Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 supl.1 Pinar del Río 2023 Epub 01-Jul-2023
Articles
Temporomandibular joint dysfunction in patients post orthodontic treatment
1Autonomous Regional University of the Andes, Santo Domingo. Ecuador.
ABSTRACT Introduction: possible temporomandibular disorders that may occur after an orthodontic procedure are more common than has been investigated. Objective: To determine the correlation between orthodontics and temporomandibular joint (TMJ) dysfunctions in patients aged 14-22 years. Methods: An observational, descriptive and cross-sectional study was conducted to determine the correlation between orthodontics and temporomandibular joint (TMJ) dysfunctions in patients between 14 and 22 years of age, Santo Domingo, Ecuador, in the period 2020 - 2022. The universe consisted of 63 patients, the sample obtained by simple random sampling and the inclusion-exclusion criteria consisted of 42 patients. Results: 63,28 % of the study population was female and 36,62 % was male. Fifty-four percent of the patients surveyed had little pain, 32 % reflected in the surveys that their pain was mild and only 9 % had severe pain. Thirty-six per cent of the patients reported that they never felt their jaw "locked" and 37 % rarely. Conclusions: orthodontics is not the definitive treatment for temporomandibular disorders; there is a relationship between them and orthodontics, yes, but it is a treatment for very specific cases, where temporomandibular disorders are caused by malocclusion. For disorders of other origin, another type of treatment or a mixture of several of these is necessary.
Key words: Temporomandibular Joint; Orthodontics; Dental Occlusion; Orofacial.
INTRODUCTION
Considering that the aim of this research has a specialised orientation, it was found that there is little research of this nature in the country and internationally. This gives significant importance to this research because it is pioneering in this field under the conditions that have been proposed.
The possible temporomandibular disorders that can occur after an orthodontic procedure are more common than is believed, however, they are often ignored by the affected patients and the professionals who carry out the orthodontic plan, as the information available to solve this problem is scarce. The fundamental problem lies in the identification of a direct relationship between orthodontics and TMJ problems or disorders, analysing the bibliographic information that supports both points of view.
The TMJ is a synovial joint made up of four articular surfaces: the glenoid fossa located in the temporal bone, the superior and inferior compartments which are divided by the articular disc and the condyle of the mandible. The articular disc is attached to the capsule between the condyle of the mandible and the glenoid cavity, which is lined by a membrane that secretes the synovial fluid necessary for its lubrication. It plays an essential role in guiding jaw movement and distributing the stresses produced by everyday tasks such as chewing, swallowing and speaking.1,2
As a joint with such particular characteristics, we know how important it is as a specific element. The care and disorders it can present are very specific due to its condition and the elements it possesses. In addition, if we consider the constant work that this joint carries out, we can infer that it is subject to a number of potential damages, and that these can degenerate the state of the patient's oral and general health.
Temporomandibular disorders (TMD) are the major cause of non-dental pain in the orofacial region. According to studies related to the number of people presenting with these conditions, we find that they account for 10-15 % of cases of TMD in adults, of which only 5 % seek treatment. In addition, the incidence peaks between 20 and 40 years of age and is more common in women.3
Temporomandibular disorders are degenerative musculoskeletal conditions associated with morphological and functional deformities. TMDs include abnormalities of position and/or intra-articular disc structure, as well as dysfunction of the associated musculature. Symptoms and signs include clicking sounds presenting with joint pain, restriction or deviation of range of motion, cranial and/or muscular pain known as orofacial pain.4
When a patient presents with damage to both the muscles and bony structures related to jaw movements, we have a temporomandibular joint disorder. This damage is usually evident in the areas directly related to the joint and internally. The most common damage is related to when the disc is displaced outside the glenoid cavity and when it is repositioned, it emits a clicking sound, evidencing the presence of damage to the TMJ.
There are several reasons that can generate a TMD, among them may be a genetic issue. This develops due to damage to one of the chromosomes and is caused by poor formation during pregnancy. One of these disorders or malformations is called Pierre Robin Syndrome, which consists of mandibular hypoplasia and a malpositioning of the tongue.5
Studies have shown that malocclusion can cause displacement of the TMJ structures, specifically the mandibular condyle, suggesting a need to correct the position of the teeth to alleviate the symptoms that TMDs can cause. As a result of this association, orthodontic treatment can be seen as a preventive and curative tool, achieving harmony and a correct skeletal-occlusal relationship.6
However, there are various opinions on the actual factors that will determine whether a patient is likely to develop TMD. For example, a patient with a type II bite, or deep bite, is more likely to develop TMD than a patient with an open bite. In addition, it is mentioned that an adult patient with disharmonious occlusion may only develop symptoms, but not a disorder as such. We know then, that TMD is a multifactorial pathology and demonstrating its direct relationship with one of its variables, such as occlusion, is a difficult task when the necessary studies and equipment are not available.7
Due to the various factors that influence the development of TMD, it has become a difficult task to determine the origins of this problem. We know that a patient with malocclusion is more likely to develop TMD than a patient without malocclusion. However, a patient with childhood respiratory problems is also more likely to have a certain weakness or tendency to suffer TMJ damage.
