Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 no.1 Pinar del Río ene.-feb. 2023 Epub 01-Ene-2023
Articles
Relationship between nutritional status, perinatal and family history and blood pressure levels in adolescents
1University of Medical Sciences of Pinar del Rio. Faculty of Medical Sciences "Dr. Ernesto Che Guevara de la Serna". Pinar del Río, Cuba
Introduction:
arterial hypertension and its risk factors go unnoticed in adolescence, so it is vital to carry out an active search in this population to improve its evolution and prognosis.
Objective:
to determine the possible relationship between nutritional status, perinatal and family history and blood pressure in adolescents in the 8th grade of the Secondary School Carlos Ulloa.
Methods:
an observational, analytical and cross-sectional study was carried out in 72 adolescents belonging to this institution. A questionnaire was administered to the guardians, which collected family and perinatal pathological antecedents. The adolescents were measured for weight, height, waist circumference, hip circumference, arm circumference, tricipital fold, systolic and diastolic blood pressure. Mean, standard deviation, absolute and relative frequencies were used, as well as mean, chi-square and Spearman correlation comparisons, all at 95 % confidence.
Results:
36,1 % showed elevated blood pressure, prehypertension (23,6 %) or arterial hypertension (8,3 % stage I and 4,2 % stage II). The patient's history of The most important factors associated with the presence of elevated blood pressure were obesity and gestational diabetes (p<0,05). High waist circumference and waist-to-height ratio showed a statistically significant association (p<0,05) with elevated blood pressure. Systolic and diastolic blood pressure were positively and significantly correlated with weight, body mass index, waist circumference, hip and waist-height index.
Conclusions:
the frequency of elevated blood pressure was present in one third of the population studied and associations with pregnancy history and excess malnutrition were identified.
Key words: ARTERIAL HYPERTENSION; ADOLESCENT; RISK FACTORS; OBESITY
INTRODUCTION
Arterial hypertension is the main risk factor for the development of cardiovascular diseases, constituting the first cause of death worldwide; it is responsible for at least 45 % of deaths due to heart disease and 51 % due to stroke.1) It was considered a disease of adult life, which only in some cases occurred in children, when they had some underlying disease that conditioned it, which has been called secondary arterial hypertension. Today it is known that essential or primary arterial hypertension in adults often begins in childhood.2
Epidemiological studies of children and adolescents in the last 20 years reveal an increase in the prevalence of hypertension and prehypertension, explained in part by the increase in obesity, thus; prehypertension progresses to hypertension at a rate of approximately 7 % per year. In adolescence, this increase is between 4,7 to 13 % in the population under 18 years of age, a worrisome fact, since the increase in blood pressure levels in adolescence remains throughout life and leads to a series of early complications in adulthood.3
In Cuba, as in the rest of the world, AHT is not a very frequent problem in pediatrics compared to adults; however, when it occurs, the consequences can be very serious. According to reports its frequency is around 30% in adolescence. In 2015 in Cuba, a rate of arterial hypertension of 0,2 per thousand inhabitants, between 10 and 14 years of age, was recorded. However, according to reports of a study conducted in 1026 high school students of both sexes in Havana the prevalence of primary HT resulted in 4,7 % and prehypertensive of 9,7 %.4
International and national studies such as the one conducted in Yunnan, China among the school-aged population aged 9 to 17 years between 2017 to 2019 the total prevalence of hypertension was 13,72 %, 12,49 % and 13,45 % respectively.5)
In Chiquimula, Guatemala a study on Arterial hypertension and obesity in school children aged 6 to 15 years, recorded 8,38 % with arterial hypertension (AHT) and 22,7 % prehypertension. Of the children with hypertension, 83.9% were overweight; 58,3 % of the overweight children had prehypertension, which demonstrates the association of excess malnutrition with a risk factor for hypertension.6
In Villa Clara, Cuba, a study on arterial hypertension in childhood found a high incidence of prehypertensive and hypertensive infants (37,.3 %), demonstrating that the alteration of blood pressure figures at an early age has become a problem to be addressed worldwide.7
