Meu SciELO
Serviços Personalizados
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de Ciencias Médicas de Pinar del Río
versão On-line ISSN 1561-3194
Rev Ciencias Médicas vol.27 no.2 Pinar del Río mar.-abr. 2023 Epub 01-Mar-2023
Articles
Results of postoperative analgesia with continous paravertebral block in patients undergoing elective thoracic surgery
1University of Medical Sciences of Camagüey. Martín Chang Puga General Teaching Hospital. Camagüey. Cuba.
2University of Medical Sciences of Camagüey. Manuel Ascunce Domenech Surgical Clinical Teaching Provincial Hospital. Camagüey. Cuba.
Introduction:
postoperative pain associated with thoracic surgery is generally severe both in intensity and duration. Its inadequate management conditions the appearance of physical and psychological complications such as chronic post-thoracotomy pain syndrome.
Objective:
to evaluate the results of postoperative analgesia with continuous paravertebral block in patients undergoing elective thoracic surgery.
Methods:
A quasi-experimental non-observational study was conducted at the Manuel Ascunce Domenech Surgical Clinical Teaching Provincial Hospital of Camagüey, between June 2016 and June 2019. The universe was constituted by 40 patients submitted to elective thoracic surgery for intrathoracic tumors and to whom postoperative analgesia was applied. Analgesia techniques were compared by dividing the sample into 2 groups.
Results:
There were no differences between groups in terms of pain intensity perception (p<0,05), but most patients (75,0 %) required rescue analgesia, with no differences between groups in this aspect (p=0,144). Most patients reported being satisfied with the treatment. The most frequent complication was pruritus, being present in 37,5 % of patients.
Conclusions:
It is concluded in this work that the application of continuous thoracic paravertebral block is as effective as epidural block in the postoperative analgesic treatment of patients undergoing elective thoracic surgery.
Key words: THORACIC PARAVERTEBRAL BLOCK; PAIN MANAGEMENT; EPIDURAL ANESTHESIA; ANESTHETIC COMPLICATIONS
INTRODUCTION
Most patients undergoing elective surgery experience postoperative pain to a variable degree. The satisfactory control of this type of pain is one of the most important challenges that remain unresolved in the surgical setting, which has a strong impact on patients and on the healthcare system as a whole.1
Postoperative analgesia is one of the basic components in functional recovery after surgery. The blockade of nociceptive stimuli contributes to decrease the response to surgical stress, accelerating rehabilitation and decreasing the incidence of postoperative chronic pain. However, it is difficult to isolate the effects of postoperative analgesia from other aspects related to surgical technique, clinical practice, type of analgesic monitoring or organizational factors of the surgical team.2
Nociceptive impulses, upon reaching the nerve centers, will give rise to segmental, supra-segmental and cortical responses. These responses define the body's reaction to the aggression and constitute the basis that explains the post-surgical problems linked to the presence of pain.3
Many methods for the treatment of post-thoracotomy pain have been proposed with variable success: intercostal block, interpleural analgesia, cryoanalgesia, lumbar epidural and thoracic epidural analgesia, paravertebral block, intravenous opioids and transcutaneous nerve stimulation. Epidural analgesia has long been considered the standard reference for the treatment of acute post-thoracotomy pain.4
The treatment of pain after thoracic surgery by epidural administration of opioids has several important advantages. Firstly, there is no sympathetic blockade or motor loss; secondly, it is usually possible to predict the efficacy of analgesia; and finally, the duration of analgesia achieved is usually much longer, and its quality much better, than that obtained by parenteral administration of opioids.5
Thoracic paravertebral blockade has been described in the sitting or decubitus position (lateral or prone). The advantage of the former is the better identification of the repair points; the advantages of the latter are: patient comfort, better hemodynamic stability or precaution against vagal responses and the possibility of performing the procedure with the patient under various levels of sedation, and even, as has been reported, with the patient already under general endotracheal anesthesia. Whatever the position, we proceed to identify the anatomical landmarks, which for this block are the spinous processes, which allow us to identify the midline.6
