Introduction
Peptic ulcer is a defect of the gastrointestinal mucosa that can reach the muscularis mucosae and is primarily the result of the activity of hydrochloric acid and pepsin in the digestive tract from the distal portion of the esophagus to the duodenum.1)
The prevalence of peptic ulcer is estimated between 5% and 10% of the general population (this figure raises to 10% -20% if individuals infected by Helicobacter pylori are considered). The incidence ranges between 0.1% and 0.3%, but it reaches up to 1% among H. pylori positive persons, which represents a rate of 6 to 10 times higher than that described in non-infected individuals. Gastric ulcer was the most common form of peptic ulcer in the last century. However, at present, its annual incidence is much lower than that of duodenal ulcer. (2
The most accepted concept to explain the pathophysiology of peptic ulcer is that it is a consequence of an imbalance between the aggressive and defensive factors that regulate the function of the gastrointestinal tract. Among the former, the hypersecretion of acid, gastrin and pepsinogen has been classically considered as the fundamental pathophysiological disorder in patients with duodenal ulcer. (1,2,3
The objective of the treatment of peptic ulcer is the relief of symptoms, the healing of the ulcer and the prevention of symptomatic recurrence and complications. 3
Non-adherence to properly prescribed medications compromises the effectiveness of available treatments, interferes with patient recovery and represents a considerable expense for national health systems. (4)
The World Health Organization considers adherence as “the degree to which a person's behavior - when taking the medication, following a diet and carrying out lifestyle changes - corresponds to the agreed recommendations of an assistance sanitary provider.“ As can be seen, the concept of adherence goes beyond the classical term of compliance which suggests that the patient follows the doctor's instructions passively and that the treatment plan is not based on a therapeutic alliance or contract established between the patient and the doctor. The concept of therapeutic adherence therefore refers to a great diversity of behaviors that include taking part of the treatment, not stopping a medication before the course of treatment is completed, not taking more or less medication than prescribed, not taking a dose at wrong time, furthermore developing health behaviors, avoiding risk behaviors and attending appointments arranged by health professionals. (4,5
In addition, the lack of adherence may be unintentional, as a consequence of forgetting or lack of skills to follow the treatment; or intentional, as a consequence of a conscious decision of the patient.
There are several researchs in the world on adherence to the treatment of chronic diseases such as arterial hypertension, diabetes mellitus, tuberculosis, but not pertaining to peptic ulcer. (6,7 Something similar happens in Cuba, 7,8 innumerable figures are presented by studies related to digestive disorders, although epidemiological investigations that include adherence to the treatment of peptic ulcer disease are insufficient. It is necessary to deepen on this topic; since the leaving of the treatment is frequent in patients when feeling improvement, and that is when the relapses appear. Good adherence is translated into a higher cure rate and less expenses for the patient and for the health system. It is necessary to emphasize that the medications used in this condition are expensive and used in other medical indications as well. All this motivated to investigate on the subject, to achieve increase the adherence to the treatment on these patients, which results in satisfactory results in health. The objective of the present investigation is: To determine the factors that influence adherence to treatment on patients diagnosed with peptic ulcer in health areas of the Bayamo municipality, in the period from July 2018 to April 2019.
Methods
A prospective observational analytical study was carried out that corresponds to a study of drug use in patients with endoscopic diagnosis of peptic ulcer, in health areas of the Bayamo municipality, in the period from July 2018 to April 2019.
The population of the studyconsisted of 330 patients with an endoscopic diagnosis of peptic ulcer in the Bayamo municipality, during the studied period. To measure the sample size, the sample sizes module was used to compare survival curves and the procedure was as follows: it is known from clinical practice that the rate of adherence to peptic ulcer treatment is 20% adherents (group 1) and 38% non-adherents (group 2) so the following parameters were prearranged: a confidence level of 95%, an error α ═ 0.05, a power of 80% and a ratio between samples (group 2 / group 1) of 1.3 and it was expected to lose 0.1% of the patients during the follow-up, resulting a sample size of 177 patients; 77 from group 1 and 100 from group 2, it was calculated by using EPIDAT version 3 statistical package.
