My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Cubana de Estomatología
Print version ISSN 0034-7507
Rev Cubana Estomatol vol.51 no.1 Ciudad de La Habana Jan.-Mar. 2014
Rev Cubana Estomatol. 2014;51(1)
PRESENTACIÓN DE CASO
Severe osteonecrosis of the jaws in a compromised patient subjected to bisphosphonate therapy
Osteonecrosis severa de los maxilares asociada al uso de bifosfonatos
Juliana Dreyer de Menezes, PhD. Nicole de Mello Rahde, PhD. Fernanda Gonçalves Salum,PhD. Maria Antonia Figueiredo, PhD. Karen Cherubini
Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, RS, Brazil.
ABSTRACT
Bisphosphonate-related osteonecrosis of the jaws is characterized by alveolar bone exposure, especially after mucosal trauma or after surgical procedures, in patients who have previously received or who are currently receiving bisphosphonates without a history of radiation therapy in the maxillofacial region. The condition is refractory to treatment, and attempts at debridement are not completely effective in eradicating the necrotic bone. We report here a case of a severe osteonecrosis of the jaws in a 77-year-old male patient, who had been subjected to chemotherapy and treatment with zoledronic acid and corticosteroid. The patient also had comorbidities such as diabetes and periodontal disease, which might have contributed to the lesion development. Bisphosphonate-related osteonecrosis of the jaws has become a reality in dental clinical practice. Although palliative treatment aiming at controlling pain, infection and injury progression is indicated, the therapeutic strategy is still challenging. So far, the best approach available is prevention, based on oral care before, during, and after bisphosphonate therapy.
Keywords: osteonecrosis, bisphosphonates, bone remodeling, jaw diseases.
RESUMEN
La osteonecrosis de los maxilares asociada al uso de bifosfonatos se traduce en la aparición de hueso alveolar expuesto y necrótico, especialmente después de un trauma de la mucosa o después de procedimientos quirúrgicos, en pacientes que han recibido previamente o que están recibiendo bifosfonatos pero sin historia de radioterapia a región máxilofacial. La afección es refractaria al tratamiento, y los intentos de desbridamiento no son totalmente eficaces en la erradicación del hueso necrótico. Se presenta aquí un caso de una grave osteonecrosis de los maxilares en un paciente masculino de 77 años de edad, que había sido sometido a quimioterapia y tratamiento con ácido zoledrónico y corticosteroides. El paciente también tenía comorbilidades como diabetes y enfermedad periodontal, que pueden haber contribuido al desarrollo de la lesión. El creciente número de casos de esta enfermedad en la literatura ha llamado la atención. Dado que el enfoque terapéutico sigue siendo difícil, la prevención es la mejor estrategia disponible.
Palabras clave: osteonecrosis, bisfosfonatos, remodelado óseo, enfermedades de los maxilares.
INTRODUCTION
Bisphosphonates are the drugs of choice to treat osteoporosis, multiple myeloma, hypercalcemia of malignancy and bone metastases, especially those associated with breast and prostate cancer. They can also be used to treat Paget's disease, osteogenesis imperfecta, and idiopathic juvenile or steroid-induced osteoporosis.1 In 2003, a warning to the medical community was published in the Journal of Oral and Maxillofacial Surgery, which reported 36 cases of jaw osteonecrosis associated with the use of the intravenous bisphosphonates pamidronate and zoledronic acid.2 The injury can occur spontaneously or after invasive surgeries such as tooth extractions, periodontal surgery, apicoectomy, dental implants or mucosal trauma, often associated with ill-fitted dentures.3 The repair process delay leads to prolonged exposure of bone tissue in the oral cavity and osteonecrosis. As the healing does not occur, the lesions become infected and osteonecrosis is perpetuated.4 We report here a case of severe osteonecrosis of the jaws in a compromised patient subjected to bisphosphonate therapy, discussing the clinical aspects concerning this injury.
CASE REPORT
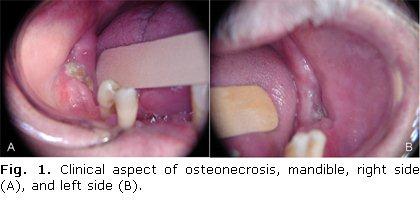
A 77-year-old male Caucasian patient was referred to the stomatology department for evaluation of a jaw injury, lasting one year, which had developed after tooth extractions. The medical history included prostate carcinoma six years prior, treated by surgical resection, which was followed by bone metastases. Metastases were treated with radio- and chemotherapy as well as the administration of zoledronic acid, 4 mg monthly for 17 months. The patient also reported diabetes and daily use of prednisone. Physical examination exhibited bilateral mandible bone tissue exposures measuring 2.0 cm X 0.5 cm on the right side (Fig.1A) and 1.0 cm X 0.5 cm on the left side (Fig.1B).
There was also swelling in the submental region with cutaneous erythema, pain, and mild increase in local temperature. On panoramic radiographic examination, radiolucent areas were observed in the body of the mandible (Fig. 2).
Computed tomography showed changes in anatomical structure of the mandible with areas of condensation and fragmentation of bone, and the presence of free fragments in the region of the right lower molars, left pre-molars and molars, and mental region, involving basilar and sub-apical area, with fracture risk in the left mental foramen region. Areas of bone condensation were observed adjacent to those already described and also reaching the mandibular ramus and the region underlying the mandibular canal. The images were compatible with osteonecrosis of the jaw.
