Introduction
Cerebrovascular disease is an important and well-studied health problem; it has been the leading cause of disability, the second of dementia, and the third of death in developed and developing countries for decades (Roger et al., 2011; Amarenco et al., 2009; González et al., 2016).
Of the multiple classifications, due to its value in clinical practice the one based on its nature, ischemic or hemorrhagic remains.
Ischemic cerebrovascular disease is the most frequent, 80% of strokes are of this nature, where the cardio-embolic etiology represents 20% (Piloto et al, 2015), although other studies offer figures of up to 34% (Diaz, 2012).
This subgroup of patients usually presents high mortality and high recurrence rate, approximately 12% in the first three months (Piloto et al, 2015).
Multiple tools are usually very useful for diagnosis, including echocardiographic studies, neurosonological studies of the neck arteries, electrocardiogram, continuous cardiovascular monitoring by Holter, whose usefulness has been demonstrated in at least 20% of the causes of cardio-embolic stroke (Díaz, 2012; Piloto et al, 2015).
Embolisms of cardiac origin are responsible for up to 15-30% of cerebral ischemic attacks (Morady & Zipes, 2016; Ferro, 2003).
The transthoracic echocardiogram and the trans esophageal echocardiogram play a role fundamental in the evaluation, diagnosis and management of the embolic source (Sacco et al, 2006; Arias et al, 2013).
In 2010, the European Society of Echocardiography published the recommendations for the use of echocardiography in the identification of potential embolic sources as a cause of ischemic stroke in the absence of another cerebrovascular disease. According to these recommendations, embolic sources can be classified into major and minor, and from a pathophysiological point of view into 3 categories: cardiac lesions prone to thrombus formation (such as atrial fibrillation and appendicular thrombus), cardiac masses and paradoxical embolisms through a patent foramen ovale (Pepi et al, 2010).
We define stroke with a cardio-embolic profile as an infarct generally of medium size (1.5 to 3 cm) or large (> 3 cm), with cortical topography, with onset of symptoms in wakefulness, instantaneous presentation (in minutes) or acute (in hours) of neurological focus and maximum neurological deficit in the first hours. Although it is true that on many occasions it is difficult to differentiate it from other embolic causes, some tools such as the echocardiogram play a fundamental role in the study of these patients.
On the other hand, diagnostic techniques such as computed tomography and magnetic resonance imaging also contribute to defining the mechanism. (Sacco et al, 2006; Pepi et al, 2010; Arias et al, 2013). However, due to population aging and greater number of comorbidities, it is not uncommon to find patients in which several pathogenic mechanisms coexist (Arboix et al, 2006).
The Institute of Neurology and Neurosurgery of Cuba, due to its status as institution in specialized care for this branch, is the recipient of a great diversity of patients with cerebrovascular disease, usually of doubtful etiology due to their forms of presentation, which requires the implementation of exclusive protocols for studies that include from the beginning the echocardiogram, neurosonology studies and fine-tuned hemochemistry for the early detection of specific markers that allow us to define the etiology and thus improve the conduct and proper use of diagnostic tools.
The general objective of this study was to define the value of transthoracic echocardiography, neuronological and biological markers in the differential diagnosis of ischemic stroke and the specific objectives was to identify socio-demographic variables and risk factors and to determine the behavior of the biological, neurological, electrocardiographic and echocardiographic variables according to the type of stroke.
Materials and Methods
Study design: It is a descriptive and observational study based on data obtained from the medical records of patients discharged with the diagnosis of ischemic cerebrovascular disease at the National Institute of Neurology Neurosurgery of Cuba in the period from January 2017 to December 2019.
The universe of study is made up of patients treated for presenting at least one ischemic stroke in this period both in the outpatient area provided by the Cerebrovascular Disease working group of this Institute as well as patients with the same diagnosis hospitalized in the stroke room of the Institute who have undergone as part of the investigations: transthoracic echocardiography, carotid and vertebral Doppler.
Inclusion criteria: Patients having suffered at least one ischemic stroke in the period studied, both sexes, which expressed their desire to participate in the research by signing the informed consent.
Exclusion criteria: Patients who suffered exclusively hemorrhagic stroke, patients in which transthoracic echocardiographic study and/or Doppler study of the supra-aortic trunks have not been performed.