Several studies have shown that arterial hypertension has its origins in early stages of life, with evidence showing the frequency of hypertension in members of some families, studies on pro-hypertensive genes, experiments in sodium sensitive rats, the high incidence associated with lipid and carbohydrate dysmetabolism, association with obesity, systematic alcohol intake, smoking, and steroid intake.8
This entity has been clinically observed in young individuals, confirming a certain genetic predisposition, which interacts with phenotypic phenomena and depends on environmental influences.9
Arterial hypertension in children and adolescents has increased as a clinical entity in association with other risk factors for cardiovascular disease, including obesity, insulin resistance and dyslipidemia. The prevalence of lipid abnormalities in children is increasing and is associated with the obesity epidemic, as well as the metabolic syndrome that includes HT. Obesity and overweight have been widely recognized in different studies as a conditioning factor, and one that needs to be modified, with respect to the development and prevention of HT and other cardiovascular diseases.10
The identification of risk factors is the main measure to control cardiovascular disease. Modifiable factors are those that can be changed to reduce or eliminate the probability of having the problem and enjoying a productive life.11
The factors associated with HT can be summarized as age, gender, ethnicity and heredity (non-modifiable), smoking, alcohol, sedentary lifestyle, diet, sociological and social (behavioral modifiable) and overweight, obesity, dyslipidemia, diabetes mellitus (metabolic modifiable). Non-modifiable or non-preventable factors are inherent to the individual. However, the modifiable ones are associated with lifestyle, so they can be prevented, minimized or, better yet, eliminated.12
In the province of Pinar del Río in 2018, a study entitled "Factors associated with arterial hypertension in adolescents in San Juan y Martínez, 2018,12" was conducted in which epidemiological elements related to the presence of high blood pressure in adolescents are provided.
The morbidity of arterial hypertension is increasing in pediatric ages. The recognition of its presence at this stage would allow the modification of lifestyles and also the implementation of therapeutic measures to minimize its impact on adult life. In the province of Pinar del Rio, few studies have been reported on the frequency of arterial hypertension or prehypertension in adolescents, its relationship with perinatal and family antecedents and nutritional status. Taking into account the great importance of this subject, and the essential need to control this disease especially at early ages, the present work is conducted in this province to provide more evidence in relation to this health problem. The present research aims to determine the possible relationship of nutritional status, perinatal and family history with blood pressure figures in adolescents of the 8th grade of the ESBU Carlos Ulloa.
METHODS
An observational, analytical and cross-sectional research was carried out in adolescents belonging to the 8th grade of the Carlos Ulloa ESBU in the city of Pinar del Río. The universe was constituted by the totality of 8th grade students of the ESBU Carlos Ulloa (n=346), it was possible to include in the sample 72 students due to the epidemiological situation of COVID-19 which met the following inclusion criteria: Adolescents of the 8th grade of the ESBU Carlos Ulloa to whom it was possible to perform all the anthropometric and blood pressure measurements prior consent of their parents or guardians to participate in the study and whose guardians answered the questionnaire of perinatal and family history.
Prior coordination was made with the management of the Carlos Ulloa ESBU to obtain authorization to carry out the study. The authorization was accepted and coordination was made with the person in charge of the eighth grade to organize the different times when all the determinations of the present study would be made according to the possibilities of the teaching schedule.
In addition, a meeting was arranged with the guardians of these adolescents to inform them of the objectives and conditions of the study in an attempt to obtain their consent for the inclusion of their children in the research and to apply the perinatal and family history questionnaire to parents or guardians. This meeting took place and subsequently the questionnaire was applied in each of their children's classrooms in a school for parents or guardians held at the school.
A room with adequate conditions was set up in which the following anthropometric determinations were made: Weight, Height, Waist circumference (CCi), hip circumference (CC) and tricipital fold (PT) with which it was possible to calculate the indicators body mass index (BMI), waist-height index (WHI) and waist-hip index (WHI) and systolic and diastolic blood pressure were measured.
