INTRODUCTION
According to the World Health Organization (WHO), an estimate of 525 000 children under five years of age die every year due to diarrheal infections. Moreover, 1.7 billion cases of infantile diarrheal diseases are reported every year worldwide. Gastroenteritis is a frequent clinical entity in developing countries mainly affecting people who live in impoverished areas.1 As published by the Ministry of Public Health [Ministerio de Salud Pública] of Ecuador in 2016, diarrhea and gastroenteritis of presumed infectious origin (CIE 10; A09), was the sixth and the fourth leading cause of morbidity in the ambulatory care services and hospitalization, respectively.2 Acute gastroenteritis could be produced by a variety of enteropathogens which includes virus, bacteria, and parasites; as a consequence of ingestion of foods improperly prepared or mishandled food service establishments, markets, or even at home.3 Bacterial infection due to pathogens such as Campylobacter, Escherichia coli, Salmonella, Shigella or Vibrio cholerae, are responsible for 20-40 % of diarrheal cases and contributes to high mortality in children from developing regions 4. The genus Shigella comprises four species: S. dysenteriae (group A), S. flexneri (group B), S. boydii (group C) and S. sonnei (group D). Furthermore, its infection typically produces diarrhea characterized by frequent passage of small liquid stools that contain visible blood, with or without mucus, abdominal cramps, tenesmus (unproductive, painful straining), fever and anorexia. However, patients may only present acute watery diarrhea.5 The increasing rate of resistance to antimicrobial drugs by Shigella is a public health problem that should concern the health providers globally, particularly nowadays when resistance to ciprofloxacin, third-generation cephalosporin and macrolides, is emerging.6) This case report aims to present the first case of a gastrointestinal infection provoked by Shigella flexneri producer of extended-spectrum beta-lactamase (ESBL) reported in the Hospital of Specialties of the Armed Forces N° 1 (Hospital de Especialidades de las Fuerzas Armadas No. 1 [HE-1]), Quito, Ecuador.
CASE PRESENTATION
Male 7-year-old patient, native-born and resident at Quito, who is a regular student in elementary school, with a personal pathological history of constipation for about three years. On 23rd January 2017, he presented with dysenteric syndrome at the HE-1, where blood and stool tests were performed, evidencing a gastrointestinal infection, so his admission was decided. The patient improved after 3 days of ceftriaxone, acetaminophen, and probiotics; thus the hospital discharge was decided with antibiotic home treatment. However, the result of the stool culture and antibiogram test was still pending.
On the 2nd February 2017, nine days after hospital discharge, the patient was taken to the emergency department of HE-1, with clinical onset of abdominal pain, fever of 39 °C (102.2 °F) and frequent passage of small liquid stools. His vital signs at admission were, pulse rate 143 beats per minute (BPM); respiratory rate 26 breaths per minute (BrPM); oxygen saturation of 92 %; weight 19.2 kg (Z-score -1.65) and height 115 cm (Z-score -1.6). During the physical examination, abdominal pain was observed after applying pressure over the umbilical, hypo-gastric and right iliac regions. Nevertheless, there was no evidence of other signs that suggest appendicitis. At the emergency department, he received 270 mg of acetaminophen without improving. Then, the patient was accepted in the pediatric unit, after which blood and stool samples were taken with precautions of asepsis and antisepsis, for laboratory investigations including complete blood count (CBC), c-reactive protein (CRP), procalcitonin (PCT), blood chemistry tests, coproparasitary examination and stool culture. In addition to this examination, abdominal x-ray and abdominal echography were achieved. The results of the previous stool culture were received, according to which antibiotic treatment was initiated. The evolution of the patient, the test results and the prescriptions are detailed in table 1.
