INTRODUCTION
Chronic subdural hematoma (CSDH) is an encapsulated collection of blood and fluid on the surface of the brain. Historically considered to be a result of head trauma, although recent evidence suggests that more complex processes are involved.1
Despite being a long-standing disease, many aspects of the epidemiology and natural history of CSDH remain to be elucidated. The global incidence is 1,72% to 20,6% per 100,000 people per year in the general population, being more common in the elderly.2
Multiple factors can modify the risk of developing CSDH, including older age and male gender. The increasing use of anticoagulants and antiplatelet drugs has also been associated with its progression.2
The formation of CSDH has not been clarified, but its pathophysiology rests on two fundamental theories: the osmotic gradient theory and the theory of recurrent bleeding, coming from the hematoma capsule, associated with hyperfibrinolysis. The gradual expansion of the hematoma by any of these mechanisms is responsible for the progression of symptoms.3
The treatment modality should be in accordance with the patient's symptoms and her clinical status. The non-surgical strategy includes the use of anti-inflammatory drugs such as dexamethasone, angiotensin-converting enzyme inhibitors, antifibrinolytics, and statins.4
There are several surgical techniques, such as Twist Drill (TD), burr hole craniotomy (BHC), and craniotomy/mini-craniotomy. In addition, there are other newly incorporated surgical variants such as embolization of the middle meningeal artery, and the use of endoscopy for solid clots.4) Each of these variants have indications, risks and differences between their results, as well as controversies in their use.
Recurrence of CSDH after treatment may occur in 3-20 % of all treated patients. Although a higher rate was found in conservatively managed patients, selection of high-risk patients for surgical intervention is likely to influence differences in recurrence rates.2
Many radiological parameters of CSDH have been reported to be associated with the risk of recurrence: unilateral or bilateral presence, thickness, midline shift, density and internal architecture, brain atrophy, and hematoma volume.5
However, studies have shown conflicting results and large discrepancies in recurrence rates due to heterogeneity in treatment, radiological measurement techniques, and variation in hematoma classifications by density or architecture.5
There are many controversies regarding surgical treatment by BHC: its single or double performance; the membranectomy; the use of drains, their duration and optimal place of placement; whether it is subdural or subgaleal; etc.
Few studies have investigated the variation in the number of drains placed in relation to recurrence, complications, or length of hospital stay.
In the present study, the possible influence of the placement of single or double drains in the cohort was analyzed. The following hypothesis is proposed: do patients with CSDH treated with double postoperative drainage have fewer complications at 30 days than those with single drainage? The objective was to analyze complications in patients with single or double drainage operated with CSDH.
METHOD
A correlational retrospective study was carried out in patients undergoing surgery for CSDH, at the Lucía Iñiguez Landín Clinical-Surgical Hospital, between January 2018 and December 2020.
The universe consisted of a total of 152 patients with a diagnosis of CSDH. Intentional sampling was applied through inclusion and exclusion criteria to obtain the sample. This was divided into 2 groups; the first formed by patients who used a subdural drain (n= 65), and the second group was in which two postoperative drains were used (n= 34). The total sample was 99 patients.
Inclusion criteria:
Exclusion criteria:
Presence of juxtadural or bilateral CSDH
Intervention through craniotomies and mini-craniotomies
Inadequate preparation of the clinical history
The information was obtained from medical records and imaging studies available on the image server of the Lucía Iñiguez Landín Hospital. The following variables were evaluated in both groups:
Age (years old)
Co-morbidities (previously diagnosed diseases)
Preoperative Glasgow Score (assessed at admission)
Characteristics of the hematoma (laterality, internal architecture according to the Nakaguchi scale,13 maximum diameter and displacement of reference structures from the midline)
Post-surgical complications at 30 days
Hospital stay (days).
For data processing, the Office Excel 2007 program was used. For statistical processing, the MYSTAT® software, version 12.02.00, was used. Continuous, normally distributed variables were expressed as means ± standard deviation (SD), qualitative variables were presented as total sum (with percentages). Statistical comparisons between single and double drain groups, with Pearson's correlation coefficient for quantitative variables. The probability value < 0.05 was considered statistically significant.
The data was obtained with the approval by the Scientific Research Ethics Committee and the Institution's Scientific Council, by resolution no. 07/2021. The ethical principles for this study were complied with in accordance with the provisions of the Declaration of Helsinki.
RESULTS
Of the 99 patients in the study, 39 of them were older than 75 years of age (table 1). Of the total number of cases, 34 suffered from arterial hypertension (AHT) and 4 from diabetes mellitus, 7 patients had a history of cerebrovascular disease and 8 had chronic obstructive pulmonary disease; 7 patients reported a history of ischemic heart disease.
