Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.24 no.3 Pinar del Río mayo.-jun. 2020 Epub 01-Mayo-2020
Original article
Changes in hematological variables and globular sedimentation rate in non-critical patients withCOVID-19
1Hospital Provincial Docente Clínico Quirúrgico Dr. León Cuervo Rubio. Pinar del Río, Cuba.
2Universidad de Pinar del Río Hermanos Saíz Montes de Oca. Pinar del Río, Cuba
3Hospital Clínico Quirúrgico Abel Santamaría Cuadrado. Pinar del Río, Cuba
Introduction:
clinical hematology tests and globular sedimentation rate (ESR) have been used as markers of clinical evolution in patients with thenovel coronavirus disease 2019.
Objective:
to analyze changes in hematological variables and ESR in patients diagnosed with COVID-19 in non-critical status, admitted to Dr. León Cuervo Rubio Provincial Clinical-surgical Teaching Hospital, between March 16 and May 4, 2020.
Methods:
an observational-analytical and longitudinal-prospective study conducted with data from 44 non-critical patients with COVID-19. Samples were examined for: hemoglobin, hematocrit, global leukocyte count, neutrophils, lymphocytes, medium size cells and erythrocyte sedimentation rate; on admission, at 48hours of admission, on the eighth day and on medical discharge. The longitudinal changes of these variables were analyzed by means of the non-parametric Friedman test for k-related samples.
Results:
hematological variables: hemoglobin, hematocrit, global leukocyte count, neutrophils and lymphocytes did not have significant changes during the follow up. Only medium size cells decreased significantly in children, when comparing their mean value at discharge in relation to admission (p=0,028) and on the second day of hospitalization (p=0,01). In adult male patients, the ESR significantly decreased at eighth day of admission and at medical discharge, in relation to its value at admission (p=0,008).
Conclusions:
the changes observed in the hematological variables assessed, especially in the medium size cellsin children, and erythrocyte sedimentation rate in men with COVID-19 in non-critical status, respond to a favorable clinical evolution.
Key words: COVID-19; EPIDEMIOLOGIC FACTORS; PATIENT; HEMATOLOGY; LABORATORY TEST
INTRODUCTION
The novel pandemic (COVID-19) originated in Wuhan, Hubei Province, China, in December 2019. The etiological agent is a new coronavirus of suspected zoonotic origin with structural similarities to the viruses responsible for Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS).1
The spread of this virus (SARS-CoV-2) has infected more than five and a half million people worldwide, and caused more than three hundred thousand deaths, with a death rate of around 6%, both globally and in the region of the Americas. (2
In addition to Real-Time PCR testing (RT-PCR), which provides accurate information on the diagnosis of SARS-CoV-2 infection, (3 other laboratory tests have been evaluated as prognostic indicators of severity. (4, 5)
Based on studies carried out in China1,4) and other countries,6 the clinical hematology laboratory plays an important role in providing the medical team with a series of useful prognostic markers in the clinical evolution of the disease. Although the information in some cases is limited, the available findings establish that hematological variables represent an essential tool in the management of affected patients.
In turn, the erythrocyte sedimentation rate (ESR), or globular sedimentation rate, is an acute phase reactant defined as one of the useful complements in the prediction of patients with critical evolution.(4, 5)
In Cuba, the National Strategic Plan to Confront COVID-197 was designed in January 2020; which includes the Organizations of the Central State Administration, the Enterprises, Private Sector and the population in general. It comprises as part of its protocol, specifically in its Appendix-2, the complementary tests that should be indicated in each case. The hemogram with differential and erythrocyte sedimentation rate head the list of complementary tests in both suspected and confirmed cases.7
Taking into account the importance of the hemogram and its differential, as well as the ESR in the follow-up of the clinical evolution of SARS-CoV-2 infected patient, the present research aims to analyze the changes of these variables in hospitalized patients with COVID-19 in non-critical status, admitted to Dr. León Cuervo Rubio Provincial Clinical-surgical Teaching Hospital, Pinar del Río province, between March 16 and May 4, 2020.
