Introduction
Dental caries is still the major oral health problem for children worldwide.1 Unrestored active carious lesions is the main cause of pain2 and subsequent dental fear3 in childhood. The principles of minimally invasive dentistry allow dentists to pursue holistic and cause-based management of caries disease to maintain healthy functional primary teeth until exfoliation.4 Restorative treatments are performed to aid biofilm control, protect the pulp-dentin complex, and restore the integrity of the dental structure.4 Resin composite has been usually used for restoring primary teeth, since fits with concept of Minimally Invasive Dentistry, and meeting patients’ demands regarding esthetics.5 Nevertheless, there is a lack of supporting clinical data regarding the survival of resin composite restorations and risk factors that may dictate the service time of the treatment in children.6,7 Thereby, retrospective studies may provide data that reflect the survival of treatments in clinic daily life, where operator and patient-related variables are not controlled.
To the best our knowledge, this is the first study that investigated that the performance of resin composite restorations placed in Chilean children involved in an individualized treatment program based on caries risk assessment and management of caries disease. Thus, the aim of this clinical retrospective university-based study was to assess the survival and factors associated with failures of resin composite restorations performed in primary dentition of high caries risk Chilean children. The hypothesis of this study is that factors associated with cariogenic risk influence the longevity of composite resin restorations at 3 years of follow-up.
Methods
This manuscript was based on the STROBE 8 recommendations for cross sectional study.
The database with clinical records from the Pediatric Dentistry Clinic at the Postgraduate School of local University, was used in the present evaluation. The research protocol (Number 2018/09) was approved by the Local Research Ethics Committee. This pediatric dental clinic treats children at a low charge, who are mainly from low socioeconomic backgrounds.
The target population consisted of high-caries risk children attended by graduate students, supervised by specialists in Pediatric Dentistry, during the period between 2013 and 2016. A clinical retrospective study was conducted. To be included in the study, children should have received at least one resin composite restoration placed in any primary tooth, and patients should have at least one visit at the clinic after the restoration placement. Children with compromised systemic health or restored teeth with hypoplasia were excluded from the study.
All procedures were performed under rubber dam isolation using non-pharmacological behavior guidance techniques. Cavities were prepared with low-speed drills and dentin excavators for carious tissue removal and high-speed carbide burs for removing enamel and unsatisfactory restorations when necessary. In teeth with shallow or moderately deep cavitated lesions, complete carious tissue removal was performed. In deep cavitated lesions, selective removal to soft dentin was performed, i.e., soft tissue was left over the pulp to avoid exposure and “stress” to pulp. In all situations, cavity margins were left hard after removal with low-speed drills.9 In deep cavities the region close to the pulp was protected with a thin layer of glass ionomer cement (Vitrebond; 3M ESPE, St. Paul, MN, USA). The cavity was conditioned by 37 % phosphoric acid gel for 15s. The acid was removed by rinsing with water for 30s, and the cavity was gently dried with air and cotton pellets. The two-step etch-and-rinse adhesive system (Adper Single Bond, 3M ESPE, St. Paul, MN, USA) was used prior to the insertion of the resin composite (Filtek Z350 XT, shade A1; 3M ESPE, St. Paul, MN, USA) using the incremental technique. For the anterior and posterior proximal cavities, a matrix was adapted to the cervical margin. The rubber dam was then removed and the occlusion was checked. For all restorations, finishing and polishing were performed using fine-grained diamond burs, sandpaper strips and siliconized tips.
First, the history of the restorations was collected from the patient files. Factors potentially associated with treatment failure were investigated, including individual and clinical characteristics: age, gender (boys or girls), behavior (cooperative or non-cooperative), oral hygiene index (Greene-Vermillion modified - OHI-S < 1.1 or >1.2),10 type of tooth (anterior or posterior), number of restored surfaces (one or two or more), cavity depth (shallow, moderate or deep), and pulp intervention (yes or no).