Table 1 Timeline
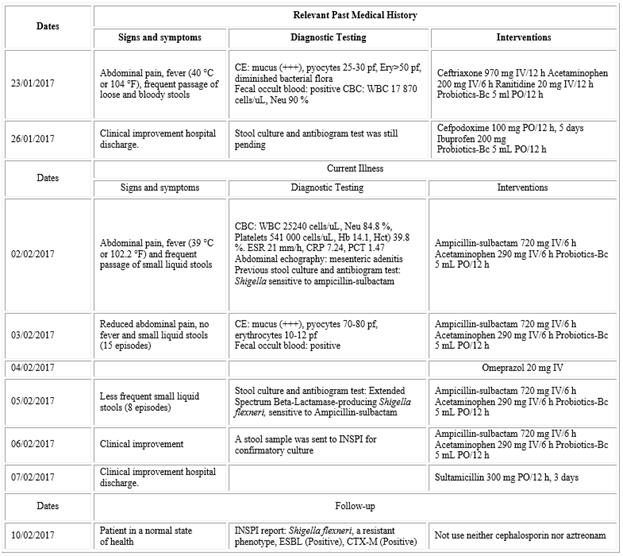
CE: coproparasitary examination; Ery: erythrocytes; CBC: complete blood count; WBC: white blood cells; Neu: neutrophils; Hb: hemoglobin; Hct: hematocrit; IV: intravenous administration; PO: oral administration; BC: Bacillus clausii; ESR: erythrocyte sedimentation rate; CRP: c-reactive protein; PCT: procalcitonin: INSPI: Instituto Nacional de Investigación en Salud Pública (National Institute of Public Health Research.
Tests findings
The laboratory tests performed on the second hospital admission reported a notable neutrophilic leukocytosis and an increase in acute phase reactants. The clinical parameters of blood chemistry tests and urinalysis were found normal. The abdominal echography reported mesenteric adenitis. The microscopic examination of stool demonstrated mucus, pyocytes and erythrocytes. The stool specimen was plated in two ml of Mueller Kaufmann Tetrathionate Broth and then incubated at 35 °C for two hours. After that, subcultures were realized in Hektoen Enteric Agar and chromogenic media, which were incubated at 35 °C during 18 to 24 h. As a result, numerous nonlactose fermenting colonies were observed, which were picked and processed for biochemical characterization in Triple Sugar Iron Agar (TSI), Motility Indole Ornithine Medium (MIO), and Urea Broth Base. Additionally, an ESBL Chromogenic Media was employed. The biochemical and microbiological results are shown in table 2.
Table 2 Biochemical results in the microbiological isolation of Shigella
TSI: triple sugar iron agar medium; SIM: sulfide indole motility medium; MIO: motility indole ornithine medium; MRVP: methyl red Voges Proskauer broth; ESBL: extended spectrum beta lactamase.
The methods utilized for the antibiogram were automated (Vitek compact 2) and disk diffusion (Kirby-Bauer), both for the minimum inhibitory concentration (MIC) and for the diameter of the inhibition halo.
Phenotypic ESBL detection was based on the inhibitory activity of clavulanic acid. Summarily, we inoculated a bacterial suspension in a Müller-Hinton agar plate; then, cephalosporin was placed at a certain distance (30 mm-20 mm) from the clavulanic acid. An expansion of 5mm in the area within the inhibition halos confirmed the presence of an ESBL bacterium.
We used paper strips filled with antibiotics to perform the E-test technique. One-half contained cephalosporin in decreasing levels, as the other half held cephalosporin in reducing concentrations with clavulanic acid in a fixed concentration of 2 μg. The synergy of these antibiotics was considered positive when the MIC decreased in two or more dilutions. The results were evaluated according to de National Committee for Clinical Laboratory Standards (NCCLS) 2015.
Diagnostic reasoning
Before obtaining the results of stool culture and antibiogram presented by the microbiology laboratory, we found some clinical aspects that could guide us to consider a gastroenteritis caused by ESBL producing Shigella. First of all, shigellosis induces a clinical picture characterized by fever, abdominal pain, and tenesmus, as well as the frequent passage of small liquid stools that contain blood, with or without mucus. All of these features were present in our patient. However, the only method to discard other invasive infectious gastroenteritis is the stool culture; because, without its help, we should consider pathogens such as Escherichia coli, Salmonella, Yersinia, Campylobacter, or even Entamoeba histolytica. Also, the complementary tests showed neutrophilic leukocytosis, a gastrointestinal bacterial infection suggested by the microscopical examination of stool, and mesenteric adenitis revealed on imaging.