Body height and weight were measured according to internationally standardized protocols,13 using an electronic digital scale (KERN, United States) with a resolution of 0,100 kg and an attached stadiometer. BMI was calculated according to the formula weight(kg)/height2(m) and was considered obese if the BMI was >percentile (pc) 97 according to age and sex in the curves for Cuban children and adolescents, overweight if the BMI was > pc 90 and ≤ pc 97, normal weight if the BMI was between pc 10 and 90, and underweight if the BMI was <pc 10. The Cci was measured at the end of a smooth expiration, with the subject in a standing position, at the midpoint between the lower costal border and the iliac crest at the level of the mid-axillary line, and parallel to the standing plane. Abdominal obesity was considered when the Cci was higher than the 90th percentile. The percentile table used was the one proposed by Esquivel and colls,14 in Havana, Cuba in the absence of reference tables for this indicator in the Cuban population.
Hip circumference was measured at the level of the gluteal prominence and the ICC was calculated as the ratio between waist and hip circumference. The 90th percentile was taken as the cut-off point indicative of cardiovascular risk due to CHF, as described by Mederico et al,15 in Venezuela, in the absence of reference tables of CHF percentiles, the tables offered in this study were taken as a reference.
The CCI was calculated from the current values of the subject's CCi and height as previously described.16 The obtained ICT value was stratified as follows: Acceptable: ICT < 0,50 vs. Elevated: ICT ≥0,50; respectively.
In addition, the circumference of the arm was measured using a tape measure which was placed in the middle part of the arm taking as reference the length between the tip of the shoulder (acromion) and the head of the radius (olecranon).
The tricipital crease was measured using a metallic Holtain plicometer calibrated in millimeters and the midpoint of the arm was carefully chosen, which is none other than the midpoint between the acromion at its most superior and external point and the head of the radius at its lateral and external point. The measurement was taken with the arm relaxed and hanging laterally, with the shoulder joint in slight external rotation and the elbow extended. The crease formed parallel to the longitudinal axis, with the thumb and index finger of the left hand separated from the underlying muscle and measured at that point, placing the plicometer perpendicular to the crease. was taken on the posterior aspect of the arm, over the triceps muscle, midway between the lateral projection of the acromion process of the scapula and the inferior margin of the olecranon process of the ulna.
Determination of blood pressure:
To measure the adolescent's blood pressure, in addition to meeting the same requirements as the adult, the size of the cuff should be taken into account, which should cover approximately 2/3 of the arm and the inflatable bag inside should cover the entire circumference of the arm or at least 80 %. If the cuff is smaller it will yield higher blood pressures and if it is larger it will be lower. The arm was supported and at the level of the heart, without rounding the figures. The systolic and diastolic blood pressures were taken as reference for the first and fifth Korotkoff noises, respectively, as in the adult, and the measurements were taken in triplicate.17
The criteria for arterial hypertension in children are based on the tables of percentile values according to age, sex and height of the SecondTaskForceonBloodPressure of 1996 and its most recent update in 2004 (Fourth Report of Children) by the WorkingGroup collected in the Cuban Guide for the prevention, diagnosis and treatment of arterial hypertension.18,19
- Normal: systolic and/or diastolic BP less than the 90th percentile for age, sex and height.
- Prehypertensive: equal to or greater than the 90th percentile and less than the 95th percentile, as well as all those with blood pressure figures equal to or greater than 120/80.
The basic descriptive parameters were estimated: mean and standard deviation for quantitative variables and absolute frequencies (No.) and relative percentages (%) for qualitative variables. Box and whisker plots, scatter plots and histograms were used to characterize the distribution of the variables, detect aberrant points and check the assumptions of normality for the tests that required it.
A mean comparison test was used for quantitative variables (Mann Whitney U) and the chi-square test for comparison of proportions by group and for the determination of the association between categorical variables. A 95 % confidence level was used for all tests. The results were expressed in tables to facilitate a quicker understanding. The data were processed using SPSS,21 for Windows.
This research was carried out with the previous authorization of the Research Ethics Committee of the Faculty of Medical Sciences Dr. "Ernesto Che Guevara de la Serna". All data obtained will be used for strictly scientific purposes and will only be disclosed in events and published in prestigious journals.
