Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 no.1 Pinar del Río ene.-feb. 2023 Epub 01-Ene-2023
Articles
Characterization of oral leukoplakia. Justo Ortelio Pestana Lorenzo Provincial Teaching Stomatology Clinic. 2019
1University of Medical Sciences of Sancti Spíritus "Justo Ortelio Pestana Lorenzo" Provincial Teaching Stomatology Clinic, Sancti Spíritus. Sancti Spíritus, Cuba.
2University of Medical Sciences of Sancti Spíritus. Sancti Spíritus, Cuba.
Introduction:
oral leukoplakia is a premalignant lesion that usually manifests as a white spot, but it is not usually painful and can go unnoticed.
Objective: to characterize oral leukoplakia in patients of the "Justo Ortelio Pestana Lorenzo" Provincial Teaching Stomatology Clinic during 2019.
Methods:
a cross-sectional descriptive observational study was conducted from January to December 2019 at the "Dr. Justo Ortelio Pestana Lorenzo" Provincial Stomatological Clinic. Twenty-one patients with oral leukoplakia who met inclusion criteria were selected. The variables studied were age, sex, skin color, risk factors and location of the lesion.
Results:
57,1 % of the patients with leukoplakia were between 45 and 59 years of age, 61,9 % were male and 47,6 % were of white skin color. 42,8 % of the area most affected was the mucosa of the cheek. Of the patients examined, 57,1 % were smokers and 28,8 % presented maladjusted prosthesis and deficient oral hygiene.
Conclusions:
patients between 45 and 59 years of age were predominant, with male sex and white skin color, the greatest localization in the mucosa of the cheek and the risk factors were smoking, poor oral hygiene and maladjusted prostheses.
Key words: LEUKOPLAKIA; RISK FACTORS; TOBACCO SMOKING; ORAL HYGIENE; DENTAL PROSTHESIS
INTRODUCTION
Cancer, in any of its variants and locations, constitutes a health problem for modern man, especially because it is a chronic disease, which increases proportionally.1
The worldwide incidence of lip and oral cavity cancer is estimated at four cases per 100,000 people, more common in men and the elderly, and differs according to socioeconomic status. The prevalence of this disease behaves dissimilarly in different continents; the annual incidence varies from two to four cases per 100,000 inhabitants in industrialized countries, and to 25 cases per 100,000 inhabitants in certain populations in Asia.2
In Cuba, cancer is among the first causes of death, with high prevalence in lips, oral cavity and pharynx. This disease is among the top ten locations and represents 4 % of all malignant lesions diagnosed. Cuba presents a pattern of incidence by location similar to that of developed countries, with exceptions such as the fourth place occupied by oral cavity neoplasms in the male sex, perhaps related to risk factors such as smoking and the ingestion of alcoholic beverages.3
The most effective measure to increase the cure of oral cancer is its primary prevention and early therapy as a consequence of a diagnosis of incipient lesions that is corroborated by a systematic and thorough examination. Early clinical detection of any lesion of the oral complex depends on the patient being examined early and the lesion being accurately diagnosed in that examination.4
The most common premalignant lesion of the oral cavity is leukoplakia, which appears in up to 60% of patients diagnosed with oral squamous cell carcinoma, which is the most frequent and whose presence is a marker of increased risk of oral cancer, is included among the new perspectives in the early diagnosis of this cancer.5
Leukoplakia is defined by the World Health Organization as a white plaque on the oral mucosa that cannot be removed by scraping or classified as any other diagnosable disease.The etiology of leukoplakia is associated with smoked or smokeless tobacco, alcohol, human papillomavirus infection, chronic irritation caused by poorly adapted prosthetic dentures, Candida albicans infection, Epstein-Barr virus, sun exposure, thermal irritants, traumatic irritants, poor oral hygiene, among other disorders.6
Leukoplakia is a frankly preneoplastic lesion, but there is no uniform criterion in the figures reported about its malignant transformation, these figures range from extreme values ranging from 4 % to 50 %. Santana reported that 7 % of malignant transformation and 12 % of keratosis, apparently not malignant, were in fact invasive carcinomas.7,8
The prevalence of oral leukoplakia varies considerably when comparing various countries, from 0,4 % to 17 %. In Eastern European countries, prevalences higher than 54 % have been reported. Leukoplakia has always been predominantly male, except in regions where women have a more frequent smoking habit than men. More than 75 % of oral leukoplakias are distributed in three sites: lip vermilion border or mucocutaneous line, cheek and gingiva.7
It is of great importance that stomatology professionals and students are scientifically prepared and have knowledge of oral pathology to understand the importance of early detection of potentially malignant lesions, timely diagnosis and effective treatment.9
Taking into account the increase in the incidence of these lesions in the oral complex, and the insufficient research approach to the problem in the territory, it was proposed to characterize oral leukoplakia in patients receiving stomatological care at the "Justo Ortelio Pestana Lorenzo" Provincial Teaching Stomatological Clinic during the year 2019.