In the previous treatment, the patient received ceftriaxone, but there was a relapse, suggesting in the context of our patient, an infection caused by an ESBL producer enteric bacilli. Therefore, the antibiogram was essential to establish a correct management.
Follow-up and outcomes
As reported by the antibiogram in the HE-1, the pathogen was sensible to ampicillin-sulbactam (table 3). Thus, the initial management was maintained during all the five days of hospital stay. After the first day in the pediatric unit, fever disappeared, and abdominal cramps decreased its severity. Nonetheless, frequent passage of watery, loose stools continued up to 6 February 2017, when depositions became normal. The clinical evolution of our patient was entirely favorable, so the hospital discharge was decided with oral rehydration and dietary care.
Three days after the patient left the hospital, was attended on ambulatory consultation, referring a good health state and absence of abdominal pain, diarrhea or fever. The patient did not have any relapse until the moment this work was written.
Table 3 Antibiogram ofShigella flexneri
HE-1: Hospital of Specialties of the Armed Forces N° 1 [Hospital de Especialidades de las Fuerzas Armadas No. 1] (HE-1); INSPI: National Institute of Public Health Research (Instituto Nacional de Investigación en Salud Pública); TMP/SMX: Trimethoprim/sulfamethoxazole.
Microbiologically confirmed ESBL/CTX-Producing Shigella flexneri by the National Institute of Public Health Research (INSPI, Instituto Nacional de Investigación en Salud Pública).
INSPI, former National Institute of Hygiene and Tropical Medicine "Leopoldo Izquieta Pérez," is a National Reference Institution in research, development, and innovation, which aims to increase efficiency and effectiveness of the provision of services of a specialized laboratory of national reference, to contribute the surveillance of public health.
A stool sample was sent on 6 February 2017 to the INSPI to confirm our result, as this was the first case of ESBL/CTX-producing Shigella flexneri reported in the history of the microbiology department in the HE-1 (INSPI-code; HM10173-0217RAM-Q). The INSPI reported a resistant phenotype, ESBL positive, CTX-M positive and suggested not to use neither cephalosporin nor aztreonam.
DISCUSSION
Shigellosis is a primary global public health concern, with approximately 167 million cases and over a million deaths annually globally, often in children under five years of age and in underdeveloped countries. Shigella species has four subgroups: Shigella flexneri, S. dysenteriae, S. boydii and S. sonnei. Among these, S. flexneri is the most common cause of endemic shigellosis.7) The mechanism of pathogenesis of S. flexneri consists in the capacity to penetrate and replicate within the colonic epithelium, which produces severe inflammation and epithelial damage. A model which explains how Shigella promotes the production of pro-inflammatory cytokines during intestinal inflammation, proposes that through the control of GSK-3β kinase, β-catenin and NF-κB, up-regulates the expression of interleukin 8, well-known as neutrophils chemotactic, among others.8) The excessive production of microbicidal products, as well as specific enzymes by the neutrophils, could explain the intense damage produced during Shigella infection, clinically characterized in the majority of cases by dysentery, abdominal cramps, tenesmus, and fever.9
In this case report, our patient presented with signs and symptoms of bacillary dysentery including, abdominal pain, fever and frequent passage of small liquid stools. The laboratory findings demonstrated an increase in neutrophils percentage and white blood cells in the CBC. In the same way, the microscopic examination of stool confirmed a significant number of pyocytes, erythrocytes, and mucus. In spite of these findings, the stool culture among with biochemical tests, and proper isolation of Shigella flexneri confirmed the diagnostic of gastroenteritis caused by enteric bacilli. Our patient was treated initially with ceftriaxone, but the antibiogram was pending at the hospital discharge. Consequently, he suffered a relapse with the same clinical characteristics. In fact, the antibiogram revealed the presence of an ESBL producing Shigella, a reason that could explain why the patient relapsed.