The thoracic paravertebral space contains: fat, intercostal (spinal) nerves, communicating branches and in its anterior portion the sympathetic chain. The spinal nerves at this level are very susceptible to local anesthetics because they are subsegmented into small branches that lie freely between the fat and are devoid of a fascial sheath, with no epineurium or perineurium.7 The intercostal nerves emerge from the intervertebral foramen and traverse the space from side to side, with communicating branches to the sympathetic chain. The posterior branch of the spinal nerve lies in the space and only leaves it past the medial border of the superior costotransverse ligament. These anatomical considerations allow the thoracic paravertebral block to be an option to achieve postoperative analgesia in patients treated with thoracotomies.1
There are few studies in Cuba that evaluate the effectiveness of thoracic paravertebral block in major surgery. The most commonly used technique to provide postoperative analgesia consists of the administration of local anesthetics and opiate derivatives through an epidural catheter, which, despite its safety profile and efficacy in pain relief, is not free of complications. Determining the efficacy of postoperative analgesia with continuous paravertebral block in patients undergoing elective thoracic surgery would be another option to be taken into account in the anesthetic-surgical management of this type of patient.
Taking into account that postoperative pain associated with thoracic surgery is generally severe both in intensity and duration, and its inadequate management conditions the appearance of physical and psychological complications such as chronic post-thoracotomy pain syndrome, this research was carried out with the aim of evaluating the results of postoperative analgesia with continuous paravertebral blockade in patients undergoing elective thoracic surgery.
METHODS
A quasi-experimental non-observational study was carried out at the Surgical Clinical Teaching Provincial Hospital Manuel Ascunce Domenech of Camagüey, between June 2016 and June 2019.
The universe was constituted by 40 patients submitted to elective thoracic surgery for intrathoracic tumors and to whom postoperative analgesia was applied, attended by the service of Anesthesiology and Resuscitation of the mentioned institution. A non-probabilistic purposive sampling was applied according to the investigator's criteria, in which all patients fulfilled the criteria.
Patients over 20 years of age, with physical status II and III according to the American Society of Anesthesiology (ASA) classification, and who agreed to participate in the study by signing the informed consent form, were included in the study. Exclusion criteria were established as those patients with a history of allergy to the drugs used, and as exit criteria those who presented any perioperative anesthetic-surgical complication that made the initial anesthetic method to be modified, making the evaluation and follow-up of postoperative analgesia difficult.
To carry out the quasi-experiment, the sample was divided into two treatment groups, Group I (control group), in which the conventional anesthetic method was applied (bupivacaine 0,125 % with doses of 7 ml/h to 14 ml/h associated with fentanyl 3 mcg/ml by epidural catheter in continuous perfusion) and Group II (study group), in which fentanyl 3 mcg/ml by epidural catheter in continuous perfusion was used, in which continuous paravertebral block (bupivacaine 0,25 % with 7ml/h dose associated with fentanyl 3mcg/ml by paravertebral catheter in continuous perfusion) was used for postoperative analgesia. The distribution of patients in groups was simple randomized. In both groups and in the absence of complications, the loading dose (bupivacaine 0,25 % condosis of 10ml plus fentanyl 5mcg/ml by epidural or paravertebral catheter) was administered just before the end of surgery, followed by continuous perfusion of the drugs used according to the study groups, with the aim of achieving postoperative analgesia. All patients underwent endotracheal general anesthesia using the Fabius GS anesthesia machine.
For the collection of the primary data, the medical records of the patients were reviewed prospectively, which included the anesthesia sheet, as well as the interview with the patients and the anesthetic evaluation the day before surgery, and were collected in a form designed by the authors; these data included the following variables: age, sex, risk factors, physical status according to ASA classification, operative diagnosis, postsurgical evaluation, heart rate, respiratory rate, oxygen saturation, mean arterial blood pressure, postoperative pain intensity according to the visual analog scale, use of rescue analgesia, satisfaction with analgesia, and postoperative complications.