METHODS
An observational-analytical and longitudinal-prospective (follow-up) study was conducted, in which a population of 44 SARS-CoV-2 confirmed patients was evaluated according to the Real Time Polymerase Chain Reaction (RT-PCR) 3, hospitalized at Dr. León Cuervo Rubio Provincial Clinical-surgical Teaching Hospitalin Pinar del Río province, between March 16 and May 4, 2020, none of them in critical condition. The patients were analyzed in four moments: at admission, at 48 hours of admission, at eighth day of admission and at discharge from the hospital.
The collection of the demographic, clinical and epidemiological data of the patients studied was possible due to the collaboration of the Department of Hygiene and Epidemiology of the Province.
Obtaining the samples
Each patient had 10 ml of blood drawn by venipuncture in one of the veins of the antecubital fossa, in accordance with the Guidelinesof Good Practice for the Clinical Laboratory and the national protocol for COVID-19 established by the Ministry of Public Health in Cuba. 7,8 The hematological variables and ESR were taken as data, at the four moments described above.
Determination of hematological variables
The determination of Hemoglobin (g/L), Hematocrit, Global Leukocyte Count (x109/L), Neutrophils (%), Lymphocytes (%) and Medium Size Cells (%) was performed with Mindray BC-3200 Hematology Complex, certified by Shenzhen Mindray Bio-Medical Electronics Co.,Ltd.; calibrated and controlled by B-30 Control Lot BC21115N-1 (For Mindray Hematology Analyzer).
Determination of ESR (Erythrocyte sedimentation) (mm/h)
Westergreen pipettes and stands were used for the ESR. The reading of the globular sedimentation rate was done on time, according to the requirements established for this procedure in Cuba. Reference values for all variables studied were those recognized in Cuba for adults and children. 8
The demographic, clinical, epidemiological and hematological data were stored in EXCEL 2016 for WINDOWS OFFICE. The normality of the quantitative variables was verified by the Shapiro-Wilk test. Data were summarized using statistics methods of central trend (mean), dispersion (standard deviation) and aggregation (percentages) according to the type of variable. The percentage distributions of the groups formed comprised for the qualitative variables were compared with the proportion-comparison test for independent samples.
The Friedman non-parametric test for k-related samples was used to analyze the longitudinal changes of the hematological variablesand the ESRof the patientduring the follow-up period. Comparison by pairs was performed in cases of statistical significance.
Statistical analysis of the results was performed with SPSS version 22. For all statistical tests, 95% of confidence was considered to point out the events of interest as significant (p<0.05).
The study was validated by the Scientific Council and Ethics Committee of the institution, as it was part of an institutional project entitled "Evaluation of patients with COVID-19 hospitalized at Dr. León Cuervo Rubio Provincial Clinical-surgical Teaching Hospital in Pinar del Río province".
RESULTS
Of the 44 patients evaluated, 68,2 % were adults. The mean age of the adult and pediatric patients was 45,8±16,1 and 9,3±4,2 years, respectively. (Table 1)
Table 1. Demographic, clinical and epidemiological characterization of patients with COVID-19 admitted to Dr. León Cuervo Rubio Provincial Clinical-surgical Teaching Hospital. Pinar del Río. March-May 2020.
