | Stable (A1) Unstable (A2, A3) |
12 (29.268%) 29 (70.731%) |
| Singh’s Osteoporosis Index |
Grade I Grade II Grade III Grade IV Grade V |
8 (19.512%) 17 (41.463%) 8 (19.51%) 6 (14.63%) 2 (4.878%) |
| Mean surgical time | 30.20 minutes | |
| Mean blood loss | 51±23 ml | |
| Average hospital stays | 6.31±734 days | |
Functional outcome
Mean modified Harris hip score of 41 patients was 71. Out of the 9 patients with poor functional outcome, 3patients had preoperative functional score by itself less than 70. Considering the same, Parkers mobility score was calculated preop and postop. Average preop parker’s score was 5.8 against average postop parker’s score at the end of 6 months follow up 5.6. Hence, postoperative functional score is comparable to baseline score, indicating that there is only negligible mean loss of function seen post PFNA2 fixation.
Radiological outcome
The average TAD was found to be 25mm +/- 4.7mm. Out of 41 patients, 10 patients had TAD not within the range of 20-30mm, of which 4 patients developed implant related complications. Thus, a positive correlation was established between TAD and implant related complication by Fischer exact test with p value as 0.024. Seventy five percent of patients had Cleveland index 5(centre centre) or 8(inferior centre) (fig. 3). Out of the 10 patients with suboptimal Cleveland index, 3 of them continued to develop implant related complication, establishing a statistical correlation by Fischer exact test (p = 0.024) (Table 2).
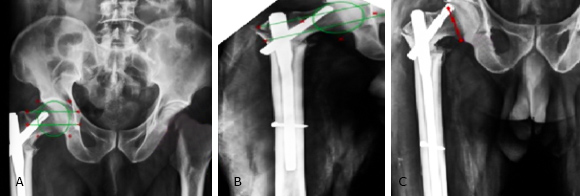
Fig. 3 A. post op x ray showing Cleveland index as 6 and TAD more than 30mm; B. 1-month postoperative x ray of same patient showing Cleveland index as 3; C. 3 months follow up showing screw cut out.
Table 2 Patients in each group of the studied parameter
| Tip apex distance
<20mm 20-30mm >30mm |
5 24 12 |
| Cleveland index
Optimal position (5&8) Suboptimal position (1,2,3,4,6,7,9) |
31 10 |
| Parkers ratio
|
27 14 |
| Nail potrusion height
0-5mm >5mm |
36 5 |
| Neck shaft angle
5-10 |
8 30 3 |
Although parkers ratio was correlating with the Cleveland index, it wasn’t found to be a reliable indicator of Implant related complications. Patients with parkers ratio less than 50 % and Cleveland index as 8, were found to have good functional outcome.
Most of the patients had nail protrusion height less than 5 mm. out of the 5 patients, none of them developed complications/poor functional outcome. Similarly, on comparing neck shaft angle with the normal side, a variation of more than 10° was noted only in 3 patients. However, they continued to have fair-good functional outcome (fig. 4 ).
Discussion
PFNA2 is preferred implant design for fixation in intertrochanteric fractures. Many studies in literature have shown consistent results with this implant. PFNA2 design provides better resistance against varus collapse and rotational stress. We studied clinical and radiological outcomes in fractures fixed with PFNA2.
Clinical and functional outcomes comparing different implant designs are available in literature suggesting better outcomes with PFNA2 design and lesser implant failure with PFNA2. Although intertrochanteric fractures have been wide prevalent fracture and various fixation methods have been used in the past, intramedullary nailing has been proven to be better fixation over DHS.4,9,10,11 With the advent of newer modifications in the available intramedullary system, efficacy of the same is less focused on. DHS was widely used initially in treating intertrochanteric fractures, biomechanical and cadaveric study with DHS concluded, for treating unstable intertrochanteric fractures, DHS requires additional stabilisation with SS wire / trochanteric plate.5 This was further substantiated when PFN was compared with DHS in treating unstable intertrochanteric fractures and concluded that PFN is better choice as it has shorter lever arm to resist bending force.3 Unlike DHS or PFN system, proximal femoral antirotation system demands better quality of reduction, as the helical blade cannot tolerate fracture pressure like ordinary lag screw.12
Radiological parameters have been described correlating the position of the helical blade in the head. Placement of screw in the head correlates with radiological outcomes. Hence studies must focus on radiological parameters which helps in achieving better reduction and also helps in predicting the outcome. The parameters describing the placement of screws in the head are Tip Apex distance, Cleveland index and Parkers ratio.
A study conducted by Baumgaertner et al,13 on 198 patients peritrochanteric fractures treated with sliding hip screw. They introduced new parameter named tip apex distance. On retrospective analysis, they found that patients with tip apex distance 25mm had a favourable outcome and patients with failure of fixation had average tip apex distance 38mm. Many biomechanical studies quote the importance of TAD,14 but debate over its significance still exists.13,15,16 TAD <25mm for DHS was found to have favourable outcome. Since PFN A2 had a helical blade, TAD of 20-30mm was preferred. If the TAD is less than 20mm with subchondral purchase, chances of cut through is higher. Similarly, if the TAD is more than 30mm, chances of cut out and back out of helical blade is more. Since the helical blade position in femoral head plays a vital role in predicting the outcome, Cleveland index was given importance. According to the various studies done so far, recommended Cleveland index is centre centre, inferior centre to avoid cut out.17
Nikoloski et al,15) in their retrospective study on 178 patients, treated with proximal femoral antirotation system found Tip apex distance of 20-30mm and Cleveland index 5 centre centre is associated with less complications of helical blade cut out, cut through. Also, recent biomechanical studies show that lower centre position of head screw had similar results to centre centre position, although tip apex distance was more than 25mm and TAD & Cleveland index were found to be reliable markers of untoward outcome, in this study.15
Another controversy which was prevalent among PFN A usage, is whether its length is appropriate for Asian population. As stated by other studies, proximal segment length of PFN A does not match that of Asian population, thereby causing friction between nail and soft tissue, which may result in thigh pain.16,17) This was studied with the help of NPH and parker’s ratio. Studies were done in Asian population with those treated with PFNA2. Patients followed up for 1 year, developing lateral trochanteric pain was graded as mild, moderate and severe. They were able to correlate nail protrusion height with position of helical blade using parker’s ratio.18,19 In our study, NPH was more than 10mm in 5 patients but it did not have much impact on patient’s quality of life. In contrast to other studies, both NPH and parkers ratio was not reliable indicator of complications.20,21,22
Functional outcome calculated by modified Harris hip score following PFNA2 fixation is found to be satisfactory in all cases.19,20 As the preoperative functional score should be taken into consideration, calculating postoperative score alone can be misguiding.23,24,25) Hence the mean loss of function after surgery was calculated with parker’s score, was found to be negligible.
Thus, PFNA2 confirms to be stable fixation for both stable and unstable intertrochanteric fractures in elderly patients with fewer complication and good functional outcome in short period of time. TAD of 20-30mm and optimal position of Cleveland index (centre centre or inferior centre) avoids implant failure.