The postoperative evaluation was performed at three time points (M): M1: 2 hours after the end of surgery, M2: 12 hours after the end of surgery and M3: 24 hours after the end of surgery. Rescue analgesia was provided on demand, by administration of bupivacaine 0,25 % (10ml) plus fentanyl (5mcg/ml) by epidural or paravertebral catheter.
For the processing and analysis of the information, a database was created in the SPSS version 25,0 statistical package; descriptive indicators such as absolute and relative frequencies and percentages were obtained, as well as those related to the association between variables, and from these the tables were filled in.
The approval of the Medical and Research Ethics Committee of the Surgical Clinical Teaching Provincial Hospital Manuel Ascunce Domenech was requested for this research. All the information obtained was used only for scientific purposes and the ethical principles dictated in the II Declaration of Helsinki were taken into account.
RESULTS
The mean age of the sample was 58,5±9,2 years, with no statistically significant differences between the control group and the study group (p=541). There was a slight predominance of male sex (57,5 %) and the most frequent personal pathological antecedents were smoking (65,0 %), arterial hypertension (40,0 %) and COPD (30,0 %), with no statistically significant differences between the groups in any of the cases (p>0,05). (Table 1)
Table 1 Distribution of patients according to group, epidemiological characteristics and personal pathological history. Manuel Ascunce Domenech Surgical Clinical Teaching Provincial Hospital. Camagüey. June 2016 - June 2019.

Source: Medical records
Regarding physical status according to ASA, all patients were evaluated as ASA-II and ASA-III, with a predominance of those evaluated as ASA-III (77,5 %), and there were no statistically significant differences between the two groups (p=0,705). The most frequent operative diagnosis was lobectomy (55,0 %), and there were no statistically significant differences between groups and operative diagnosis (p=0,232). (Table 2)
Table 2 Distribution of patients according to group, physical status and operative diagnosis.
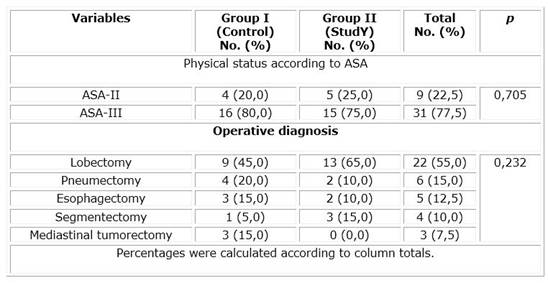
Source: Medical records
In the analysis of the vital signs compared at the three moments evaluated, it was observed by means of the ANOVA technique that there were no statistically significant differences between the quadratic means of heart rate, respiratory rate, partial oxygen saturation and blood pressure (p>0,05). (Table 3)
Table 3 Distribution of patients according to group and vital parameters evaluated at the three postoperative moments.
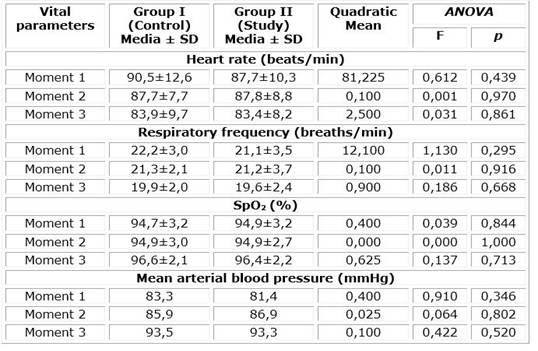
Source: Medical records
Regarding the distribution of patients according to group and pain intensity by means of the visual analog scale (VAS) evaluated at the three postoperative moments, it was observed that no patient referred pain as severe at any moment in any of the two groups studied. It was also observed by means of Pearson's X2 analysis, based on its homogeneity hypothesis, and the Monte Carlo significance (in the cases where it was applied), that there were no differences between the groups regarding the perception of pain intensity (p<0,05) in any of the moments in which the patients were evaluated (Table 4)
Table 4 Distribution of patients according to group and pain intensity evaluated in the three postoperative moments.