METHODS
A cross-sectional descriptive observational study was carried out from January to December 2019at the "Justo Ortelio Pestana Lorenzo" Provincial Teaching Stomatological Clinic of Sancti Spíritus.
The 21 patients who attended the stomatological services of this unit and who met the following inclusion criteria were selected: any sex and age, with histological diagnosis of Leukoplakia.
The variables studied were: age, sex, skin color (white, black, mixed race), location of the lesion (lip, cheek mucosa, palate, alveolar ridge) and risk factors (smoking habits, alcohol, poor oral hygiene, thermal irritants, traumatic irritants, sun exposure, maladjusted prosthesis).
The data were recorded on a data collection form prepared by the authors. The simplified Oral Hygiene Index,10 was used to determine oral hygiene.
The patients were given a detailed explanation of the research and its objectives, prior to the application of the methods for obtaining information, in accordance with the ethical principles for medical research on humans: respect for persons, beneficence, non-maleficence and justice. The study was approved by the Ethics Committee of the institution where the research was carried out.
RESULTS
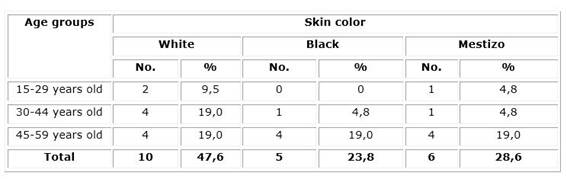
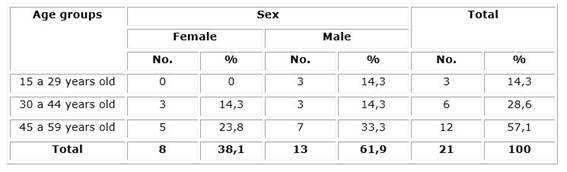
The predominant age group was 45-59 years with 57,1 % and the female sex with 59 % in relation to the male sex which was 41 %. The age group 35-59 years with 55,1 % was the most represented in both sexes (Table 1).
Table 1 Incidence of oral leukoplakia according to age group and sex. Provincial Teaching Stomatological Clinic. "Justo Ortelio Pestana Lorenzo".
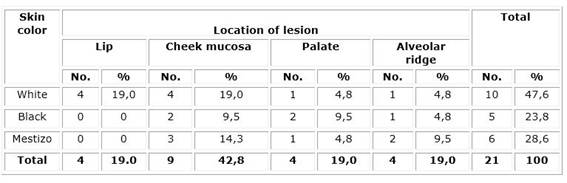
In the sample there was a predominance of patients with white skin color with 47,6 % in the age groups 30-44 years and 45-59 years, followed by mestizo with 28,6 %. (Table 2).
The most frequent location of oral leukoplakia in the study patients was the mucosa of the cheek, with 42,8 % and white skin color in 47,6 % (Table 3).
57,1 % of the patients were smokers and 28,8 % presented maladjusted prostheses and poor oral hygiene (Table 4).
DISCUSSION
The predominance of the age group 45 to 59 years old, white skin color and male sex in the present investigation coincides with that obtained by Milanés A, et al.7) Carmona M, et al.11and Guerrero M, et al.12) However, Garcia Yet al.13) found a greater number of patients aged 60 years or older and a predominance of female sex by Batista M, et al.4 and González E, et al.14
The association between the appearance of these lesions and the preponderance of the male sex and skin color is reported in the studies of Valentín F, et al.15
The most frequent location of leukoplakia in the cheek mucosa coincides with several studies.7,9,15 The same occurred with the higher incidence of tobacco consumption, as reported by Cardentey J, et al.16 who mentioned it as the main risk factor in 55,5 % of the patients inspected.