RESULTS
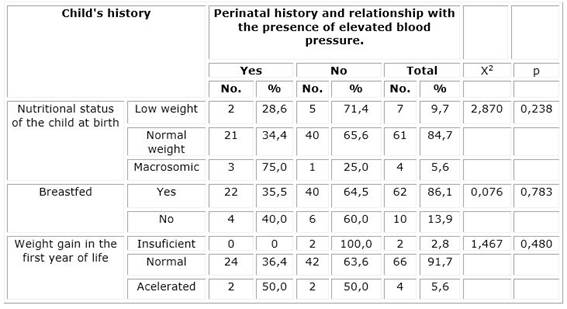
Table 1 shows the diagnosis made according to systolic and diastolic blood pressure figures by sex.
Table 1 Diagnosis according to systolic and diastolic blood pressure figures by sex.
X2=1.581 p=0.064
Legend:
BP: blood pressure. AHT IE: Arterial Hypertension Stage I. AHT IBD: Arterial Hypertension Stage II.
Table 1 shows that females predominated in the population of adolescents studied, with 55,6 %.
Of the sample, 63,9 % had normal blood pressure figures and 36.1% showed blood pressure levels considered normal-high (23,6 %) or arterial hypertension in any of its stages (8,3 % stage I and 4,2 % in stage II).
The test for comparison of proportions by group showed that there was no difference in the frequency of different blood pressure levels between the two sexes (p>0,05).
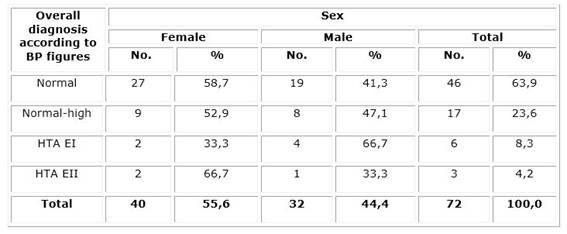
Table 2 below shows the family pathological history and during maternal pregnancy and its relationship with the presence or not of elevated blood pressure figures in the adolescents studied.
Table 2 Family and pregnancy pathological history and its relationship with the presence or not of elevated blood pressure in the adolescents studied.
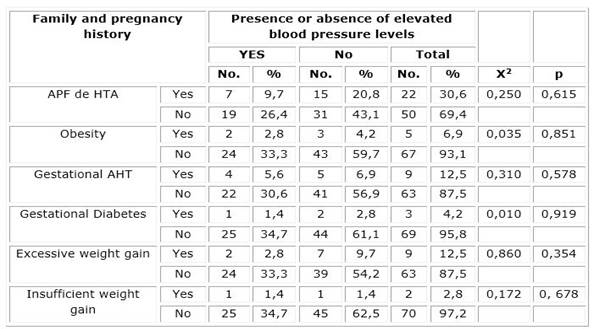
Table 2 shows that no association was found between maternal or paternal family history of hypertension and the presence of high blood pressure in the adolescents included in the study. In the case of maternal pregnancy history, a statistically significant association was found between maternal obesity during pregnancy and having had gestational diabetes and the presence of high blood pressure during adolescence in these patients (p<0,05), and no association was found with any of the other antecedents evaluated (p>0,05).
As can be seen, when considering the birth weight factor, no association was found between the presence of low or high birth weight and the presence of high blood pressure. Nor was there any association between high blood pressure and not having received breastfeeding or inadequate weight gain during the first year of life (p>0,05).
Table 4 shows the relationship between the presence of excess malnutrition as assessed according to different anthropometric indicators and the presence or absence of high blood pressure.
Table 4 Relationship between the presence of excess malnutrition as assessed according to different anthropometric indicators and the presence or absence of high blood pressure.
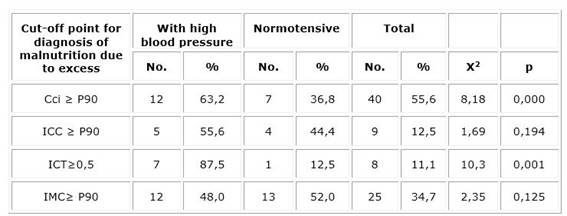
Legend: Cci: Waist circumference. ICC: Waist Hip Index. WHI: Waist-to-height ratio. BMI: Body Mass Index.
A statistically significant association was found between the presence of abdominal obesity as assessed by waist circumference values (CCi>P90) and the presence of high blood pressure in the sample studied (p<0,05). Similarly, the waist-to-height ratio ≥0,5 was also found to be significantly associated (p<0,05) with elevated blood pressure. No statistically significant association (p>0,05) was found between waist-hip index ≥ P90 or body mass index ≥ P90 and the presence of elevated blood pressure figures.