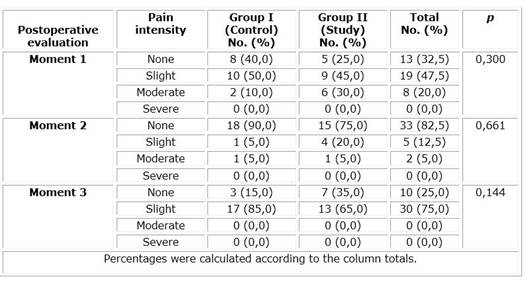
Source: Medical records
It could be seen that most of the patients (75,0 %) required rescue analgesia according to the programmed protocol, with no differences between groups in this aspect (p=0,144). Regarding satisfaction with analgesia, most patients reported being satisfied, both in the control group (85,0 %) and in the study group (65,0 %). There were no statistically significant differences between the two groups in terms of satisfaction with analgesia (p=0,144).
Table 5 Distribution of patients according to group, need for rescue analgesia and satisfaction with analgesia during the surgical procedure.
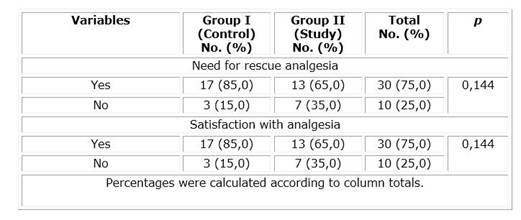
Source: Medical records
Regarding complications, pruritus was the most frequent, being present in 37,5 % of the patients, followed by nausea and vomiting (35,0 %), cardiac arrhythmias (15,0 %) and hypotension, which only occurred in 1 patient (2,5 %). There were no statistically significant differences between the groups in terms of complications (p>0,05).
Table 6 Distribution of patients according to group and postoperative complications.
| Complicacions | Group I (Control) No. (%) | Group II (Study) No. (%) | Total No. (%) | |
|---|---|---|---|---|
| Pruritus | 6 (30,0) | 9 (45,0) | 15 (37,5) | 0,327 |
| Nausea and vomiting | 7 (35,0) | 7 (35,0) | 14 (35,0) | 1,000 |
| Cardiac arrhythmias | 2 (10,0) | 4 (20,0) | 6 (15,0) | 0,376 |
| Hypotension | 1 (5,0) | 0 (0,0) | 1 (2,5) | 0,311 |
Percentages were calculated according to column totals.
Source: Medical records
DISCUSSION
The present work evaluated the results of postoperative analgesia with continuous paravertebral block in patients undergoing elective thoracic surgery, comparing this technique with the conventionally used epidural block. At the international level, a Cochrane review was recently published by Yeung et al.8 comparing the effectiveness of thoracic paravertebral block in patients undergoing thoracotomy with epidural anesthesia, in terms of important variables such as mortality, major complications, minor complications, pain relief and hospital stage, which yielded quite conclusive results.
In the present work the patients had a mean age of 58,5±9,2 years; in a recently published study by Zengin et al.9 the mean age of patients undergoing video-assisted thoracic surgery was 44,3 years. This study demonstrated the efficacy and safety of the use of paravertebral thoracic block in the management of pain in this type of patient, although it should be noted that this was a pilot study carried out in only 13 patients. Older ages are associated with a higher anesthetic risk, due to a greater presence of comorbidities and a higher incidence of complications during surgery; however, these are not significant when patients enter the geriatric age, since below 65 years of age there are no differences in prognosis in the different age groups in adult patients.10
In this study there were no statistical differences in terms of sex, and the most frequent personal pathological antecedents were smoking, arterial hypertension and COPD. Wang et al.11 on comorbidities in the use of thoracic paravertebral block with opioids in internal rib fixation mentioned that comorbidities did not influence the presence of complications related to anesthesia.