| Variables of the patients | Patients | |
|---|---|---|
| Adults n [%] | Pediatric patients n [%] | |
| Hospitalized | 30 [68,2] | 14 [31,8] |
| Sex | ||
| Male | 14 [46,6] | 8 [57,1] |
| Female | 16 [53,4] | 6 [42,9] |
| Presence of symptoms | ||
| Asymptomatic | 14 [46,6] | 8[57,1] |
| Symptomatic | 16 [53,4] | 6[42,9] |
| Municipalities | ||
| Guane | 12 [40,0] | 3 [21,4] |
| Consolación | 9 [30,0] | 4 [28,6] |
| Pinar del Río | 8 [26,7] | 6 [42,9] |
| Viñales | 1 [3,3] | 1 [7,5] |
| Source of infection* | ||
| Abroad Cuba | 6 [20,0] 24 [80,0] | 2 [14,3] 12 [85,7] |
| Typeof case | ||
| Primary | 6 [20,0] | 1 [7,5] |
| Co-primary | 1 [3,3] | 0 |
| Secondary | 21 [70,0] | 13 [92,9] |
| Undetermined | 2 [6,7] | 0 |
*p<0.001 according to the Test of Comparison of Ratios for Independent Samples
The percentage distribution was similar in relation to sex and the presence or absence of clinical symptoms in both adult and pediatric patients. The cases diagnosed were mainly concentrated in the municipalities of Guane (40,0 %), Consolaciondel Sur (30,0%) and Pinar del Río (26,7%). The main source of infection came from confirmed cases of Cuban nationality (p<0.001) in the two study groups, with a predominance of secondary case classification in both adult (70 %), and pediatric patients (92,9 %).
The mean values of hemoglobin and hematocrit during the entire time of hospitalization of patients with COVID-19, showed no significant changes (p>0,05), in addition the average value for both hematological variables was in the normal range established for women, men and children, at all four times of the assessment. (Fig. 1)
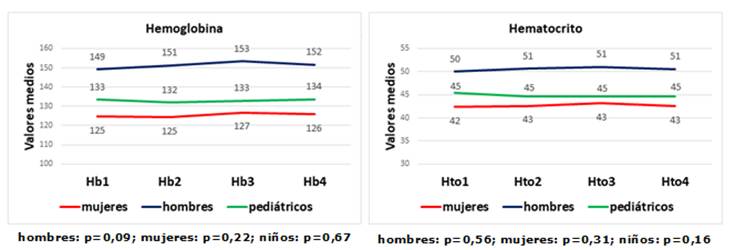
Fig. 1 Longitudinal values of hemoglobin and hematocrit in adults (according to sex) and pediatric patients with COVID-19, during the period of hospitalization (1: on admission; 2: at 48h; 3: on the eighth day of admission and 4: on discharge).
Although the results of the leukocyte count and its differential in the longitudinal study show certain trends in the variations of these cells, both in adults and in children during the evaluation period, only a slightly significant decrease in the average size cells was found for the pediatric patients (p=0,04). When the comparison was made by pairs in the non-parametric Friedman test for k-related samples, the statistical significance resulted, comparing the mean value of those cells at the time of the children's discharge with their value at the time of admission (p=0,028) and the second day of hospitalization (p=0,01). (Fig. 2)
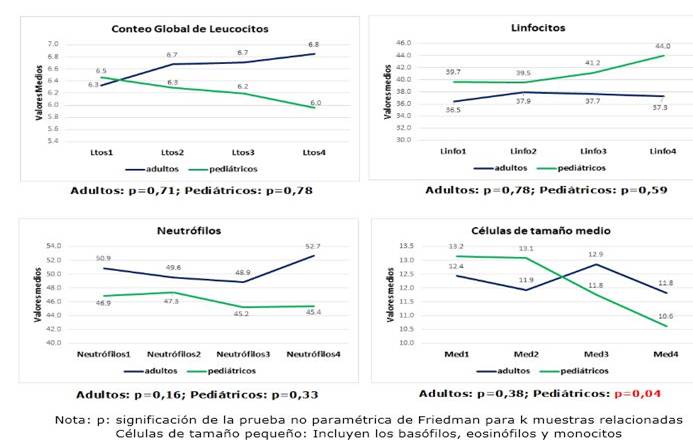
Fig. 2 Longitudinal values on the leukocyte count and differential of patients with COVID-19, during the period of hospitalization (1: on admission; 2: at 48h; 3: on the eighth day of admission and 4: on discharge).