Table 5 shows the mean values and standard deviation of the different anthropometric indicators evaluated, taking into account the presence or absence of elevated blood pressure among the adolescents studied. In addition, the mean comparison test and its significance are shown.
Table 5 Mean values and standard deviation of the different anthropometric indicators evaluated taking into account the presence or absence of high blood pressure among the adolescents studied.
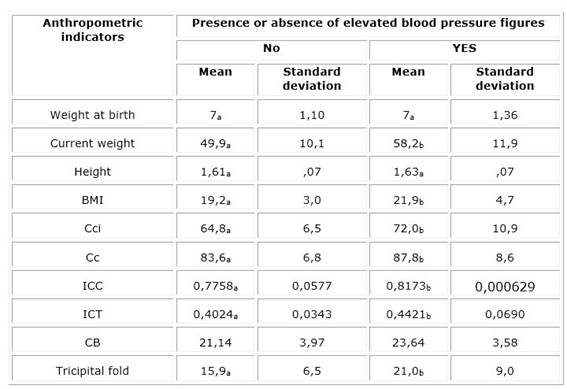
Legend: BMI: Body Mass Index. Cci: Waist circumference.
Cc: Hip circumference. HCW: Waist Hip Index. ICT: Waist Height Index.
CB: Circumference of the Arm.
Note: Values in the same row and subtable that do not share the same subscript are significantly different at p<0.05 in the two-sided test of equality for column means.
As can be seen with the exception of birth weight and arm circumference the rest of the anthropometric parameters evaluated showed higher mean values among adolescents with elevated blood pressure figures with statistically significant differences with those who had normal blood pressure figures (p<0,05).
DISCUSSION
There is evidence that cardiovascular disease begins at an increasingly younger age. The prevalence of arterial hypertension in pediatric ages reported in epidemiological data from developed countries is between 4,7 and 13 %.20
In the present study, 36.1 % showed elevated blood pressure, prehypertension (23,6 %) and arterial hypertension (8,3 % stage I and 4,2 % in stage II), a higher frequency than that recorded in another study carried out in Pinar del Rio, Sandino municipality by Troche Valdés and collaborators,21) where the prevalence of prehypertensive patients was 3,57 % and 5,87 % of hypertensive patients.
In a similar study carried out in Paraguay by Real Delor and collaborators, (21 lower figures were also obtained, with only 1,5 % of all adolescents studied having arterial hypertension. The difference could be due to the fact that the samples are not similar, as they were made in different social and geographic contexts, in addition to the small sample size, the main limitation of this study as a consequence of the Covid-19 pandemic.
The study found no association between maternal or paternal family history of hypertension and the presence of high blood pressure in the adolescents included, which shows that the genetic component does not determine the presence of high blood pressure in this sample but that other associated factors are present; however, according to Mata Wong,2 in a study of 203 adolescents, 33 (16,2 %) were hypertensive and of these, 60,6 % had a family history of hypertension and (57,5 %) of obesity.
In the case of maternal pregnancy history, a statistically significant association was found between maternal obesity during pregnancy and having had gestational diabetes and high blood pressure during adolescence in these patients (p<0,05), and no association was found with any of the other antecedents evaluated (p>0,05). No similar results were found in other national or international studies for comparison.
Systolic and diastolic blood pressure were positively and significantly correlated with weight, body mass index, waist circumference, hip circumference and waist-height index. A statistically significant association was found between the presence of abdominal obesity as assessed by waist circumference values (CCi>P90) and the presence of high blood pressure in the sample studied (p<0,05).
Similarly, the waist-to-height ratio ≥0,5 was also found to be significantly associated (p<0,05) with elevated blood pressure. No statistically significant association (p>0,05) was found between waist-hip index ≥ P90 or body mass index ≥ P90 and the presence of elevated blood pressure figures.