The patients who integrated the sample in this investigation were functionally classified in their entirety as ASA-II and ASA-III. Patients undergoing elective thoracic surgery for intrathoracic tumors were included, in which the operative diagnoses were lobectomy, pneumectomy, esophagectomy, segmentectomy and mediastinal lumpectomy, all these surgical procedures were performed by open thoracotomy. Many other studies evaluate the thoracic paravertebral block in other types of interventions, for example: Wang and Peng et al.11 evaluate it in internal rib fixation, while Wang and Zhang et al.12) evaluated it in proximal humerus fracture surgery. Schreiber et al.,13 evaluated the effectiveness of paravertebral block in liver resection surgery, while authors such as Teeter and Kumar,14) and Martinisiv et al.,15) like the present study, compared thoracic paravertebral block with thoracic epidural block in patients undergoing thoracotomy.
Most authors agree that the results of analgesia with paravertebral block are comparable to those of epidural block. However, paravertebral block has some advantages over the epidural block technique, such as those derived from the fact that it can be performed unilaterally, thus preserving the respiratory and sympathetic functions of the side contralateral to the anesthetic injection. This may be associated with lower rates of hypotension, fewer pulmonary complications and lower incidence of urinary retention. In addition, failure rates in the adult technique are significantly lower in most published series.11,12-13
Teeter and Kumar,14 report that in patients undergoing thoracotomy, epidural catheter analgesia was associated with lower rates of complications, including vascular puncture, hypotension, hematoma, puncture site pain and pneumothorax These results differ from those of the present study, since there were no statistically significant differences in the incidence of complications, which included only pruritus, nausea and vomiting, cardiac arrhythmias and hypotension.15
Tamayo et al.,16 in their study on thoracic epidural analgesia for postoperative pain relief in thoracotomy described a mean oxygen saturation of 99,5 % and respiratory rate of 16 res/min, while most patients had no postoperative complications secondary to the analgesic technique, and rescue analgesia was not necessary in most of them. In the present study, the partial oxygen saturation figures in both groups were not significantly different, nor were the heart rate, respiratory rate and blood pressure. In this work, 75,0 % of the patients required rescue analgesia, with no significant differences in terms of the anesthetic treatments compared, although it should be noted that patients treated with continuous paravertebral block required rescue analgesia less frequently.
In this study, satisfaction with postoperative analgesia was quite high, both in patients treated with epidural block and in those in whom continuous paravertebral block was used. Rabanal Llevot et al.,17 agree with the results of this work, since they report a level of satisfaction of 80,0 %, close to the 75,0 % described in this work.
Regarding pain intensity evaluated by means of the visual analog scale (VAS), the patients studied reported pain mostly as light, moderate or absent, without this variable being significantly different in terms of the two treatments used. However, it was observed that in the serial assessment of pain (at 2 hours, 12 hours and 24 hours), pain was absent more frequently at 24 hours in the group in which continuous paravertebral block was used, while at 2 hours and 12 hours, pain was absent more frequently in patients treated with thoracic epidural block. Although there were no significant differences, it can be inferred from the frequency analysis that continuous paravertebral block relieved pain more efficiently in the mid or late postoperative period, while epidural block did so more effectively in the immediate postoperative period.
Marshall and McLaughlin,18 and Ma et al.,19) agree with the results of the present work, since they report that thoracic paravertebral block is as effective in pain relief as epidural block, being even superior in some cases.
It is concluded in this work that the application of continuous thoracic paravertebral block is as effective as epidural block in the postoperative analgesic treatment of patients undergoing elective thoracic surgery, with similar rates of complications, patient satisfaction and need for rescue anlagesia.