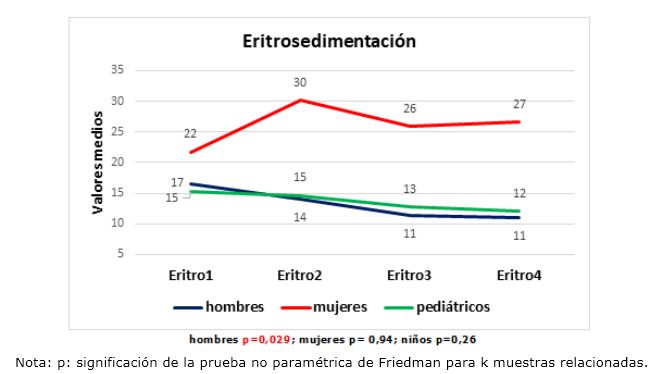
On the other hand, the erythrocyte sedimentation rate (ESR) showed slightly elevated values in all three study groups during the follow-up time, without significant changes (p>0,05) in women and children. In the case of adult male patients, the decrease in ESR at day 8 and medical discharge was statistically significant in relation to its value at admission (p=0,008 in the comparison of pairsby Friedman non-parametric test for k- related samples)(Fig. 3)
DISCUSSION
The longitudinal study of hematological variables, as well as other clinical laboratory determinations, has allowed health personnel to better understand and predict the clinical evolution of a significant number of human diseases, in current times, COVID-19 is not an exception.
Despite the heterogeneity observed among the available studies, most of them show that hemoglobin and hematocrit values are essentially reduced in critical patients with COVID-19, compared to those with milder manifestations of the disease. (1, 4) Therefore, initial assessment and longitudinal monitoring of hemoglobin values appear to be advisable in patients infected with SARS-CoV-2.
The anemia of the critical patients with COVID-19 may have a similar explanation to the anemia that appears in severe sepsis. Garcia de Lorenzo et al., (9) stated that this hematological alteration is not completely understood, and refer that it may be partially explained by the suppressive effect of inflammatory cytokines on renal erythropoietin production. In addition, these cytokines appear to inhibit red blood cell production directly in the bone marrow and stimulate iron-binding proteins that sequester iron and limit red blood cell production in these patients.
For the specific case of COVID-19, there is a hypothesis still to be tested according to which SARS-CoV-2 proteins, (ORF1ab, ORF10 and ORF3a) directly attack the hemoglobin of infected patients, and the arguments of this hypothesis are based on computerized methods, without experimental evidence up to the moment.10
As a result, the stability in the mean levels of hemoglobin and hematocrit found in the patients studied during the entire period of hospitalization, corresponds with the form of presentation of these hematological variables in the non-severe forms of the disease, reinforced by the fact that there were no reports of critical patients or deaths in this Cuban province during the time of the investigation. Nevertheless, it is valid to point out that, in the study, one patient of the total population (2,3 %) had low values of hemoglobin and hematocrit since admission, and three patients had polyglobulia (6,8 %), with favorable evolution in all cases.
The possible explanations for the anemia of critical patient with COVID-19 described above, allow the deduction of low serum levels of inflammatory cytokines and/or low viral load of SARS-CoV- 2 in the study population (non-critical patients). Leukocytosis, regardless of whether it represents neutrophilia, lymphocytosis or both, is observed in a minority of patients infected with COVID-19 and appears to indicate a bacterial infection or over-added infection. 6) In the specialized scientific literature, leukocytosis is reported in 11,4 % of patients with severe disease and in 4,8 % of patients with mild to moderate disease, demonstrating the relationship between the presence of leukocytosis and the severity of COVID-19 (odds ratio (OR), 2,54; 95 % confidence interval (CI)).4
Although the average for the overall leukocyte count at none of the four points in the study showed leukocytosis, it should be noted that out of a total of 44 patients only one presented leukocytosis (2,3 %), a lower percentage than the reports mentioned above.