Table 1 Distribution of patients in arithmetic mean and standard deviation according to number of post-surgical drainage
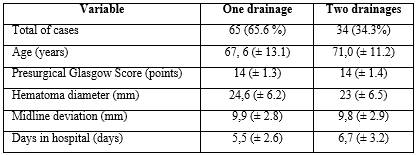
At admission, most patients in the single drainage group (57 patients) presented a Glasgow Score greater than 12 points, representing 87,69 %, while only 8,82 % of the cases in the double drainage group presented a lower score (table 2).
In the initial CT studies, the most frequent pattern was pattern B, with 25 cases (25,3 %) and the least frequent was pattern E, with only 8 cases (8,1 %). The diameter of the CSDH was more than 20 mm in 61 cases, and in 32 cases, the displacement of the midline structures was greater than 10 mm.
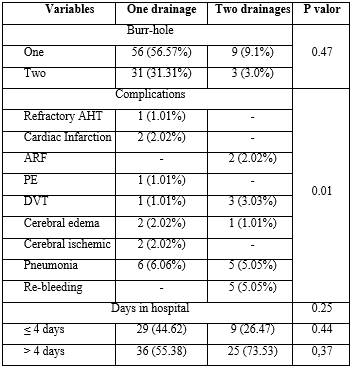
Table 2 Distribution of pre-operative variables in absolute number and percentage according to number of drainages
AHT: arterial hypertension; DM: diabetes mellitus; CVD: cardiovascular disease; COPD: chronic obstructive pulmonary disease.
Hospital stay averaged 5,8 days. The most frequent complication was pneumonia associated with health services with 11 cases (11,11 %) in the single drainage group, while cerebral edema was only observed in 1,01 % of the patients in the double drainage group.
A significant difference (p= 0,009) was found around the complication variables, so the double drainage group showed fewer complications at 60 days (table 3).
DISCUSSION
CSDH is a form of intracranial hemorrhage common in older adults. Optimal treatment remains controversial. CSDH surgery in older adults leads to favorable neurological outcomes, with a higher risk of systemic complications, recurrence or re-intervention of the hematoma, compared to younger patients.6
With regard to hospital stay, in patients with single drainage it was shorter, a fact that differs from the study by Pahatouridis et al.7) in which the duration was longer, which corresponds to the double drainage group of the present investigation; the highest percentage of patients were operated on for a single burr hole and with a single drain, which differs from the design of the Greek study, which is why the length of stay in this group was longer.
CT is a powerful tool to diagnose subdural hematoma and to define its prognostic factors.8 The modified Nakaguchi classification9) allows estimating the degree of recurrence in the postoperative period, in particular, CSDH with hyperdense components or with laminar or separated architecture, have higher rates of recurrence.8,10 In the series presented by the authors, the lowest number of patients in both groups presented these types, which is related to the low incidence of rebleeding obtained.
Evacuation of the hematoma through single or double burr-holes is the treatment of choice, due to its low morbidity and mortality rates and its less invasive nature.7
In the present series, the largest number of patients underwent surgery for a single trephine, taking into account the premise that unilocular CSDH can be efficiently drained and irrigated, without the need for an additional burr-hole, as a single cavity containing a fluid liquid. Performing a single burr-hole has also been associated with less surgical time and a low recurrence rate.11
The use of subdural drains results in a significantly improved postoperative image, which provides a valuable tool for postoperative imaging and clinical correlation.12
Nakaguchi et al.13 in 2000 reported that patients with single frontal drainage showed a lower rate of recurrence than those with occipital or parietal drainage following BHC. Other authors show recurrence rates, for the placement of single frontal drains, between five and 11,4 %.14
There are few studies evaluating the placement of one versus two subdural drains. Gernsback et al.15) reported that there is a lower tendency for recurrence in those patients with two drains compared to the group with a single drain, but this difference was not significant.
However, Qiangjun Wu et al.14 in 2020, conclude that the placement of double drains is superior to the placement of a single frontal drain in the surgical treatment of CSDH with a significantly lower recurrence rate. These results agree with the results of our study.
Among the limitations of this study are: the low number of cases, the patients were not operated on by the same surgical team, the choice of the number of drains was at the decision of the acting surgeon, the short post-surgical follow-up time, and only post-operative head CT was performed in patients who presented clinical deterioration or persistent neurological deficit.
The placement of double subdural drainage in patients with CSDH operated through single or double burr-holes is related to fewer complications than those with single drainage.