In pediatric dentistry, patient-related factors can play an important role when considering behavior management. Most clinicians characterized children in one of three definable ways cooperative, noncooperative or potentially cooperative. The restoration performance can vary among patients, due to different conditions affecting the execution of the technique. Composite resin is highly sensitive to the technique and time-consuming.1
The performance of composite resins is completely affected by presence of water or saliva, this is a problem in noncooperative children, and in cases where moisture control is critical, the correct restoration can be jeopardized and a low performance can be expected. In our study, we used rubber dam to provide a dry operatory field, preventing saliva contamination while allowing a better view of the field. In a young age of pediatric patients associated with difficulties with behavior management it is sometimes impossible to adequately isolate molar to perform resin composite restoration, and in such occasion GIC and RMGIC are alternatives because these materials are less technique sensitive.11,12,13
The restorations were clinically evaluated between May and September 2018 independently by two trained and calibrated examiners (M.J.T. and M.P.C.) using dental11 explorer and mirror, based on modified United States Public Health Service (USPHS) criteria including marginal adaptation, marginal staining, and caries (table 1). In case of disagreement, the examiners evaluated the restorations jointly, until a consensus was reached. The calibration procedures considered the analysis of some restorations twice, randomly distributed, for Cohen’s Kappa calculation (Kappa = 0.84). Codes Alfa, Bravo, and Charlie were used to rate the restorations according to the assigned descriptive values for each characteristic of USPHS parameter. For clinical decision-making, the worst grading among all parameters was considered. The restorations were recorded as failed if they were classified as Bravo for caries or Charlie for the other parameters. Those patients who presented a treatment need during clinical evaluation were referred for treatment.
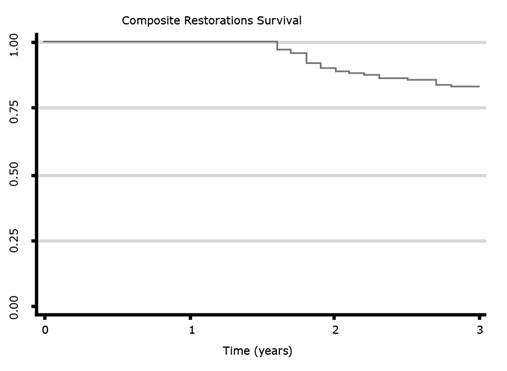
Data analyses were performed with STATA software 12.0 (Stata Corp., College Station, TX, USA). The descriptive analysis provides the distribution summary according to the independent variables. The annual failure rate (AFR) of the restorations was calculated according to the formula: (1- y)z =(1-x), in which “y” expresses the mean AFR and “x” the total failure rate at “z” years. Survival analysis was performed to assess factors associated with the longevity of the restorations, and data was censored at 3-year of follow-up. Survival curves of the restorations were assessed through the Kaplan-Meier method.
Multivariate Cox regression models with shared frailty were performed to identify factors associated with failure of the restorations. These models consider that observations within the same group (the patient) are correlated, sharing the same frailty, being analogous to multilevel regression models with random effects. Hazard ratios and their respective 95 % confidence intervals (HR; 95 % CI) were obtained. A backward stepwise procedure was used to select covariates in the fitting of the model. Only those variables presenting p values < 0.2 in the unadjusted assessment were selected for the multivariate analysis. A significant level of 5 % was considered for the final model.
Results
Two hundred and thirty restorations placed in 48 patients (23 boys and 25 girls) were included in the analysis. The mean age of the children was 5.1 years (±0.9), presenting a decayed, missing and filled - teeth (dmf-t) mean of 10.5 (± 3.4). The follow-up period ranged from 0.7 to 4.8 years with a mean of 2.7 (±1.04) years (table 1).