Lymphopenia is common in patients with COVID-19, and it is believed that represents a defective immune response to the virus. 6,11 There seems to be some geographical variability in the percentage of patients who present lymphopenia. 4,6) It is likely that this alteration is caused by viral genomic mutations or that the immune response to the virus may change as the pandemic spreads to other countries. Another possibility is that the tests may not be uniform and, depending on when the sample is taken, the degree of lymphopenia may vary. 4,9,12 In the particular case of children, lymphopenia is less common, contrary to the behavior of other similar viruses.13
A report from March 202011 states that low lymphocyte counts in severe cases of COVID-19 are due to the action of the virus, but that host factors may also induce lymphopenia. Compared to patients who do not require intensive care, those admitted to the ICU with COVID-19 are mainly older adults, who already have a declined immune response (immunosenescence) and are more likely to suffer from comorbidities. Both aging and chronic diseases induce chronic endothelial dysfunction, which has an interconnection with lymphopenia. 4,9,11
The current research found mean values of lymphocytes in the normal range in both adult and pediatric patients; generally there was no lymphopenia in the population studied during the follow-up period. However, 38,6 % (13 adults and four children) of the studied population at some point in the investigation, showed low values of lymphocytes, without influence on their clinical evolution.In this sense, it is important to bear in mind that of the 44 patients infected with SARS-CoV-2 evaluated in this investigation, 31,8 % were children and the mean age of the 30 adults was 45,8 years old, where only seven were over 60 years old (23,3 % of the total number of adults); so that the infected adults were relatively young, consequently the minor coexistence of chronic diseases in them allowed this factor not to be taken into account in the study.
The data on variations in neutrophils in COVID-19 described in the literature have not been widely addressed up to the moment. Some authors state that the presence of neutrophilia may be an expression of the cytokine storm and the hyperinflammatory status as part of the pathogenic role triggered by SARS-Cov-2 or may also indicate over-added bacterial infection. 6,9,11
In recent research Eugene et al., 4 noted that neutrophilia is common in patients treated in the ICU during hospitalization (11,6 x109 / L compared to 3,5 x109 / L for patients who were not in the ICU, p<0,001).
The role of neutrophils in severe sepsis appears to be linked to pathogenicity of coagulopathy, particularly in thrombin restriction. Because of thrombin production, a group of mechanisms are activated, among them antithrombin (AT), which, when joined, blocks its proteolytic action. During septic processes TA concentrations are low due to consumption, alteration of synthesis and degradation by elastase from activated neutrophils, specifically. 9
As with other hematological variables, research is requiring to clearly demonstrate the role of neutrophils in COVID-19. However, there are studies12 which, using computer systems, attempt to identify possible inflammatory mechanisms and bioactive genes. Analysis of RNA-seq obtained from SARS-Cov-2 infected lung epithelial cells revealed that, the infected cells specifically expressed neutrophil-attracting chemokines, further supporting the likely role of neutrophils in the inflammation of this novel disease.
Another mechanism involved that is still not completely clear is ENTosis (Process of producing ENT: Extracellular Neutrophil Traps made up of chromatin, histones and granular antimicrobial proteins), induced by SARS-Cov-2 and other viruses. In this mechanism, on the one hand, there is virus entrapment, but the inflammatory and immunological reaction triggered by the release of ENTs by neutrophils, can be harmful in itself. The main objective is to understand whether the ENTs can be implied in the response to COVID-19 and by which mechanisms, resulting in concrete therapeutic proposals. 14
In the case of this report, no significant differences between adults and children were observed in this parameter, however, of the total patients, five (one child and four adults) (11,3 %) had mild neutrophilia at some point in the study, without compromising their evolution. This behavior could be related to the balanced response of the mechanisms involved that led to clinical stability in all patients.
The significant decrease in medium size cells (Mid %) from 48 hours after admission until discharge from the hospital at pediatric age is a result of the decrease, of at least one of the three types of cells: monocytes, basophils or eosinophils that are included in this category (Mid %). There are very few references in the literature about this variable, COVID-19 and pediatric age;14however, it seems that monocytes, along with other cells and molecules, are involved in the inflammatory pathogenesis of this novel disease, although there are still elements to be discovered. 4,13,15
Merad et al., 15 in their May 2020 study, stated that an inadequate response of macrophages and monocytes can trigger damage in patients with COVID-19, at the same time, macrophage activation syndrome has been found to induce severe infections, including SARS-Cov-2 virus.