For many years, BMI has been the anthropometric indicator of choice for the prediction of cardiovascular damage or other health risks due to the ease of obtaining the primary variables, and its calculation and interpretation. However, it is clear to many that BMI can be affected by the muscularity of the subject as well as by the presence of water distribution disorders.21
On the other hand, waist circumference (WC) is a useful anthropometric measure for the identification of abdominal obesity and has been rated as a better tool for assessing cardiovascular and metabolic risk than body mass index (BMI).12
Similar results to this study were obtained by Rojas Concepción and collaborators,10 who reported a relationship between excess malnutrition and the presence of arterial hypertension. Other studies also agree with this research, such is the case of the one carried out by Amor Micaela and collaborators,22 in the city of Buenos Aires, Argentina, who found a 6,6 % prevalence of HT in the adolescents studied, mainly associated with obesity and overweight (10,9 %) and with an increased waist circumference (13,4 %). These authors also coincide in finding no statistically significant association between the waist-hip index and the presence of high blood pressure.
With similar results, Cabal Giner and collaborators,23 in a study carried out in Havana reported that 0,7 % of the school children in their study series presented elevated blood pressure figures, of which 5,0 % were obese. This was corroborated when CC and CTI were used as predictors. Thus, schoolchildren with increased CC and/or CTI values were also those with increased BP values.
Garí Llanes,7 in his research determined that weight, height and body mass index, in isolation, are not good predictors of blood pressure; however, among the anthropometric markers studied, the waist circumference variable shows a continuously increasing mean (among the variables, it is the best predictor of blood pressure), which coincides with the findings of the present study.
It is worth highlighting the importance and obligatory nature of measuring BP and assessing nutritional status in consultations with adolescents. Taking into account the positive and significant correlation between blood pressure and weight, body mass index, waist circumference, hip circumference and waist-to-height ratio, an appropriate nutritional assessment should be made of adolescents in consultations, measuring all anthropometric markers, as well as detecting risk factors for hypertension and implementing an action plan to favorably address modifiable factors.24,25
It is concluded that the frequency of high blood pressure was present in one third of the population studied and associations with pregnancy history and excess malnutrition were identified.
BIBLIOGRAPHIC REFERENCES
1. Álvarez Ochoa R, Pinguil Yugsi M, Cordero Cordero G. Factores de riesgo de hipertensión arterial en adolescentes. Revista Científica Y Tecnológica UPSE [Internet]. 2018 [citado 24/03/2021]; 5(2): 111-118. Disponible en: Disponible en: https://doi.org/10.26423/rctu.v5i2.347 1. [ Links ]
2. Mata Wong P. Factores de riesgo asociados a hipertensión arterial en adolescentes de 12 a 17 años [Tesis]. Universidad Veracruzana. Región Veracruz. Facultad de Medicina, 2018 [citado 23/03/2021]. Disponible en: Disponible en: https://cdigital.uv.mx/bitstream/handle/1944/49716/MataWongPablo.pdf?sequence=1&isAllowed=y 2. [ Links ]
3. Organización Mundial de la Salud. [Internet]. OMS; 2017 [citado 24/03/2021]. Disponible en: http://www.who.int/mediacentre/factsheets/fs311/es3. [ Links ]