Table 1 Modified United States Public Health Service (USPHS) criteria (A=Alpha, B=Bravo, C=Charlie)
| USPHS Criteria | Code | Definition |
| Marginal adaptation | A | Restoration closely adapted to the tooth. No crevice visible. No explorer catch at the margins, or there was a catch in one direction. |
| B | Explorer catch. No visible evidence of a crevice into which the explorer could penetrate. No dentin or base visible. | |
| C | Explorer penetrates into a crevice that is of a depth that exposes dentin or base | |
| Marginal staining | A | No staining along cavosurface margin |
| B | < 50 % of cavosurface affected by stain | |
| C | > 50 % of cavosurface affected by stain | |
| Secondary caries | A | Absent |
| B | Present |
Table 2 shows the distribution of restorations and their rates of “success” according to individual and clinical-level variables. Among all restorations considered in the analysis, 151 (65.7 %) were placed in younger children (≤5 years) and 56.3 % girls, 43.7 % in boys. Posterior restorations were more common (82.6 %) than anterior ones (17.4 %), as well as those performed in deep cavities (76.1 %) when compared with shallow or moderate cavities (23.9 %). Most restorations were placed on vital teeth (94.8 %) and involved two or more surfaces (71.7 %). The majority of restorations were placed in children with cooperative behavior (68.7 %), which ingested sugar until six times daily (59.6 %), and presented poor biofilm control (80.0 %). The overall success rate was 75.2 % (173/230).
Table 2 Survival of resin composite restorations placed in primary teeth after 36 months follow-up, according to clinical features (n=230), expressed in N (%)
| Variables | Restorations | Success | Failure |
|---|---|---|---|
|
>5 years |
151 (65.7) 79 (34.3) |
107 (70.1) 66 (83.5) |
44 (29.1) 13 (16.5) |
|
dmft < 10 dmft >10 |
75 (32.6) 155 (67.4) |
60 (80.0) 113 (72.9) |
15 (20.0) 42 (27.1) |
|
Cooperative/pottencially Non-cooperative |
158 (68.7) 72 (31.3) |
126 (79.7) 47 (65.3) |
32 (20.3) 25 (34.7) |
|
< 1.1 > 1.2 |
46 (20.0) 184 (80.0) |
37 (80.4) 136 (73.9) |
9 (19.6) 48 (26.1) |
|
< 6 >6 |
137 (59.6) 93 (40.4) |
104 (75.9) 69 (74.2) |
33 (24.1) 24 (25.8) |
|
Anterior Posterior |
40 (17.4) 190 (82.6) |
28 (70.0) 145 (76.3) |
12 (30.0) 45 (23.7) |
|
1 2 or more |
65 (28.3) 165 (71.7) |
50 (76.9) 123 (74.5) |
15 (23.1) 42 (25.5) |
|
Shallow and moderate Deep |
55 (23.9) 175 (76.1) |
42 (76.4) 131 (74.9) |
13 (23.6) 44 (25.1) |
|
Yes No |
12 (5.2) 218 (94.8) |
7 (58.3) 166 (76.1) |
5 (41.7) 52 (23.9) |
*Oral Hygienic Index Green and Vermeillon modificate: over 1.2 is considered risk of caries.
*Pulp Treatment: Pulpotomy and Pulpectomy
Table 3 shows the unadjusted and adjusted Hazard Ratios (HR) for failures according to independent variables. The unadjusted model showed that restorations performed in children with dmf-t greater than 10, had more risk of failure in their restorations (p=0.04). However, this association lost significance in the adjusted analysis (p=0.08).
Table 3 Unadjusted and adjusted Hazard Ratios (HR;95 % CI) for failure of the restorations according to clinical and demographic characteristics. Cox regression model
| Independent variables | HCRc (95 % CI) | p-value | HRa (95 % CI) | p-value |
|---|---|---|---|---|
|
Male Female |
1.00 1.34 (0.27;6.71) |
0.71 | - | - |
|
< 5 years > 5 years |
1.00 0.36 (0.06;1.99) |
0.24 |
1.00 0.55 (0.10;3.02) |
0.49 |
|
<10 >10 |
1.00 6.11 (1.03;36.15) |
0.04 |
1.00 4.77 (0.80;28.36) |
0.08 |
|
<1.1 >1.2 |
1.00 0.67 (0.004;0,96) |
0.04 |
1.00 0.11 (0.009;1.34) |
0.08 |
|
Yes No |
1.00 0.29 (0.07;1.11) |
0.07 |
1.00 0.31 (0.08;1.15) |
0.08 |
The cumulative restoration survival estimate is shown in figure 1. Mean survival time was 2.7 years (95 % CI: 0.75-0.87) with 82.5 % of the restorations surviving after 3-year of evaluation. The overall AFR after 3-year follow-up was 6.2 %. The distribution of the restorations according to the USPHS criteria is summarized in Table 4. Most reason for restoration failure was marginal adaptation, and 16 % of the restoration failed for caries.