In the present study it was found that, from the second day of the hospital admission, the Mid % decreased significantly. The non-critical evolution of the pediatric patients could be related to this decrease and be considered this moment, as a turning point to evaluate the evolution of these patients. It would be advisable to carry out further studies to compare these results with the dynamics of these cells in critical patients.
One of the acute phase reactants that from the beginning of the pandemic was associated with its increase and severe forms of the disease, was the ESR.This was defined as the most powerful factor to predict the progression of the disease provoke by SARS-Cov-2. 1,6 A later analysis showed that ESR, D-dimer, albumin and interleukin-6, were the main contributing factors to distinguish severe from mild patients 4.
In their pooled report of studies, Lapić et al.5 evaluated the usefulness of ESR to distinguish severe cases of COVID-19 from non-severe cases. Although the result of this analysis has been based on small sample sizes, similar to the present research, and with significant heterogeneity among studies, the researchers suggest that severe cases of COVID-19 are associated with significant elevations of ESR, compared to non-severe cases, reflecting the degree of inflammation, response and expression of acute phase proteins.
In the current study, a significant decrease in this variable was evident in men, on the eighth day and at medical discharge in relation to admission. It is valid to point out that with an average of two days elapsing between admission and the onset of symptoms (in those patients who turned out to be symptomatic). If these elements are associated to the fact that there were no patients who evolved to a critical status in this population in study, it could be indicated that, those adult-male-patients who, from the eighth day onwards, decrease their ESR with respect to admission, could have a favorable evolution of the disease.
Ensuring that the evolution of patients with COVID-19 is well-managed, requires health personnel, and in particular the clinical laboratory, to investigate possible analytical variables that contribute to a timely diagnosis of severe forms of the disease. The present study corroborated the stability of hematological variables in non-critical patients with COVID-19. However, a progressive decrease in the medium size cellscould indicate favorable evolution in the pediatric age, while the progressive decrease of the ESR during the disease in men would suggest a satisfactory course of the disease.
It is clear that the role of hematological variables and ESR,in COVID-19, requires in-depth scientific studies that clearly define their involvement in this disease and the possible associations with clinical and epidemiological variables, as well as with future vaccination and therapeutic alternatives.
REFERENCES
1. Zhu N, Zhang D, Wang W, Li X, Yang B et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med [Internet]. 2020 Feb [citado 19/5/2020>; 382(8): [aprox. 6p. ]. Disponible: Disponible: https://www.nejm.org/doi/full/10.1056/NEJMoa2001017 1. [ Links ]
2. WHO. Coronavirus disease (COVID-19) pandemic [Internet]. WHO; 2020. [actualizado 24 May 2020; citado 25/05/2020]. Disponible en: Disponible en: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 2. [ Links ]
3. Corman VM, Landt O, Kaiser M, Kaiser M, Molenkamp R. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Rev Eur Surveill [Internet]. 2020 Ene 25 [citado 19/5/2020]; 25(3): [aprox. 8p. ]. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988269/ 3. [ Links ]