The following aspects were taken into account:
Inclusion criteria:
Patients´will to participate in the study, with the filling of informed consent form. Patients´ aged from 18 years and over who were diagnosed by endoscopic study of peptic ulcer.
Exclusion criteria:
Patients who, in addition to peptic ulcer disease, suffered from other digestive diseases.
Patients with psychiatric illnesses.
The data of the investigation were obtained in a collection form of the primary data (Annex I), which was completed by individual medical interview with each patient that participated in the study.
It was defined as a dependent variable: Adherence to treatment, defined as compliance by itself; (take the medication according to the dosage of the prescribed program) in addition to the persistence (taking the medication throughout the established time) that is the degree to which the patient's behavior coincides with all the recommendations made by the doctor about pharmacological and non-pharmacological measures.
It was operating as adherence, if the patient answered "always" in items c, d, e, g and h, and the rest items from question 16 (compliance with non-pharmacological measures is measured) and Morisky - Green´s test correctly (Question 17) Annex II. It was considered as non-adherence, when patients´answers did not meet these requirements. This variable was classified as nominal qualitative dichotomous.
To determine the relationship between adherence to treatment as a dependent variable and the independent ones (age, sex, living area, school level, occupation, patient´s economic resources, knowledge about his disease, compliance with the non-pharmacological and pharmacological treatment, complexity of the treatment , adverse reactions, availability and cost of the medications, medical guidelines prescribed to the patient, the follow-up and doctor-patient relationship) the Chi-square test was used and a significance level of 0.05% was established.
The results obtained in the study were compared with current national and international literature and other published articles and were processed by the statistical package EPIDAT VERSION 3.0 for Window.
This research was carried out under conditions of respect from fundamental people rights and ethical regulations that affect biomedical research with human beings, following the contents of the Declaration of Helsinki and its subsequent updates.
Results
There was therapeutic adherence in 51 (28.8%) patients, while 126 patients did not have adherence, which represented 71.2% of the total. Statistical calculation showed that there was no relationship between age and adherence to treatment. The lack of adherence was found to be greater in men, which represented 50.3% of the studied population. Patients who lived in urban areas (58.2%) showed lack of adherence whicrepresented 34.5% of the sample. It was greater in patients that lived in rural area 36.7% of the total. There was a significant association (x2 = 16.8112, p = 0.0000).
Talking about educational levels, the largest numbers of patients (35%) were pre-university students, in which the lack of adherence predominated, constituting 25.4% of the non-adherents. The greatest differences between adherents and non-adherents were in the primary, secondary and technical schools students. The statistical analysis using the Chi-square method demonstrated a great influence between school level and adherence. (x2 = 10.6797, p = 0.0304).
There was a predominance in 71 (40.1%) workers in which the non-adherence was alarming; 33.9% of the study population. There was an important association between occupation and adherence, since the independent variable (occupation) negatively influenced adherence to treatment, this was reaffirmed by the statistical calculation of the square Chi (x2 = 15.7445, p = 0.0004)
Although the economic resources of the participants were not high in general, it was impossible to statistically show that there was an association between the variable (economic resources) and the adherence to treatment.
Table 1 shows patients´adherence according to their knowledge about the disease. 71 patients (40.1%) who had a moderate level of knowledge about the disease predominated, in which the lack of adherence was greater (33.3% of the total). However, the therapeutic adherence was higher in those who showed high knowledge; 26 (14.7%) out of 49 patients adhered to treatment. When statistically analyzing the influence of knowledge on the dependent variable adherence, the association between the two was found to be relevant. (x2 = 12.8073, p = 0.0017).
Table 1 Patients adherence according to their level of knowledge about disease.
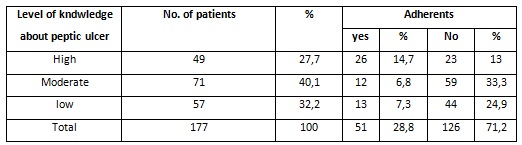
Chi-square = 12,8073; p= 0,0017.