Methods: The medical records of the patients treated for cerebrovascular disease in the stroke room and in the neurovascular group consultations were analyzed to select the patients who met the inclusion criteria.
The markers studied in all included patients were checked in the same period, during admission, after the event occurred.
The study includes 127 medical records of patients with the diagnosis of ischemic cerebrovascular disease, selecting a total of 79 records of patients who had undergone transthoracic echocardiography and ultrasound Doppler of the neck arteries.
Information was collected on socio-demographic variables of age, gender, established vascular risk factors such as arterial hypertension, diabetes mellitus, previous cerebrovascular disease, heart failure, old myocardial infarction, paroxysmal or permanent atrial fibrillation as a medical history referred to in the medical history; Atrial fibrillation diagnosed on admission by electrocardiogram, electrocardiographic Holter, or continuous hemodynamic monitoring, other electrocardiographic data demonstrating left ventricular hypertrophy, or left bundle branch block.
The data obtained in the transthoracic echocardiogram were recorded as diameters of the interventricular septum, diameters of cavities, hypokinesis of the wall or interventricular septum, calculation of ventricular function by Teich, search for thrombi in cavities, aneurysm of the interatrial septum and/or patent foramen ovale, valve alterations, related to embolic pathologies.
Variables obtained by ultrasound of the neck arteries were also studied, referring to the existence or not of carotid atheromatosis and the percentage of stenosis, in addition to the values of serum cholesterol and triglycerides levels as well as renal functional tests, all the variables analyzed were compared according to type of stroke.
The examinations (Ultrasound, Doppler, Echocardiogram, Electrocardiographic) were performed on an Alpha 5 Aloka Equipment, located in the Institute's Imaging Department.
Statistical analysis: A description of the demographic characteristics was made and it was planned that the quantitative variables would be presented as mean ± standard deviation if their distribution was normal, or as medians and interquartile range in those whose distribution did not meet the normality criteria.
Normality was evaluated with the Shapiro-Wilk/Kolmogorov-Smirnov test and its distribution in the population was evaluated with the Student's t test for means and with the Mann-Whitney test for medians. The qualitative variables were expressed as percentages.
The outcome of the study was compared using the Fisher's Exact Probability Test, p values less than 0.05 were considered significant. Data analysis was performed with Stata 12 software.
Results
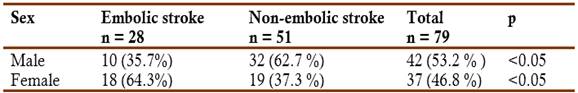
Of the 79 clinical histories evaluated, 35.44% (n=28) were embolic strokes, while the remaining 51 cases (64.6%) were non-embolic, Males predominated (53.2%) in the entire sample.
The analysis by sex and etiology (Table 1) showed a predominance of the female sex (64.3%) in patients who suffered cardio-embolism, while in non-embolic patients the male predominated (62.7%). This relationship was significant (p<0.05) for both groups.
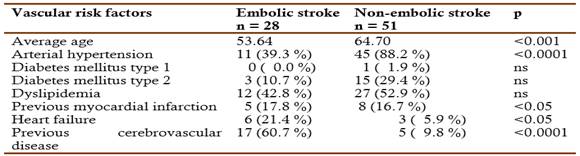
The vascular risk factors found in the study shown in the Table 2. The arterial hypertension related with the 88.2% of non-embolic strokes and with 39.3% of embolic stroke (p<0.0001).
Type 1 diabetes mellitus does not appear in cases of embolic strokes and only one case in non-embolic ones. Type 2 diabetes mellitus with 3 (10.7%) in embolic and 15 (29.4%) in non-embolic, dyslipidemia with 12 (42.8%) in embolic and 27 (52.9%) in non-embolic, non-significant differences.
The previous myocardial infarction related with 5 (17.8%) in the embolic and 8 (16.7%) in the non-embolic, non-significant differences. Previous cerebrovascular disease occurs in 17 (60.7%) of the embolic and in 5 (9.8%) of the non-embolic (p<0.0001).