4. Pérez Quintana O, Paz Barthelemy R, Mercadilla Ramírez S, Hermosilla Batista GI, Pérez Mola K, Barcelay Salvador N. Comportamiento de factores de riesgo de hipertensión arterial en niños y adolescentes. Municipio Guantánamo. 2018 - V Congreso virtual de Ciencias Morfológicas [Internet]. 2020 [citado 23/03/2021]. Disponible en: Disponible en: http://morfovirtual2020.sld.cu/index.php/morfovirtual/morfovirtual2020/paper/download/768/646 4. [ Links ]
5. Yunjuan Yang, Jieqing Mi, Litao Chang, Jiajia Chai, Zhizhong Song, ShunZha, et al. Tendencias de prevalencia de hipertensión entre niños y adolescentes de 9 a 17 años en Yunnan, 2017-2019: a serial cross-sectional surveillance survey. Salud Pública de BMC [Internet]. 2021 [citado 20/05/2021]; 21(1). Disponible en: Disponible en: https://www.researchgate.net/publication/349267983_Prevalence_trends_of_hypertension_among_9-7_aged_children_and_adolescents_in_Yunnan_2017 5. - [ Links ]
6. Díaz S, Melvin Bonilla F. Diagnóstico y evaluación de la hipertensión arterial en niños. Archivos Latinoamericanos de Nefrología Pediátrica. [Internet] 2019 [citado 08/06/2021]; 76-88. Disponible en: Disponible en: http://www.cdc.gov/growcharths 6. [ Links ]
7. Garí Llanes M, García Nóbrega Y, Chávez González E, González Rodríguez CE, García Sáez J, González Cuétara JM. Hipertensión arterial en la infancia. Factores de riesgo antropométricos relacionados con su presencia. Acta Médica del Centro [Internet]. 2018 [citado 20/05/2021]; 12(4): 455-460. Disponible en: Disponible en: https://www.medigraphic.com/pdfs/medicadelcentro/mec-2018/mec184g.pdf 7. [ Links ]
8. Laura Campos M. Usuarios ambulatorios del Hospital Manuel Ángel Higa ArakakiSatipo, 2017 [Tesis]. UNIVERSIDAD PERUANA LOS ANDES FACULTAD DE CIENCIAS DE SALUD; 2020 [citado 20/05/2021]. Disponible en: Disponible en: https://repositorio.upla.edu.pe/bitstream/handle/20.500.12848/2087/TESIS%20FINAL.pdf?sequence=1&isAllowed=y 8. [ Links ]
9. Domínguez Fabars A, Díaz Samada RE, Casin Rodríguez SM, Adiz Marino A. Intervención educativa sobre temas de Hipertensión Arterial en adolescentes [Internet]. Convención Internacional de Salud, Cuba Salud; 2018 [citado 20/05/2021]. Disponible en: Disponible en: http://www.convencionsalud2018.sld.cu/index.php/connvencionsalud/2018/paper/download/944/298 9. [ Links ]
10. Rojas Concepción AA, Guerra Chagime R, Guerra González Y, Hernández Peraza E, Forteza Padrino O. Factores asociados a la hipertensión arterial en adolescentes de San Juan y Martínez, 2018. Rev Cubana Salud Pública [Internet]. 2020 [citado 23/03/2021]; 46(4). Disponible en: Disponible en: http://www.revsaludpublica.sld.cu/index.php/spu/article/view/2174 10. [ Links ]
11 . Recinos Alejandro Pinot. Factores de riesgo cardiovascular, obesidad e hipertensión arterial en adolescentes de los establecimientos educativos públicos y privados del área urbana del municipio de Flores Costa Cuca del Departamento de Quetzaltenango.[Internet].2018 [citado 20/05/2021] Disponible en: Disponible en: https://glifos.umg.edu.gt/digital/48086.pdf [ Links ]
12. Landrove-Rodríguez O, Morejón-Giraldoni A, Venero-Fernández S, Suárez-Medina R, Almaguer-López M, Pallarols-Mariño E, et al. Enfermedades no transmisibles: factores de riesgo y acciones para su prevención y control en Cuba. RevPanam Salud Publica [Internet]. 2018 [citado 20/05/2021]; 42:e23. Disponible en: Disponible en: https://doi.org/10.26633/RPSP.2018.23 12. [ Links ]
13. Esquivel Lauzurique M, Rubén Quesada M, González Fernández C, Rodríguez Chávez L, Tamayo Pérez V. Curvas de crecimiento de la circunferencia de la cintura en niños y adolescentes habaneros. RevCubanaPediatr [Internet]. 2011 [citado 09/03/2021]; 83(1): 44-55. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75312011000100005&lng=es 13. [ Links ]