Source: Survey.
Table 2, reveals the distribution of patients with peptic ulcer according to non-pharmacological treatment compliance. In 110 patients treatment was performed inadequately, this represented 62.1% of the sample; in them the absence of adherence to non-pharmacological treatment predominated, which accounted for 59.3% of the total. In addition, as a result of the application of the Chi-square test, the existence of a statistically significant relationship between compliance with non-pharmacological treatment and lack of adherence was verified. (x2 = 82.3060, p = 0.0000).
Table 2 Patients distribution according to the compliance of non-pharmacological treatment.
| Compliance | No. of patients | % | Adherence | |||
|---|---|---|---|---|---|---|
| Yes | % | No | % | |||
| Adequate | 67 | 37,9 | 46 | 26 | 21 | 11,9 |
| Inadequate | 110 | 62,1 | 5 | 2,8 | 105 | 59,3 |
| Total | 177 | 100 | 51 | 28,8 | 126 | 71,2 |
Chi-square =82,3060; p=0,0000.
Source: Survey.
When studying the results of Table 3, it is found that 129 patients performed the pharmacological treatment inadequately, constituting 72.9% of the sample, in this group the non-adherence prevailed, reflecting 70.1% of the total. The main difficulties with respect to compliance were caused by forgetting and not taking the medicines at the prescribed time. There was also a statistically significant influence between this variable and adherence to treatment, which was verified by determining the Chi-square. (x2 = 144.2237, p = 0.0000).
The treatment was complex in 125 patients, which represented 70.6%, in which the lack of adherence was significant, which constituted 67.2% of the people included in the study.
Table 3 Patients distribution according to with pharmacological treatment compliance.
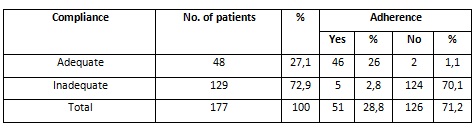
Chi-square=144,2237; p=0,0000.
Source: Survey.
Table 4 illustrates the distribution of patients with peptic ulcer according to adverse reactions to treatment. 98 (55.4%) patients experienced frequent adverse reactions. The gastrointestinal disorders were the most commun illness that affected the patients that suffer from pectic ulcer and metronidazole was the drug that caused the greatest adverse reactions. When performing the statistical calculation using the Chi-square test, the existence of influence of the undesirable responses on the therapeutic adherence was demonstrated. (x2 = 9.4465, p = 0.0239).
Table 4 Patients distribution according to adverse reactions experimentation
| adverse reactions | No. of patients | % | Adherence | |||
|---|---|---|---|---|---|---|
| Yes | % | No | % | |||
| Frequent | 98 | 55,4 | 22 | 12,4 | 76 | 42,9 |
| Occasional | 45 | 25,4 | 21 | 11,9 | 24 | 13,6 |
| Rare | 7 | 4 | 2 | 1,1 | 5 | 2,8 |
| None | 27 | 15,3 | 6 | 3,4 | 21 | 11,9 |
| Total | 177 | 100 | 51 | 28,8 | 126 | 71,2 |
Chi-square =9,4465; p=0,0239.
Source: Survey.
Although the drugs were available in 82 patients, non-adherence prevailed in 24.3% of the sample, the statistically significant influence between the availability of the drugs and the lack of adherence was verified by the Chi-square test. (x2 = 26.6746, p = 0.0000)
There was an important association between price of medicines and adherence, since the price of the drugs had a negative effect on adherence to treatment, this was confirmed by the statistical calculation of the square Chi. (x2 = 43.0404, p = 0.0000)
Although table 5 showes the influence of doctor-patient relationship over the dependent variable (adherence). No statistical association was found between both, calculated by Chi-square. (x2 = 0.1938, p = 0.1228).