4. Eugene B, Lian VC, Seok S, Hsiang G, Hsiang S. Hematologic parameters in patients with COVID-19 infection. AJH [Internet]. 2020 Ene 25 [citado 20/5/2020]; 95(6): [aprox. 5p. ]. Disponible en: Disponible en: https://onlinelibrary.wiley.com/doi/epdf/10.1002/ajh.25774 4. [ Links ]
5. Lapic I, Rogic D, Plebani M. Erythrocyte sedimentation rate is associated with severe coronavirus disease 2019 (COVID-19): a pooled analysis. Clin Chem Lab Med [Internet]. 2020 May [citado 20/5/2020]; 58(7): [aprox. 2p. ]. Disponible en: Disponible en: https://www.degruyter.com/view/journals/cclm/ahead-of-print/article-10.1515-cclm-2020-0620/article-10.1515-cclm-2020-0620.xml 5. [ Links ]
6. Frater JR, Zini G, d’Onofrio G, Rogers HJ. COVID-19 and the clinical hematology laboratory. ISLH [Internet]. 2020 Abr [citado 21/5/2020]; 42(s1): [aprox. 7p. ]. Disponible en: Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1111/ijlh.13229 6. [ Links ]
7. Misnisterio de Salud Pública. Protocolo de actuación nacional para la covid-19. (Versión provisional para uso del personal de salud que labora en el enfrentamiento a los casos) Versión 1.4. [Internet]. Infomed; Abril 2020 [actualizado Abr 2020; citado 23/05/2020] Disponible:Disponible:http://www.sld.cu/anuncio/2020/05/11/ministerio-de-salud-publica-protocolo-de-actuacion-nacional-para-la-covid-19 7. [ Links ]
8. Sociedad Cubana de Patología Clínica [Internet]. Cuba: Infomed; 2020 [actualizado 19 May 2020; citado 20/05/2020]. Disponible en: Disponible en: http://www.sld.cu/uvs/patologiaclinica/ 8. [ Links ]
9. García de Lorenzo Mateos A, Quintana Díaz M. Aspectos hematológicos en la sepsis grave. REMI [Internet]. 2004 Abr [citado 20/05/2020]; 4(12). Disponible: Disponible: https://remi.uninet.edu/2004/12/REMIC20.htm 9. [ Links ]
10. Wenzhong L, Hualan L. COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism. Rev Chem R xiv [Internet]. 2020 Abr 13 [citado 21/5/2020]; 26(7): [aprox. 23p. ]. Disponible en: Disponible en: https://chemrxiv.org/articles/COVID-19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173 10. [ Links ]
11. Zhang H, Wang X, Fu Z, Luo M, Zhang Z. Potential Factors for Prediction of Disease Severity of COVID-19 Patients. Med Rxiv [Internet]. 2020 Mar [citado 19/05/2020]. Disponible en: Disponible en: https://www.medrxiv.org/content/10.1101/2020.03.20.20039818v1 11. [ Links ]
12. Didangelos A. Neutrophil involvement in Covid-19. Preprint [Internet]. 2020 Abr [citado 19/05/2020]: [aprox. 5p. ]. Disponible: Disponible: https://www.preprints.org/manuscript/202004.0363/v2 12. [ Links ]
13. Henry BM, Lippi G, Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med [Internet]. 2020 Jun 25 [citado 12/5/2020]; 58(7): [aprox. 4p. ]. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32172227/ 13. [ Links ]
14. Mozzini Ch, Girelli D. The role of Neutrophil Extracellular Traps in Covid-19: only an hypothesis or a potential new field of research? Thromb Res [Internet]. 2020 Jul [citado 24/5/2020]; 191: [aprox. 1p. ]. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184981/ 14. [ Links ]
15. Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nad Rev Im [Internet]. 2020 May [citado 21/5/2020]; 20(6): [aprox. 7p. ]. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32376901/ 15. [ Links ]
Financing
REFERENCES
1. Zhu N, Zhang D, Wang W, Li X, Yang B et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med [Internet]. 2020 Feb [citado 19/5/2020>; 382(8): [aprox. 6p. ]. Disponible: Disponible: https://www.nejm.org/doi/full/10.1056/NEJMoa2001017 1. [ Links ]
2. WHO. Coronavirus disease (COVID-19) pandemic [Internet]. WHO; 2020. [actualizado 24 May 2020; citado 25/05/2020]. Disponible en: Disponible en: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 2. [ Links ]