Among the most common disorders that we can find, we have the ankylosis of the TMJ. This corresponds to a disorder classified as mandibular hypo-mobility. The literature defines this as an abnormality of jaw movement that leads to a restriction of the mouth opening with reduced mouth movement, and that can end, if not followed, in the form of a reduced jaw movement.
Among the most common disorders that we can find, we have the ankylosis of the TMJ. This corresponds to a disorder classified as mandibular hypo-mobility. The literature defines this as an abnormality of mandibular movement that leads to a restriction of the buccal opening with reduced buccal movement, and which can end, if not treated, in an absolute loss of mobility.8
The future of the relationship between TMJ and orthodontics is based on prevention. This is supported by tools such as radiographs that help us to deepen our knowledge of the patient's condition. In this way the orthodontist will be able to carry out the appropriate treatment on a patient at risk of developing TMD, and thus complete the process correctly.9
It must be considered that, since these disorders and dysfunctions are multifactorial, the study for the solution of each one of them must be exhaustive, and several factors must always be considered in order for the treatments to be efficient.
Thanks to new research, we now know that malocclusion, although it is true that it is a factor that can influence the appearance of TMD, is not a determining factor, as was believed in the eighties of the 20th century. At that time, orthodontics was considered to be the best solution, and it still is, although we know that malocclusion is not a determining factor. After the 2000s until 2010, more invasive surgical procedures were used as the last option to correct disorders in this area.10
Since 2010, a paradigm shift has emerged that has led to a new vision and approach to TMJ treatment. This paradigm is constantly advancing and growing due to the constant new research that continues to be developed on this subject. Considering a treatment related to "behavioural therapies". All of this is linked to the development of advances in neuroscience and biopsychosocial diagnostic and treatment models.10
Physical therapy has been used for decades for the treatment of cranio mandibular disorders using thermal packs, cooling steam and supra cutaneous electro-nerve stimulants. A study in England found that, despite limited evidence, 72 % of patients treated considered physical therapies to be effective. To a degree of efficiency, jaw exercises were found to be 79 % effective and acupuncture 42 % effective. This resulted in a significant reduction of neck and back pain.11
METHODS
The study had a correlational scope, as the bibliography was reviewed with information on the subject, seeking to determine whether there is a direct relationship between orthodontics and TMD (Temporomandibular Disorder). It is transversal, being delimited by a specific period of time, taking into account from 2020 to 2022. Non-experimental research design, as it will not be involved with concrete actions that affect the participants and subjects of the study.
The universe consisted of 63 patients, the sample obtained by simple random sampling and the inclusion-exclusion criteria consisted of 42 patients.
A 7-question survey was administered to patients who underwent orthodontic treatment, and to those who are currently undergoing treatment, at the Design Dental dental office during the period from 2020 to 2022 in Santo Domingo, Ecuador.
An interview was also conducted with orthodontic dentists to identify the frequency of patients who have presented a TMD prior to orthodontic treatment, whether the existence of such disorders is correctly assessed and whether this procedure can correct or worsen this condition. They were asked for their opinion on whether they consider orthodontics as a definitive treatment for TMDs. Each doctor was interviewed separately, so as not to contaminate the ideas of one doctor with the opinions of the others.
Among the variables, the following were considered: joint noises presented together with jaw movements, considered as a sign, joint pain on palpation of the TMJ area, considered as a symptom, traumatic history, maximum mouth opening, type of dentition, mandibular deviation, previous dental treatment, craniofacial anomalies, tongue projection and bruxism.
Responses were tabulated using Microsoft Excel, and patient surveys were sent using Google forms.
The ethics committee of the institution was informed about the development of the research, the documentary nature of the data collection as well as the respect for the individuality of the patients; furthermore, the main results will only be used for scientific purposes taking into account the Declaration of Helsinki.
RESULTS
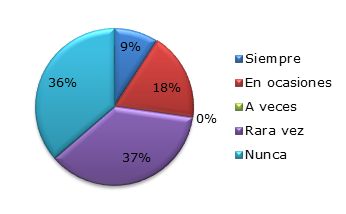
54 % of the patients surveyed had little pain, 32 % reported mild pain and only 9 % had severe pain (Graph 1).