Discussion
Studies of therapeutic adherence present a very relevant evaluation problem. None measurement strategies have been considered optimal, so the combination of methods have been stimated as the best approximation to the measurement of adherence behavior. Some jobs use clinical criteria. Others are based only on direct questions to patient. The questionnaires are one of the most used procedures due to the simplicity as they reflect patients´ behavior and are based on direct questions of easy application. The main disadvantage is that they tend to overestimate compliance. (9
Observation of taking the medication by trained personnel is probably one of the most reliable methods in hospital settings. The presence of the drug in the blood or urine is an expensive and complex method since it requires laboratory analysis. Electronic devices for measuring compliance or use control, such as the Medication Event Monitoring System (MEMS), are considered less intrusive and more feasible than direct observation, but their high cost precludes their widespread use in daily consultation. On the other hand, the opening of the bottle at certain hours by the patient does not absolutely guarantee the taking of the drug. 9,10
It has been suggested that the lack of adherence could be, fundamentally, the result of adverse events or the absence of a therapeutic response. However, there are other factors that intervene in therapeutic compliance, such as those related to the patient, the disease, medication and the doctor. (5,7,9
Despite the limited available evidence, modifying certain unhealthy lifestyle habits can be beneficial: stop smoking, avoid foods that cause discomfort and worsen symptoms, and avoid coffee, alcohol, among others. The patient should be helped to identify and modify the possible triggers, as well as promote healthy lifestyle habits. 6,7,10
In a study conducted in Mexico, 11 to evaluate the effect of a cognitive-behavioral intervention on adherence to treatment and the emotional regulation of patients with digestive disorders favorable changes were observed in adherence behaviors and emotional regulation at the end of the investigation. It is indisputable that the knowledge and characteristics of the individual influence adherence. Several authors describe that the cognitive-behavioral variable exercises a direct control over aspects of healthy modifying behavior and it is evident that the person who knows the causes, consequences and reasons of treatment has greater motivation to comply and perception of what really happens and know that with better behavior can become a healthy person without the need of other treatments.
Apart from beliefs about the disease, beliefs regarding treatment are a major factor influencing non-adherence to treatment. Thus, a large number of studies, 4,9,12,13 have shown that positive attitudes of patients with regard to medication are associated with an increase in adherence, both directly and indirectly (for example through the impact of doctor-patient communication).
From the review conducted it has been found that patients who have a good doctor relationship receive more information and are allowed to choose between different therapies adhere bettee to the prescribed treatment. Regarding this point, it is also helpful for the doctor to attend patient´s beliefs and take them into account when prescribing treatment decisions. (14,15
An incorrect compliance of the treatment by the patient, can lead the doctor to the conclusion that the management is not effective, so the doctor would increase the dose or make unnecessary changes or combinations of drugs, which increase the risk of side effects and the reasons for non-compliance. 11,12,15
Similar results were obtained in a study done in "José Martí" Health Area, from Santiago de Cuba, in which a good level of therapeutic adherence were obtained and only 5% of patients showed poor adherence. Health education activities were implemented which allowed patients to adopt positive behaviors and improve their lifestyle.
Finally, it should be noted that the results obtained pointed out that the patients with greater therapeutic adherence are those who have a better perception of the effect of medication with an earlier recovery than those patients who do not comply with the prescribed treatment.
Conclusions
There was a lacking of adherence to treatment to heal the pecptic ulcer in patients studied in this research. Male sex, living in rural geographic area, educational level and occupation were the main socio-demographic variables that influenced low adherence while age was no significant. Complexity of the management plan prescribed by the doctor, frequent adverse reaction, availability and cost of drugs were factors that triggered low therapeutic adherence. Moderate knowledge about the disease, inadequate performance of non-pharmacological and pharmacological measures affected non-adherence. Variebles related to the doctor´s role such as; doctor´s orientation, follow up and doctor - patient realationship, were not decisive factors in deprived adherence to treatment.
The study of adherence and the factors that impact it are imperative and should be a part of the habitual clinical care of chronic diseases in order to improve health.