3. Corman VM, Landt O, Kaiser M, Kaiser M, Molenkamp R. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Rev Eur Surveill [Internet]. 2020 Ene 25 [citado 19/5/2020]; 25(3): [aprox. 8p. ]. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988269/ 3. [ Links ]
4. Eugene B, Lian VC, Seok S, Hsiang G, Hsiang S. Hematologic parameters in patients with COVID-19 infection. AJH [Internet]. 2020 Ene 25 [citado 20/5/2020]; 95(6): [aprox. 5p. ]. Disponible en: Disponible en: https://onlinelibrary.wiley.com/doi/epdf/10.1002/ajh.25774 4. [ Links ]
5. Lapic I, Rogic D, Plebani M. Erythrocyte sedimentation rate is associated with severe coronavirus disease 2019 (COVID-19): a pooled analysis. Clin Chem Lab Med [Internet]. 2020 May [citado 20/5/2020]; 58(7): [aprox. 2p. ]. Disponible en: Disponible en: https://www.degruyter.com/view/journals/cclm/ahead-of-print/article-10.1515-cclm-2020-0620/article-10.1515-cclm-2020-0620.xml 5. [ Links ]
6. Frater JR, Zini G, d’Onofrio G, Rogers HJ. COVID-19 and the clinical hematology laboratory. ISLH [Internet]. 2020 Abr [citado 21/5/2020]; 42(s1): [aprox. 7p. ]. Disponible en: Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1111/ijlh.13229 6. [ Links ]
7. Misnisterio de Salud Pública. Protocolo de actuación nacional para la covid-19. (Versión provisional para uso del personal de salud que labora en el enfrentamiento a los casos) Versión 1.4. [Internet]. Infomed; Abril 2020 [actualizado Abr 2020; citado 23/05/2020] Disponible:Disponible:http://www.sld.cu/anuncio/2020/05/11/ministerio-de-salud-publica-protocolo-de-actuacion-nacional-para-la-covid-19 7. [ Links ]
8. Sociedad Cubana de Patología Clínica [Internet]. Cuba: Infomed; 2020 [actualizado 19 May 2020; citado 20/05/2020]. Disponible en: Disponible en: http://www.sld.cu/uvs/patologiaclinica/ 8. [ Links ]
9. García de Lorenzo Mateos A, Quintana Díaz M. Aspectos hematológicos en la sepsis grave. REMI [Internet]. 2004 Abr [citado 20/05/2020]; 4(12). Disponible: Disponible: https://remi.uninet.edu/2004/12/REMIC20.htm 9. [ Links ]
10. Wenzhong L, Hualan L. COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism. Rev Chem R xiv [Internet]. 2020 Abr 13 [citado 21/5/2020]; 26(7): [aprox. 23p. ]. Disponible en: Disponible en: https://chemrxiv.org/articles/COVID-19_Disease_ORF8_and_Surface_Glycoprotein_Inhibit_Heme_Metabolism_by_Binding_to_Porphyrin/11938173 10. [ Links ]
11. Zhang H, Wang X, Fu Z, Luo M, Zhang Z. Potential Factors for Prediction of Disease Severity of COVID-19 Patients. Med Rxiv [Internet]. 2020 Mar [citado 19/05/2020]. Disponible en: Disponible en: https://www.medrxiv.org/content/10.1101/2020.03.20.20039818v1 11. [ Links ]
12. Didangelos A. Neutrophil involvement in Covid-19. Preprint [Internet]. 2020 Abr [citado 19/05/2020]: [aprox. 5p. ]. Disponible: Disponible: https://www.preprints.org/manuscript/202004.0363/v2 12. [ Links ]
13. Henry BM, Lippi G, Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med [Internet]. 2020 Jun 25 [citado 12/5/2020]; 58(7): [aprox. 4p. ]. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32172227/ 13. [ Links ]
14. Mozzini Ch, Girelli D. The role of Neutrophil Extracellular Traps in Covid-19: only an hypothesis or a potential new field of research? Thromb Res [Internet]. 2020 Jul [citado 24/5/2020]; 191: [aprox. 1p. ]. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7184981/ 14. [ Links ]
15. Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nad Rev Im [Internet]. 2020 May [citado 21/5/2020]; 20(6): [aprox. 7p. ]. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32376901/ 15. [ Links ]
Additional material
Received: May 26, 2020; Accepted: June 15, 2020











 texto en
texto en