The harmful effect of tobacco on the oral mucosa is due to the fact that it contains some 300 carcinogenic substances that are converted into active metabolites capable of interacting with DNA by the action of oxidative enzymes, among which nicotine, arsenic, methanol, ammonium, cadmium, carbon monoxide, formaldehyde, butane and hydrogen cyanide stand out. In addition to the action of carcinogens, exposure to heat maintained by tobacco combustion can aggravate oral mucosal lesions.1,17)
We also agree with the results of Milanés A, et al.7) where the risk factors that predisposed to leukoplakia were poor oral hygiene, smoking and traumatic irritants.
González E, et al.14 identified the ingestion of alcoholic beverages as the risk factor with the highest percentage in their population (63 %), stating that alcohol exerts a caustic effect increasing the permeability of the oral mucosa and allowing the passage of other carcinogens such as tobacco, followed by smoking (60,9 %) and the use of maladjusted prostheses (43,5 %).
The influence of deficient oral hygiene in the presence of leukoplakia is also identified by Quintanilla Cl, et al.,17 Santana Garay8 points out that this is one of the most common risk factors and relates it to the accumulation of dentobacterial plaque which, by forming tartar, mechanically inflames the gums, causes bacteria and their toxins to infect them and diminishes the host's response to bacterial infections.
The results of the study differ from those found by Pérez Y, et al.,18) where the ingestion of hot food predominated among the risk factors when it was identified in 55 patients.
The authors consider it necessary to apply educational intervention strategies in the population to raise the perception of risk for oral cancer. The study is limited by the small size of the patient selection. It is suggested to study the association between the variables analyzed in this study.
BIBLIOGRAPHIC REFERENCES
1. Yero-Mier I, Rodríguez-Pimienta E, Pérez-García L, de-Castro-Yero J. Conocimiento sobre prevención del cáncer bucal y factores de riesgo presentes en el adulto mayor. Medimay [Internet]. 2022 [citado 28/07/2022]; 29(1): [aprox. 7 p.]. Disponible en: Disponible en: http://www.revcmhabana.sld.cu/index.php/rcmh/article/view/1933 1. [ Links ]
2. Bray F, Ferlay J, Soerjomataranm I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin [internet] 2018 nov (citado 20/03/2022); 68(6): 394-424. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/30207593/ 2. [ Links ]
3. Ministerio de Salud Pública. Dirección de Registros Médicos y Estadística de salud. Anuario Estadístico de Salud 2020 [Internet] 2021 [citado 23/03/2022]. Disponible en: Disponible en: https://salud.msp.gob.cu/wp-content/Anuario/Anuario-2020.pdf 3. [ Links ]
4. Batista Vila M, González Ramos R, Batista Bochs M, Mesa Mendiola I. Lesiones bucales diagnosticadas por Programa de Detección del Cáncer Bucal. Facultad de Estomatología. La Habana. 2015-2016. Medimay [Internet]. 2020 [citado 11/03/2022]; 27(1) :[aprox. 9 p.]. Disponible en: Disponible en: http://revcmhabana.sld.cu/index.php/rcmh/article/view/1564 4. [ Links ]
5. Toledo Cabarcos Y, Suárez Sori B, Mesa López A, Albornoz López del Castillo C. Caracterización clínico e histopatológica de la leucoplasia bucal. AMC [Internet]. 2018 [citado 08/03/2022]; 22(4): [aprox. 11 p.]. Disponible en: Disponible en: http://www.revistaamc.sld.cu/index.php/amc/article/view/5405 5. [ Links ]
6. López-Castro JG, Guzmán-Gastélum D, Espinosa-Cristóbal LF, Cuevas-González JC, Tovar-Carrillo KL, Reyes López SY, Donohue-Cornejo A. Lesiones potencialmente malignas de la cavidad bucal. Revista de ciencia y tecnología de la UACJ. [Internet]; 2021 [citado 07/03/2022]; (suppl 1). Disponible en: https://erevistas.uacj.mx/ojs/index.php/cienciafrontera/article/view/3594/32666. [ Links ]