BIBLIOGRAPHIC REFERENCE
1. Redondo GZ, Díaz MM, Pascual VH, García DG. Estrategias y problemas asociados a la analgesia postoracotomía. Revista Cubana de Anestesiología y Reanimación [Internet]. 2013 [Citado 01/11/2022]; 12(1): 70-9. Disponible en: Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=43009&id2= 1. [ Links ]
2. Alonso Tuñón O, Balsera Valle M, Acosta Martínez J, García Aparicio P, Vilches Arenas Á. Analgesia perioperatoria mediante bloqueo del plano erector espinal en implante de asistencia ventricular izquierda. Revista Española de Anestesiología y Reanimación [Internet]. abril de 2022 [Citado 01/11/2022]; 69(10): 689-692. Disponible en: Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S003493562100308X 2. [ Links ]
3. Álvarez-Baena L, Hervías M, Ramos S, Cebrián J, Pita A, Hidalgo I. Analgesia paravertebral torácica continua tras cirugía mínimamente invasiva de cierre de comunicación interauricular en población pediátrica: análisis de eficacia y seguridad. Rev Esp Anestesiol Reanim [Internet]. 1 de mayo de 2022 [Citado 01/11/2022]; 69(5): 259-65. Disponible en: Disponible en: https://www.elsevier.es/es-revista-revista-espanola-anestesiologia-reanimacion-344-articulo-analgesia-paravertebral-toracica-continua-tras-S0034935621002152 3. [ Links ]
4. Ardon AE, Lee J, Franco CD, Riutort KT, Greengrass RA. Paravertebral block: anatomy and relevant safety issues. Korean J Anesthesiol [Internet]. octubre de 2020 [Citado 01/11/2022]; 73(5): 394-400. Disponible en: Disponible en: https://doi.org/10.4097/kja.20065 4. [ Links ]
5. Ben Aziz M, Mukhdomi J. Thoracic Paravertebral Block. En: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [Citado 01/11/2022]. Disponible en: Disponible en: http://www.ncbi.nlm.nih.gov/books/NBK570560/ 5. [ Links ]
6. Bigler D, Dirkes W, Hansen R, Rosenberg J, Kehlet H. Effects of thoracic paravertebral block with bupivacaine versus combined thoracic epidural block with bupivacaine and morphine on pain and pulmonary function after cholecystectomy. Acta Anaesthesiol Scand [Internet]. octubre de 1989 [Citado 01/11/2022]; 33(7): 561-4. Disponible en: Disponible en: https://doi.org/10.1111/j.1399-6576.1989.tb02966.x 6. [ Links ]
7. Carballo Fernández J, García Pérez A, Jiménez Calvo AM, Sampayo Rodríguez L. Thoracic paravertebral block with spinal space diffusion. Minerva Anestesiol [Internet]. agosto de 2022 [Citado 01/11/2022]; 88(7-8): 639-40. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/35199978/ 7. [ Links ]
8. Yeung JHY, Gates S, Naidu BV, Wilson MJA, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev [Internet]. 21 de febrero de 2016 [Citado 01/11/2022]; 2(2): CD009121. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/26897642/ 8. [ Links ]
9. Zengin M, Baldemir R, Ulger G, Sazak H, Alagoz A. Postoperative Analgesic Efficacy of Thoracic Paravertebral Block and Erector Spinae Plane Block Combination in Video-Assisted Thoracic Surgery. Cureus [Internet]. junio de 2021 [Citado 01/11/2022]; 13(6): e15614. Disponible en: https://doi.org/10.7759/cureus.15614 [ Links ]
10. Xiong C, Han C, Zhao D, Peng W, Xu D, Lan Z. Postoperative analgesic effects of paravertebral block versus erector spinae plane block for thoracic and breast surgery: A meta-analysis. PLoS One [Internet]. 2021 [Citado 01/11/2022]; 16(8):e0256611. Disponible en: Disponible en: https://doi.org/10.1371/journal.pone.0256611 10. [ Links ]