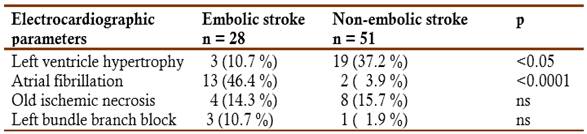
The electrocardiographic parameters sought in the series: left ventricular hypertrophy occurs in 3 (10.7%) of the embolic and in 19 (37.3%) of the non-embolic (p<0.05); atrial fibrillation occurs in 13 (46.4%) of the embolic and in 2 (3.9%) of the non-embolic (p<0.0001). Old ischemic necrosis and left bundle branch block did not show statistical significance in our series (Table 3).
In the echocardiographic studies of the variables analyzed by frequency and by hundreds (Table 4), it was obtained that 4 (14.3%) of the embolic patients presented dilatation of the left ventricle, and 0 in the non-embolic (p<0.01), the dilation of the left atrium appears 8 (28.6%) of the embolic and in 2 (3.9%) of the non-embolic (p<0.01); mitral calcification was found in 11 (39.3%) in embolic cases and 5 (9.8%) in non-embolic cases (p<0.01); mitral valve prolapse was observed in 7 (25%) of the embolic and in 0 of the non-embolic (p<0.001).
The atrial septum aneurysm is seen in 4 (14.3%) of the embolic and in 0 of the non-embolic (p<0.01); patent foramen ovale was seen in 2 (7.1%) of the embolic and in 0 of the non-embolic (p<0.05). Grade 1 diastolic dysfunction of the left ventricle is observed in 9 (32.1%) of the embolic and in 38 (74. 5%) of the non-embolic (p<0.001).
Finally, left ventricular hypertrophy was diagnosed in 6 (21.4%) of the non-embolic and in 32 (62.7%) of the non-embolic (p<0.001), and mitral regurgitation 7 (25%) in embolic patients and 4 (7.8%) in non-embolic patients (p<0.05).
Table 4 Variables of transthoracic echocardiogram and stroke profile
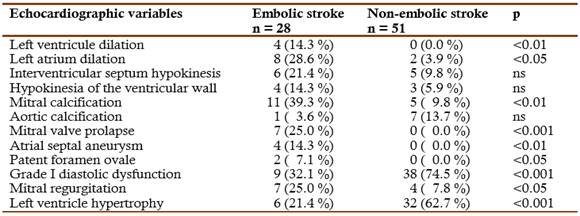
Fisher's Exact Probability Test
An analysis of the quantitative results obtained from studies of glomerular filtration, body mass index, uric acid, cholesterol, and echocardiographic data involving left ventricular ejection fraction in % by Teich, thickness of the interventricular septum and left ventricular wall, as well as % of carotid stenosis in cases with carotid atheromatosis detected by Doppler of supra-aortic trunks (Table 5).
Table 5 Metabolic, echocardiographic, and neurosonological variables according to type of stroke
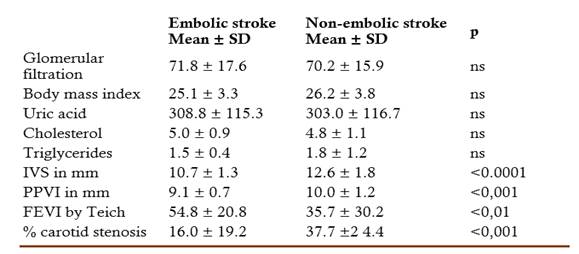
SD standard deviation, IVS interventricular septum, PPVI posterior wall of the left ventricle, FEVI left ventricular ejection fraction. Student's t Test
The mean glomerular filtration rate in embolic strokes was 71.8 and in non-embolic cases it was 70.2 ml/1.7 m2/min. Another parameter we calculated was the body mass index (BMI in kg/m2), which in embolic with a mean of 25.1 and in non-embolic with a mean of 26.1, standard deviations of 3.3 and 3.8 respectively.
The uric acid levels in the blood of the series indicate that the mean in the embolic was 308.3 mml/l and in the non-embolic it was 302 mml/l. Cholesterol levels are maintained with a mean of 5.0 and 4.8 respectively. In the same way, triglyceride levels with a mean of 1,5 for embolic and a mean of 1,8 for non-embolic.
The echocardiographic data analyzed by mean and standard deviation: diameter in mm of the interventricular septum, we found that in embolic patients the mean was 10.7 mm with a standard deviation of 1.3 and the mean of non-embolic ones was 12.5 mm with a standard deviation of 1.8 (p<0.001).