7. Milanés Chalet A, Rogert Alcolea I, Pérez Milán A, Palomino Rodríguez K, Beatón Sablón A. Factores de riesgos asociados con leucoplasia bucal en pacientes del consultorio 43. Ciro Redondo. Bayamo. 2017. MULTIMED [Internet]. 2018 [citado 07/03/2022]; 22(2): [aprox. 15 p.]. Disponible en: Disponible en: http://www.revmultimed.sld.cu/index.php/mtm/article/view/839 7. [ Links ]
8. Santana Garay JC. Prevención y diagnóstico del cáncer bucal. La Habana: Editorial Ciencias Médicas; 2017. [ Links ]
9. Hernández Cuétara L, Ramírez Ramírez R, Serrano Díaz B, Fernández Queija Y. Lesiones cancerígenas y precancerosas bucales. Factores de riesgos asociados. Policlínico Bernardo Posse. Año 2017. Rev.Med.Electrón.[Internet]. 2019Jun [citado 25/02/2022];41(3): 618-627. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242019000300618&lng=es 9. . [ Links ]
10. Colectivo de autores. Compendio de Periodoncia. -2. ed. -La Habana: Editorial Ciencias Médicas ; 2017. Disponible en: http://www.bvscuba.sld.cu/libro/compendio-de-periodoncia/ [ Links ]
11. Carmona Lorduy M, Pimienta Vásquez L, Pérez Martínez M, Porto Puerta I. Caracterización epidemiológica de pacientes fumadores invertidos en Cartagena, Colombia. Acta Odontológica Colombiana[Internet]. 2019 Abr [citado 20/04/2022]; 9(2): 47-58.Disponible en: Disponible en: https://www.redalyc.org/journal/5823/582361537004/html/ 11. [ Links ]
12. Guerrero Brito M, Pérez Cabrera D, Hernández Abreu NM. Lesiones bucales premalignas en pacientes con hábito de fumar. Medicentro Electrónica[Internet]. 2020 Mar [citado 19/04/2022];24(1): 159-164. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30432020000100159&lng=es 12. . [ Links ]
13. Garcia Molina Y, González Lara M, Crespo Morales A. Lesiones premalignas y malignas en el complejo bucal en La Palma, Pinar del Río. Rev Ciencias Médicas[Internet]. 2018 Dic [citado 25/02/2022]; 22(6): 61-69. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-31942018000600061 13. [ Links ]
14. González Crespo E, Martínez Alonso L, Labrador Falero D M. Intervención educativa sobre cáncer bucal en pacientes adultos mayores en Santa Inés, Venezuela. Rev Ciencias Médicas [Internet]. 2021Jun [citado 25/02/2022]; 25(3): e4836. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-31942021000300002&lng=es 14. [ Links ]
15. Valentín González F, Rodríguez González G M, Conde Suárez H F, Vila Morales D. Caracterización del Cáncer Bucal. Estudio de 15 años. Rev.Med.Electrón. [Internet]. 2017Abr [citado 20/04/2022]; 39(2): 245-258. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242017000200010&lng=es 15. . [ Links ]
16. Cardentey-García J, Gonzalez R, González-García X. Enfermedades bucales premalignas en adultos mayores del Policlínico Universitario Pedro Borrás Astorga, Pinar del Río, Cuba. Correo Científico Médico [Internet]. 2019 [citado 19/04/2022]; 23(3) Disponible en: Disponible en: http://www.revcocmed.sld.cu/index.php/cocmed/article/view/2738 16. [ Links ]
17. Quintanilla Domínguez C, Toledo Reyes L, Hernández Abreu N , Pérez Álvarez R, González González B, Hernández Pérez M A. Programa educativo para la prevención del cáncer bucal desde la adolescencia. EDUMECENTRO[Internet]. 2019 Mar [citado 01/03/2022]; 11(1): 87-104. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2077-28742019000100087&lng=es 17. [ Links ]
18. Pérez-Reyes Y, Bermúdez-Núñez Y. Factores de riesgo asociados al cáncer bucal en pacientes de un consultorio médico de la familia. Revista Electrónica Dr. Zoilo E. Marinello Vidaurreta [Internet]. 2020 [citado 01/03/2022]; 45(5). Disponible en: Disponible en: http://revzoilomarinello.sld.cu/index.php/zmv/article/view/2172 18. [ Links ]
Received: June 27, 2022; Accepted: November 18, 2022











 texto en
texto en