11. Wang A, Peng T, Zhang P, Fan K. Thoracic Paravertebral Block (TPVB) in non-intubated open reduction and internal rib fixation. Journal of Clinical Anesthesia [Internet]. 1 de octubre de 2020 [Citado 01/11/2022]; 65: 109848. Disponible en: Disponible en: https://www.sciencedirect.com/science/article/pii/S0952818020303287 11. [ Links ]
12. Wang X, Zhang H, Xie Z, Zhang Q, Jiang W, Zhang J. The effectiveness of additional thoracic paravertebral block in improving the anesthetic effects of regional anesthesia for proximal humeral fracture surgery in elderly patients: study protocol for a randomized controlled trial. Trials [Internet]. 19 de febrero de 2020 [Citado 01/11/2022]; 21(1): 204. Disponible en: Disponible en: https://doi.org/10.1186/s13063-020-4078-9 12. [ Links ]
13. Schreiber KL, Chelly JE, Lang RS, Abuelkasem E, Geller DA, Marsh JW, et al. Epidural Versus Paravertebral Nerve Block for Postoperative Analgesia in Patients Undergoing Open Liver Resection: A Randomized Clinical Trial. Reg Anesth Pain Med [Internet]. agosto de 2016 [Citado 01/11/2022]; 41(4): 460-8. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/27281726/ 13. [ Links ]
14. Teeter EG, Kumar PA. Pro: Thoracic Epidural Block Is Superior to Paravertebral Blocks for Open Thoracic Surgery. J Cardiothorac Vasc Anesth [Internet]. diciembre de 2015 [Citado 01/11/2022]; 29(6): 1717-9. Disponible en: Disponible en: https://doi.org/10.1053/j.jvca.2015.06.015 14. [ Links ]
15. Martsiniv VV, Loskutov OA, Strokan AM, Bondar MV. Efficacy of pectoral nerve block type II versus thoracic paravertebral block for analgesia in breast cancer surgery. Wiad Lek [Internet]. 2020 [Citado 01/11/2022]; 73(7): 1470-5. Disponible en: Disponible en: https://wiadlek.pl/wp-content/uploads/archive/2020/WLek202007129.pdf 15. [ Links ]
16. Tamayo MS, Real EG, Martín MLS, Crespo MC. Analgesia peridural torácica para el alivio del dolor posoperatorio en la cirugía torácica. Revista Cubana de Anestesiología y Reanimación [Internet]. 2018 [Citado 01/11/2022]; 17(2): 10-20. Disponible en: Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=85683 16. [ Links ]
17. Rabanal Llevot JM, Fayad Fayad M, Bartolomé Pacheco MJ, Carceller Malo JM, Naranjo Gómez S, Ortega Morales J. Eficacia del bloqueo paravertebral continuo como método analgésico en la toracotomía. Cir Esp [Internet]. 1 de julio de 2010 [Citado 01/11/2022]; 88(1):30-5. Disponible en: Disponible en: https://www.elsevier.es/es-revista-cirugia-espanola-36-articulo-eficacia-del-bloqueo-paravertebral-continuo-S0009739X10001181 17. [ Links ]
18. Marshall K, McLaughlin K. Pain Management in Thoracic Surgery. Thorac Surg Clin [Internet]. agosto de 2020 [Citado 01/11/2022]; 30(3): 339-46. Disponible en: Disponible en: https://doi.org/10.1016/j.thorsurg.2020.03.001 18. [ Links ]
19. Ma H, Song X, Li J, Wu G. Postoperative pain control with continuous paravertebral nerve block and intercostal nerve block after two-port video-assisted thoracic surgery. Wideochir Inne Tech Maloinwazyjne [Internet]. marzo de 2021 [Citado 01/11/2022]; 16(1): 273-81. Disponible en: Disponible en: https://doi.org/10.5114/wiitm.2020.99349 19. [ Links ]
Received: November 25, 2022; Accepted: November 28, 2022











 texto em
texto em 