As this was the first case of an infection caused by an ESBL producing Shigella flexneri in the HE-1, a stool sample was sent to the INSPI which confirms our results reporting a CTX-M type ESBL producing Shigella flexneri. However, a limitation to us was the impossibility of a detailed identification of ESBL genes and molecular characteristics of the bacterial isolates. It is necessary to remark a previous report of Shigella sonnei harboring blaCTX-M-55 in Ecuador, which was the first description outside Asia, this is particularly relevant in the frame of recent data suggesting that Asiatic bacteria resistance determinants, including blaCTX-M-55, are present in our location. Nevertheless, more studies designed to clarify this affirmation are required as there is a possibility of the dispersion of multidrug-resistant bacteria among different geographical regions.10
Previous case reports in Latin America showed the emerging antimicrobial resistance of Shigella; in Peru, two cases of children affected by ESBL producing Shigella flexneri were reported in 2013, as well as, in Argentina one case of ESBL producing Shigella sonnei was published in 2001.11,12) Correspondingly, ESBL Shigella was identified in other countries such as Nepal, India, Pakistan, Bangladesh, among others.13) The resistance of Enterobacteriaceae, particularly to β-lactam antibiotics, is characterized by diverse mechanisms like chromosomal enzymes, membrane impermeability, drug efflux and the current paradigm of mobile gene pools. In this fashion, a study conducted in Bangladesh suggests that the ESBL producing plasmid might be transferred between E. coli and S. sonnei through conjugation in the human gut.14,15) In fact, the acquisition of a virulence plasmid is an essential phenomenon in the evolution of Shigella from a non-pathogenic Escherichia coli ancestor to a pathogenic genus. A current investigation highlights the value of coordination between heterologous genes and the host chromosome in the evolution of bacterial species.16 Additionally, in a previous report we found 16.95 % of cases affected by ESBL producing E. coli in children hospitalized by urinary tract infection in the HE-1. Therefore, is necessary the implementation of guidelines to improve the adequate empiric antibiotic therapy in the management of infections caused by enteric bacilli.17) On the basis that WHO recommends the appropriate antibiotic selection in the treatment of infection, some alternatives had been suggested. A Cochrane systematic review shows that there is no strong evidence to suggest a particular class of antibiotics as the trials included present antimicrobial effectiveness against isolates of Shigella dysentery by ampicillin, cotrimoxazole, nalidixic acid, fluoroquinolones, pivmecillinam, ceftriaxone, and azithromycin.18) Thus, the establishment of protocols for the empiric management of dysentery should be developed according to the local rates of antimicrobial resistance. Also, in spite of fluoroquinolones and cephalosporins are the pillar of the treatment of severe cases of shigellosis, the reports of multidrug-resistant strains are needed to consider the use of azithromycin as a valid alternative in the empirical therapy, something that could prevent the increasing bacterial resistance to fluoroquinolones and third-generation cephalosporins.
To conclude, the increasing reports of ESBL producing Shigella represents a problem to the management of dysentery as ceftriaxone and ciprofloxacin are often used as empiric antimicrobial therapy. Furthermore, this represents a severe obstacle to the national public health in low-income countries since the infections caused by multidrug-resistant bacteria could increase the necessary time to treat common pathologies, as well as the mortality rates. Consequently, the cost of management could increase affecting many people, especially those who suffer poverty. The adequate clinical diagnosis in a patient with gastroenteritis followed by the appropriate laboratory studies which include the stool culture and antibiogram are essential to give a proper antibiotic therapy in infections caused by Shigella strains and other enteric bacilli. We recommend publishing the different antimicrobial resistance patterns among health institutions to create politics that control the inadequate use of antibiotics, for the sake of the patients suffering infectious diseases, especially in vulnerable groups.