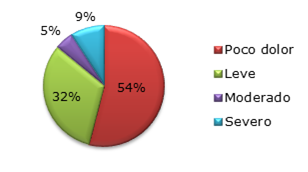
Graph 1 Level of TMJ pain. Obtained through patient survey. Dental office "Design Dental" during the period from 2020 to 2022 in Santo Domingo - Ecuador.
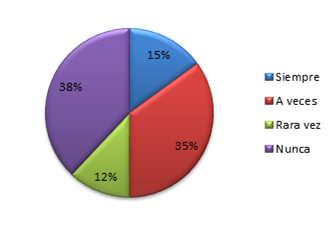
In the only cases where a group of different values was evident, were the values in relation to the question about whether the jaw was locked. Here we can see that 36 % of the patients never have this discomfort and 37 % rarely.(Graph 2)
It was shown that 38 % of the patients did not present pain or sounds in their TMJ ever, however, the sum of those who do present pain sometimes and always corresponds to 50 %, that is, we can determine that more than 50 % of the patients still require treatment to correct the TMDs, either at an early stage of these TMDs so that they do not develop and can become even more complicated (Graph 3).
DISCUSSION
It was found that there is a direct relationship between the studies carried out since 2010 by Gil-Martínez,10 and Vélez and et al,12 which state that orthodontics is not a definitive method, and that malocclusion is not the most influential factor in the existence of any type of temporomandibular joint disorder.
According to Santana MR,13 as stated in their article on treatments for damage to the temporomandibular joint, orthodontics is one of the treatments that can solve this problem, but in any case it is not the only one that can be used, especially when inflammation is present, for which they recommend maintaining a white diet and temporarily limiting masticatory movements.
It is evident how this response is related to what the interview revealed, where it is considered that orthodontics is the most effective treatment for this problem.
It became clear how this response is related to what the interview revealed, where orthodontics is considered to be one of several treatments that can be used to correct TMJ problems. It is not the definitive treatment, but it is one of the recommended treatments depending on the disorder present.
On the other hand, there are considerations by and Vélez and et al,12 who recommend physiotherapy to prevent students or workers, especially women between 25 and 35 years of age who suffer more from this condition, in relation to absences from work and studies. Taking into consideration that TMDs are found in 70 to 90 % of the general population.
There are several positions as to whether malocclusion and its solution with orthodontics and TMDs have a direct correlation. While it is true that there is no scientific rigour to define this definition and correlation as absolute, we do have the opinion of Luther, who suggests that the problems of malocclusion and TMDs will be solved with orthodontics.14 We can note that in older publications orthodontics was considered to be the definitive treatment for TMDs, and that malocclusion was a determining factor at the time of presenting these disorders.
Based on the findings of this research, it was found that orthodontics can be determined to be the definitive treatment for TMDs, and it is being put together with the results of current research on this topic. While it is feasible to say that orthodontics can help with certain types of disorders, it is not a definitive treatment. While this is true, it is acceptable to define orthodontics as a very viable and plausible treatment, even though it is necessary to have a more specific study in relation to the patient who is going to have the treatment.
It can be noted that in this research there is a certain relationship with what has been said before, we can see that 40 % of the patients who have undergone orthodontic treatment do not present pain or discomfort in their TMJ, however, 60 % do have some affectation, even presenting very intense pain, qualified by themselves with a 5/5.
We can see that the patients who still have pain in their TMJ and who may develop TMD are 60 % of those who have undergone orthodontics. Thus relating the results of the survey with the interview with the doctors specialising in orthodontics, where they mentioned that this treatment can be one of the many occasions to help TMJ problems or disorders of this joint.
In the interview with the doctors, the idea of whether malocclusion is directly proportional to TMD is clarified, and we can see that this is not the case, that although it is true that it is one of the influential factors, this is not going to determine that the patient who presents a malocclusion is necessarily going to have a TMD. In our results we found that 60 % of patients already have a good occlusion and still have jaw discomfort, or if they feel their bite is incorrect, or they already have the characteristic clicking sound of the articular disc repositioning, synonymous with a previous step to a TMJ disorder.
CONCLUSIONS
It was defined that malocclusion is not a definitive reason that will necessarily lead to temporomandibular joint problems or disorders. It is rather one of the multiple factors that can generate wear and tear or alteration of the temporomandibular joint. As could be seen in this research, only 30 % of patients who finished their orthodontic treatment do not report any discomfort or pain in their joint.