The posterior wall of the left ventricle in embolic patients with a mean of 9.1 mm and in non-embolic patients with a mean of 10 mm (p<0.001).
The left ventricular ejection fraction by Teich, in the case of embolic patients, has of 54.8% and in non-embolic patients of 35.7% (p<0.01). In the neurosonological study of the carotid arteries in which atheromatous plaques were detected, the mean percent of stenosis in embolic was 16% and in non-embolic it rose to 37.7% (p<0.001).
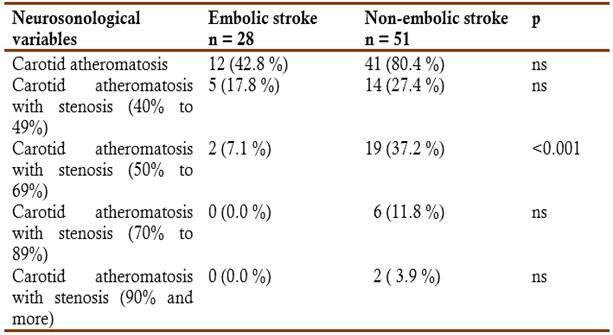
The results of the neurosonological studies (Table 6) of the supra-aortic trunks detect that 41 (80.4%) of the patients with non-embolic stroke had carotid atheromatosis, against 12 (42.8%) of the embolic (p<0.01), it was determined that 5 (17.8%) ) of the embolic strokes had a stenosis of 40 to 49% of the vessel lumen and in the non-embolic in this range 14 (27.4%), in the range of atheromatosis with stenosis of 50 to 69%, 2 (7.1%) were embolic and 19 (37.2%) were non-embolic (p<0.001), with stenosis of the lumen of the vessel greater than 70%, no embolic strokes were reported, 6 (11.8%) were non-embolic and 2 (3.9%) with stenosis of more than 90%, non-embolic.
Discussion
In our series, embolic strokes constitute 32.4%, which is in the range of other multicenter studies and analyzes (Ferrera et al, 2014; Tummala et al, 2016; Ntaios et al, 2017; Froio et al, 2017).
It is more frequent in the elderly (due to the increased prevalence of atrial fibrillation in this population), and in patients under 45 years of age (Tummala et al, 2016; Ntaios et al, 2017).
The predominance of males in this study is a result similar to that obtained in an investigation carried out by Ferreras et al. (2014), where in the analysis of 164 patients, 51.4% were males, however, their results stood out that most of them were of cardio-embolic etiology (58.5%) unlike ours, where it is predominant in the female sex. Some risk factors such as age and history of arterial hypertension, heart failure and previous cerebrovascular disease were relevant in terms of their relationship with the stroke profile in the research we carried out, while other findings reported by Ferreras et al. (2014), they did not find a significant relationship between any of these factors such as hypertension.
These authors did find a higher proportion of smokers, alcoholics and of patients with a history of peripheral vascular disease (p<0.05). As in our group, there was no significant relationship in diabetics, nor in the evaluation of renal function.
These differences could be related to the casuistry, taking into account that these are patients who are sent of other centers in order to determine the etiology of the events, and in others the presence of peripheral arterial disease and the real level of toxic habits was not studied in depth, in the case of arterial hypertension , with non-embolic strokes it is due to its direct relationship with the atherogenesis process, while the mechanisms of cardio-embolic stroke involve other factors that are predominant.
The diagnosis of atrial fibrillation in 46.6% of the patients with embolic stroke in our series is significant (p<0.0001). Atrial fibrillation is independently associated with a 2-fold increased risk of all-cause mortality in women and a 1.5-fold increase in men. Approximately five times the risk of cerebrovascular accident is increased by atrial fibrillation and the risk of all-cause mortality is double (Morady & Zipes, 2016).
Atrial fibrillation is also associated with heart failure (Llisterri et al, 2011; Morady & Zipes, 2016). Cerebrovascular accidents ischemic disorders associated with atrial fibrillation are often fatal, and patients who survive are more disabled by their ischemic episode and are more prone to recurrence than patients with other causes of stroke (Llisterri et al, 2011).
Death from stroke can be greatly reduced by anticoagulation, while other cardiovascular deaths, for example those caused by heart failure or sudden death, remain common even in patients with atrial fibrillation receiving evidence-based treatment (Pepi et al, 2010; Arias et al, 2013).