14. Mederico M, Paoli M, Zerpa Y, Briceño Y, Gómez-Pérez R, et al. Valores de referencia de la circunferencia de la cintura e índice de la cintura/cadera en escolares y adolescentes de Mérida, Venezuela: comparación con referencias internacionales Endocrinol Nutr [Internet]. 2013 [citado 09/03/2021]; 60(5): 235-242. Disponible en: Disponible en: http://dx.doi.org/10.1016/j.endonu.2012.12.003 14. [ Links ]
15. Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Volume 177. Human Kinetics Books. Champaign [Illinois]:1988. pp. 3-8. [ Links ]
16. Martínez MMLC, Blázquez GME, Hernández HME, et al. Índice cintura-talla: prueba para valoración de riesgo cardiovascular y diagnóstico del síndrome metabólico. Rev cubana med [Internet]. 2017 [citado 23/03/2021]; 56(2):109-118. Disponible en: Disponible en: https://www.medigraphic.com/pdfs/revcubmed/cm-2017/cm172c.pdf 16. [ Links ]
17. Tagle Rodrigo. Diagnóstico de Hipertensión Arterial. Rev. MED. CLIN. CONDES [Internet]. 2018 [citado 20/05/2021]; 29(1): 12-20. Disponible en: Disponible en: https://reader.elsevier.com/reader/sd/pii/S0716864018300099?token 17. [ Links ]
18. Cuba. Ministerio de Salud Pública. Hipertensión arterial. Guía para la prevención, diagnóstico y tratamiento [Internet]. La Habana: Editorial Ciencias Médicas; 2006. [citado 20/03/2021]. Disponible en: Disponible en: http://www.sld.cu/galerias/pdf/servicios/hta/guia_hta_cubana__version_final_2007revisada_impresa.pdf 18. [ Links ]
19. Pérez Caballero MD, León Álvarez JL, Dueñas Herrera A, Alfonzo Guerra JP, Navarro Despaigne DA, de la Noval García R, et al. Guía cubana de diagnóstico, evaluación y tratamiento de la hipertensión arterial. Rev cubana med [Internet]. 2017 Dic [citado 23/03/2021]; 56(4): 242-321. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232017000400001&lng=es 19. . [ Links ]
20. Real Delor RE, Duarte E, López N. Factores de riesgo cardiovascular en adolescentes de una ciudad del Paraguay. Encarnación (Paraguay) Acta Medica Colombiana [Internet]. 2017 [citado 23/03/2021]; 42(1). Disponible en: Disponible en: http://www.actamedicacolombiana.com/ojs/index.php/actamed/article/view/752 20. [ Links ]
21. Troche VM, Estrada PM, Quevedo MM. Hipertensión Arterial, enemigo silencioso en los adolescentes. Rev Ciencias Médicas [Internet]. 2018 [citado 23/03/2021]; 22(3): 466-475. Disponible en: Disponible en: https://www.medigraphic.com/pdfs/pinar/rcm-2018/rcm183f.pdf 21. [ Links ]
22. Amor M, Pronsky L, Irazabal C, Ortiz de Latierro S, et al. Detección de hipertensión arterial y su relación con otros factores de riesgo cardiovascular en adolescentes que concurren a realizar el apto físico escolar. Arch Argent Pediatr [Internet]. 2019 [citado 23/03/2021]; 117(5): 340-347. Disponible en: Disponible en: https://www.sap.org.ar/uploads/archivos/general/files_cb_amor_pdf_1563478135.pdf 22. [ Links ]
23. Cabal Giner MA, Herrera Gómez V, Díaz Ramírez N, González Gutiérrez J, Arias W. Sobre las asociaciones entre la obesidad y la hipertensión arterial en escolares cubanos. RCAN Rev Cubana Aliment Nutr 2018 [citado 20/05/2021] 28(1):95-106. Disponile en: http://www.revalnutricion.sld.cu/index.php/rcan/article/view/530/56823. [ Links ]
24. Chim AL, Medina IA, Medina JA, Yam AV, Candila JA. Factores de riesgo para diabetes e hipertensión arterial en adolescentes de Yucatán, México. Cuidarte [Internet]. 2019 [citado 20/03/2021]; 8(15): 67-79. Disponile en: Disponile en: http://dx.doi.org/10.22201/fesi.23958979e.2019.8.15.69158 24. [ Links ]
25. Acosta N, Guerrero T, Murrieta E, Alvarez L, Valle J. Niveles de presión arterial en niños y adolescentes con sobrepeso y obesidad en el noroeste de México. Enfermería Univ [Internet]. 2017 [citado 23/03/2021]; 14(3): 170-5. Disponible en: Disponible en: http://linkinghub.elsevier.com/retrieve/pii/S166570631730043X 25. [ Links ]
Received: July 09, 2022; Accepted: October 17, 2022











 texto en
texto en