BIBLIOGRAPHICAL REFERENCES
1. Stoll ML, Kau CH, Waite PD, Cron RQ. Temporomandibular joint arthritis in juvenile idiopathic arthritis, now what? Pediatric Rheumatology[Internet]. 2018[cited 01/03/2023]; 16(1). Available from: Available from: http://dx.doi.org/10.1186/s12969-018-0244-y 1. [ Links ]
2. Murphy MK, MacBarb RF, Wong ME, Athanasiou KA. Temporomandibular Joint Disorders: A Review of Etiology, Clinical Management, and Tissue Engineering Strategies. Int J Oral Maxillofac Implants[Internet]. 2013 Nov.-Dic[cited 01/03/2023]; 28(6): e393-e414. Available from: Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4349514/ 2. [ Links ]
3. Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. AFP [Internet]. 2015 [cited 01/03/2023]; 91(6): 378-86. Available from: Available from: https://www.aafp.org/pubs/afp/issues/2015/0315/p378.html 3. [ Links ]
4. Crespo Peréz M. Trastornos de la articulación temporomandibular, tratamientos fisioterapéuticos una revisión sistemática[Internet]. 2021 [cited 01/03/2023]. Repositori URV. Ciències de la salut Health sciences Ciencias de la salud. Available from: Available from: https://repositori.urv.cat/estatic/TFG0011/en_TFG3550.html 4. [ Links ]
5. Bush PG, Williams AJ. Incidence of the Robin Anomalad (Pierre Robin syndrome). Br J Plast Surg [Internet]. 1983 [cited 01/03/2023]; 36(4): 434-7. Available from: Available from: https://www.jprasurg.com/article/0007-1226(83)90123-6/pdf 5. [ Links ]
6. Michelotti A, Rongo R, D’Antò V, Bucci R. Occlusion, orthodontics, and temporomandibular disorders: Cutting edge of the current evidence. J World Fed Orthod [Internet]. 2020[cited 01/03/2023]; 9(3 Supl): S15-S18. Available from: Available from: https://www.sciencedirect.com/science/article/pii/S2212443820300436 6. [ Links ]
7. Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil [Internet]. 2010[cited 01/03/2023]; 37(6): 411-29. Available from: Available from: http://dx.doi.org/10.1111/j.1365-2842.2010.02087.x 7. [ Links ]
8. García S, Vanessa D. Alto rendimiento en deportistas: boxeo, y su relación con trastornos de la articulación temporomandibular. concentración deportiva de Pichincha. Periodo Marzo-Junio 2015. Quito: UCE; 2015. [ Links ]
9. Villar C, Jeremy M. Tratamiento en pacientes con disfunción temporomandibular; 2021. [ Links ]
10. Gil-Martinez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res [Internet]. 2018 [cited 01/03/2023]; 11: 571-87. Available from: Available from: http://dx.doi.org/10.2147/jpr.s127950 10. [ Links ]
11. Armijo-Ikuvo S, Oitance L, Singh V, Neto F; Thie N, Michelotti A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis [Internet]. Physical Therapy11. . 201611. [cited 01/03/2023]; 96(1): 9-25 Available from: Available from: https://academic.oup.com/ptj/article/96/1/9/2686339?login=false 11. [ Links ]
12. Vélez Uribe JD, Vélez LC, Pérez Mejía M, Barragán KA. Síndrome de disfunción de la articulación temporomandibular y el papel de la educación en su tratamiento[Internet]. CES Movimiento y Salud. 2015 [citado 01/03/2023]; 3(1): 44-52. Disponible en: Disponible en: https://revistas.ces.edu.co/index.php/movimientoysalud/article/view/3352 12. [ Links ]
13. Santana MR, Grau León IB, Chala YM, Salso Morell RA. Evaluación de un protocolo para el diagnóstico y tratamiento de los trastornos inflamatorios temporomandibulares. Revista Electrónica Dr. Zoilo E. Marinello Vidaurreta [Internet]. 2015 [citado 01/03/2023]; 40(5). Disponible en: Disponible en: https://revzoilomarinello.sld.cu/index.php/zmv/article/view/64 13. [ Links ]
14. Luther F. Orthodontics and the temporomandibular joint: Where are we now? Part 1. Orthodontic treatment and temporomandibular disorders [Internet]. 1998[citado 01/03/2023]; 68(4): 295-304. Available from: Available from: https://meridian.allenpress.com/angle-orthodontist/article/68/4/295/57194/Orthodontics-and-the-temporomandibular-joint-Where 14. [ Links ]
Received: June 15, 2023; Accepted: June 16, 2023











 texto en
texto en