Discussion
The results of the clinical retrospective study demonstrated a satisfactory survival rate (82.5 %) of resin composite restorations placed in primary teeth of high caries-risk children. AFR was 6.2 % up to 3 years of follow-up. Previous retrospective studies found that AFR rates of resin composite restoration in primary teeth ranged from 4.2 %12 to 18.8 %.13 Child’ age, behavior guidance techniques used to perform treatment (pharmacological or non-pharmacological), sample size, operator experience, population profile, and criteria for failure can influence on the results. This study assessed the longevity of restorations in primary teeth using the USPHS,11 criteria, including marginal staining, marginal adaptation, and caries. We evaluated only these parameters because considered that the esthetic demand from the pediatric patient may be not a factor determining for restoration replacing as in adult population, and most restorations were placed in posterior teeth. Marginal defects were the most frequent reason for failure. It could be argued that the largest number of defective restorations observed reflect inappropriate restorative technique; although the restorative procedures were performed by graduate students, supervised by specialists in Pediatric Dentistry. Others retrospective studies12,14 also reported defective restorations (fracture and partial loss) in primary teeth were the most frequent reason for failure. Failed restorations due marginal pigmentation were considered when > 50 % of cavo-surface affected by stain. Marginal pigmentation can occur due degradation of bonding agents or penetration of dyes from dietetic habits; factors not directly associated to caries. In a systematic review on survival of restorations in primary teeth, recurrent caries was reported as the main reason for failure.15 Secondary caries has frequently described as the main reason for restoration replacement in high caries risk.16,17 The target population of our study consisted of high caries prevalence children, with a dmf-t mean of 10.5 (± 3.4). It is important to highlight that dental caries has a long course of progression due to its accumulative nature, and dmf-t reflects mainly the past history of the disease because caries activity is not contemplated. All children who attend the Pediatric Dental Service were treated for the management of caries disease and control activity of existing non-cavitated and cavitated lesions, receiving non- invasive treatments such as oral hygiene, dietary advice, prophylaxis and fluoride therapy, and all invasive procedures necessary. It may explain the high survival of resin composite restorations found in our study.
It has been evidenced that caries-active patients experienced more failures in their restorations when compared to caries-controlled patients. The 3-year survival of adhesive restorations for caries-active patients was 49.9 % (AFR=20.6 %), while for caries-controlled patients the longevity reached 77.7 % (AFR= 8.0 %).14 Although this variable was not collected in our study, we assumed that periodic recall program had a positive impact for a portion of the sample because only 16 % of the restorations failed for caries recurrent. Thus, these failures may be related to a failure in the periodic recall program or incomplete treatment plan for these patients. It is well established in the scientific literature that dental biofilm that the lifetime exposure to dental biofilm might be a risk factor for cumulative dental diseases, such as caries, failure of restorative treatments, and tooth loss.18
The oral hygiene index was not a significant restoration failure factor in our study (p=0.06). There is a paradigm shift in dentistry toward minimally invasive approaches. In our sample, complete carious tissue removal was performed in teeth with shallow or moderately deep cavitated lesions while selective carious tissue removal to soft dentin was indicated for deep cavitated lesions. The contemporary approach of managing carious lesions recommends selective carious tissue removal, irrespective of the depth of lesions.9 Selective carious tissue removal minimizes the risk of pulp exposure and post-operative 19 symptoms in deep carious lesions, reducing the discomfort for the patients.20 Even if the restorations present shortcomings over time, most could be repaired, allowing more conservative approaches for teeth with deep carious lesions.21,22,23 The results of this study should be viewed considering their possible methodological limitations. The retrospective design results in an obvious lack of standardization of indication and treatment protocols. On the other hand, they could reflect conditions closer to everyday practice, where uncontrolled settings provide high external validity.
The resin composite restorations placed in primary teeth of children involved in a management protocol based on caries risk assessment and management of caries disease presented satisfactory survival after 3-year of follow-up.