Clinico-radiographic diagnosis was bisphosphonate-related osteonecrosis of the jaw. Therapeutic approach consisted of amoxicillin 500 mg (t.i.d.) and chlorhexidine 0.12 % oral rinse (t.i.d.). After the start of therapy, there was resolution of edema and erythema, allowing afterwards antibiotic withdrawal. Two bone fragments were released spontaneously, whose histopathological examination showed non-vital bone, lymphoplasmacytic and polymorphonuclear neutrophil infiltrate, as well as microbial colonies consistent with Actinomyces sp. (Fig. 3). Eight months later, a new x-ray showed some improvement of the radiographic features but without complete resolution.
.
DISCUSSION
Although IV bisphosphonate can by itself determine jaw osteonecrosis in individuals subjected to tooth extractions,5 its association with chemotherapy and chronic use of drugs such as steroids can affect the repair of the extraction wound even more.4 The duration of the treatment and number of infusions to which patient has been exposed have been identified as significant risk factors. Bamias et al.6 observed that the minimum number of bisphosphonate infusions prior to the onset of osteonecrosis was 13. Other factors such as age over 65 and periodontal disease may increase the risk.7,8 The present report shows a case of an old man who received 17 zoledronic acid infusions and had tooth extractions after using the drug. Moreover, medical history included diabetes and use of both steroids and chemotherapy. These factors confirm the reports in the literature on risk factors for the occurrence of the injury. Also, the periodontal disease presented by this patient was an important comorbidity which might have contributed to the development of the lesion.
In general, bisphosphonate-related osteonecrosis patients exhibit the infectious process to a greater or lesser degree, and this is usually responsible for painful symptoms. In this case, the swelling and cutaneous erythema in the submental region, and the pain reported by the patient went into remission after starting the antibiotic therapy. The maintenance of topical therapy, in turn, aimed to prevent the exacerbation of the injury. Moreover, as the patient reported two previous unsuccessful surgeries, it was decided at first not to perform any surgical intervention.
The anatomical site affected by osteonecrosis in this report (mandible) is considered the most prevalent one, followed by the maxilla and with the lowest prevalence for occurrence in the maxilla and mandible simultaneously. It is not clear why these lesions affect almost exclusively the jaws. However, it is known this is due in part to the high turnover of alveolar bone as well as to the exposure of jaw to the outside environment through the teeth and periodontal ligament.9,10 Otherwise, pathological fracture is not a common finding, unless debridement surgeries have been performed, which reduce the structural integrity of bone.7 Accordingly, in this report, the severity of the lesion and the risk of mandible fracture might have been favored by the two previous surgical procedures performed.
Bisphosphonate-related osteonecrosis of the jaws has become a reality in dental clinical practice. Although palliative treatment aiming at controlling pain, infection and injury progression is indicated, the therapeutic strategy is still challenging. So far, the best approach available is prevention, based on oral care before, during, and after bisphosphonate therapy.
REFERENCES
1. Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaw -2009 update. Aust Endod J [serial on the Internet]. 2009 [cited 2013 Jun 28];35:119-30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19961450
2. Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115-7.
3. Vescovi P, Campisi G, Fusco V, Mergoni G, Manfredi M, Merigo E, et al. Surgery-triggered and non surgery-triggered Bisphosphonate-related Osteonecrosis of the Jaws (BRONJ): A retrospective analysis of 567 cases in an Italian multicenter study. Oral Oncol. 2011;47:191-4.
4. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527-34.
5. Maahs MP, Azambuja AA, Campos MM, Salum FG, Cherubini K. Association between bisphosphonates and jaw osteonecrosis: a study in Wistar rats. Head Neck. 2011;33:199-207.
6. Bamias A, Kastritis E, Bamia C, Moulopoulos LA, Melakopoulos I, Bozas G, et al. Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol 2005;23:8580-7.
7. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567-75.
8. Bagan JV, Jimenez Y, Murillo J, Hernandez S, Poveda R, Sanchis JM, et al. Jaw osteonecrosis associated with bisphosphonates: multiple exposed areas and its relationship to teeth extractions. Study of 20 cases. Oral Oncol. 2006;42:327-9.
9. Coskun Benlidayi I, Guzel R. Oral bisphosphonate related osteonecrosis of the jaw: a challenging adverse effect. ISRN Rheumatol [serial on the Internet] 2013 [cited 2013 Jun 28];2013:215034. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23762600
10. Allen MR, Burr DB. The pathogenesis of bisphosphonate-related osteonecrosis of the jaw: so many hypotheses, so few data. J Oral Maxillofac Surg [serial on the Internet]. 2009 [cited 2013 Jun 28];67:61-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19371816
Recibido: 10 de agosto de 2012.
Aprobado: 7 de noviembre de 2013.
Juliana Dreyer de Menezes. Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, RS, Brazil.
Corresponding author Karen Cherubini Serviço de Estomatologia. Av. Ipiranga 6690, Sala 231, Hospital São Lucas PUCRS, CEP 90610-000.
Porto Alegre, RS, Brazil. E- mail: kebini.ez@terra.com.br; karen.cherubini@pucrs.br