The risk of stroke in patients with paroxysmal atrial fibrillation it should be considered similar to that of patients with persistent or permanent atrial fibrillation in the presence of risk factors (Morady & Zipes, 2016; Froio et al, 2017).
Some parameters appear significantly in embolic strokes such as: mitral calcification (p<005), mitral valve prolapse (p<001), atrial septum aneurysm (p<0.01) and dilation of the left atrium (p<0.01).
Left ventricular hypertrophy (p<0.001) and grade I diastolic dysfunction (p<0.001) appears to be significantly related to non-embolic infarction. In the study by Secades et al. (2013) on the role of the echocardiogram, mitral calcification and left atrial enlargement coincide as a finding of significant relationship in embolic strokes.
A multivariate analysis to identify the transthoracic echocardiogram markers of potential embolic risk showed that the indexed atrial volume was the only independent risk marker for the development of cardio-embolic stroke [OR 1.10, 95% IC (1.03-1.17), (p<0.01)], and the presence of peripheral occlusive factors showed a strong non-significant trend of higher risk [OR 2.51, 95% IC (0.88-7.18), p=0.085] (Ferrera et al, 2014).
The indication for an echocardiographic study in stroke patients is also controversial. It is known that less than 25% of subjects older than 45 years who consult for a stroke will present alterations in the echocardiography (Weir, 2016; Secades et al, 2013).
In cardio-embolic stroke, in general, echocardiography would be indicated in all patients under 45 years of age and in those over 45 years without significant atheromatosis.
Transthoracic echocardiography can be used as a screening test, although in the absence of clinical or para clinical evidence of heart disease, the possibility of discovering a clear source of cardio-embolism is low.
In the results of a group of quantitative parameters, which include the mean values of glomerular filtration, body mass index, uric acid, cholesterol and triglyceride values according to the clinical subtypes, no significant variation is found. However, data obtained by the transthoracic echocardiogram, such as the diameter of the interventricular septum, have a higher and significant (p<0.0001) mean in patients with non-embolic stroke.
The left ventricle hypertrophy obtained by echocardiography is more specific than when we do the evaluation only by electrocardiogram, it turns out that in the group of non-embolic patients where hypertension is significantly related, and its consequences also appear in a higher percentage than in embolic patients.
Actually the studies that are carried out look for embolic sources and markers for embolic strokes, but we found that there is evidence of hypertensive heart disease that appears in non-embolic patients in a significant way, in relation to embolic strokes (Alvarez et al, 2006).
When we analyze the results of carotid Doppler in patients diagnosed with carotid atheromatosis, the mean stenosis that appears in embolic strokes is lower than in non-embolic strokes where the mean degree of stenosis is high and significant (p<0.0001) compared to the other subtype.
It is significant that 80.4% of the patients in our series with non-embolic stroke had carotid atheromatosis detected and none of the cases with stenosis greater than 70% was embolic. In this study, the characteristics of the atheroma plaques found that are an emboli source.
Doppler echo at the carotid level has a 70% concordance with angiography, which increases to 96% in severe stenosis and occlusions (Pigrettil et al, 2019).
Atherosclerotic carotid stenosis or occlusion causes about 30% of cerebrovascular ischemias. It can also evolve asymptomatically.
The annual risk of stroke in symptomatic carotid stenosis preceded by transient ischemic attack is 12-13%. It is higher if the transient ischemic attack is hemispherical, recent, in crescendo or with severe stenosis. Preceded by stroke, the annual risk again stroke is 5-9%.
The risk increases related to existence of a plaque that is echo lucent, ulcerated, or accompanied by a thrombus. If symptomatic stenosis undergoes endarterectomy, the post-endarterectomy risk is 1-3%, similar to the natural risk for asymptomatic carotid stenosis.
The annual risk of stroke in asymptomatic carotid stenosis > 75% is 2-3%, similar to the post-endarterectomy risk. However, 83% of strokes do not have warning symptoms, which makes treatment decision difficult for asymptomatic stenosis (Buskens et al, 2004, Norris & Halliday, 2004; Pigrettil et al, 2019.
Although so far, in our country, previous studies have been conducted including separately some of variables analyzed here, the present study is the first one including a complete set of variables as considered here in our case.