Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Cubana de Estomatología
versión impresa ISSN 0034-7507versión On-line ISSN 1561-297X
Rev Cubana Estomatol vol.52 no.4 Ciudad de La Habana oct.-dic. 2015
ARTÍCULO DE REVISIÓN
Efficacy of combined radiotherapy and chemotherapy versus radiotherapy for oral squamous cell carcinoma
Eficacia de la radioterapia y la quimioterapia combinadas comparada con la radioterapia en el carcinoma oral de células escamosas
Jaime Irisarri Arévalo, Patricio Oliva Mella
Facultad de Ciencias de la Salud. Universidad del Desarrollo. Concepción, Chile.
ABSTRACT
Introduction: in the last decade, with all the advanced medical research in the treatments for cancer, there is a constant debate for the best possible treatment for oral squamous cell carcinomas. Radiotherapy with surgery has they compared with the addition of chemotherapy for control of the disease or survival of the patient.
Objective: to compare the effectiveness of radiotherapy with combined chemotherapy and radiotherapy for the control of oral squamous cell carcinomas
Methods: it was a systematic review with meta-analysis. Randomized trials in all phases were search with specific inclusion criteria through electronic database, hand searching and contacting experts in the field. After exclusion, criteria and the use of critical review checklist, three trials they selected for analysis. Three randomized trials representing 508 patients they identified. Some trials they analyzed in Review manager software 5.0®. The fix effect model they chosen for the statistical analysis, assuming that any observed variation in the score was an error of the specific article, with a confidence of 95 % (CI 1.13–2.77). The I2 presents percent of heterogeneity of 0 %, indicating that there is no clinically significant change in the results of the studies included
Result: evidenced the significance of 0.44 (higher than 0.05) in the chi square test indicating that the results are homogeneous or clinically similar. The Forest plot is located in the experimental group (chemotherapy and radiotherapy), establishing the clinical recommendation of use.
Conclusion: the usage of chemotherapy treatment in combination of radiotherapy regimen they recommended as for its promising results. Not also, the overall survival has improved, survival and distant metastasis free rates improve.
Keywords: carcinoma, squamous-cell, radiotherapy, chemotherapy, cancer oral.
RESUMEN
Introducción: en la última década se ha avanzado en tratamientos para el cáncer; sin embargo, se mantiene un debate constante para determinar el mejor tratamiento para los carcinomas orales de células escamosas. El tratamiento combinado de radioterapia y cirugía fue comparado con la quimioterapia para el control de la enfermedad o la supervivencia de la paciente.
Objetivo: comparar la efectividad de la radioterapia con la radioterapia y quimioterapia combinadas para el control de los carcinomas de células escamosas orales.
Métodos: se realizó una revisión sistemática con metaanálisis. Se buscaron ensayos aleatorios en todas las fases a través de bases de datos, búsquedas manuales y el contacto con expertos. Después de evaluar los criterios de selección y el uso de lista de revisión crítica, se seleccionaron tres ensayos para el análisis identificando tres ensayos aleatorios que incluyendo 508 pacientes. Se analizaron con el software Review manager 5.0®. Para el análisis estadístico se eligió el modelo de efecto fijo, con una confianza de 95 % (IC 1,13-2,77). El I2 presenta el porcentaje de la heterogeneidad de 0 %, lo cual indica que no existe una variación clínicamente significativa en los resultados de los estudios incorporados
Resultado: se evidencia una significación de 0,44 (superior a 0,05) en la prueba de chi cuadrado, esto indica que los resultados son homogéneos o clínicamente similares. La medida de resumen del Forest Plot se sitúa en el grupo experimental (quimioterapia y radioterapia), el establecimiento de la recomendación clínica de uso.
Conclusión: el uso de un tratamiento de quimioterapia en combinación con radioterapia es recomendable. La supervivencia en general ha mejorado y las tasas libres de metástasis también mejoran.
Palabras clave: carcinoma de células escamosas, radioterapia, quimioterapia, cáncer oral.
INTRODUCTION
The squamous cell carcinoma (SCC) is a type of cancer that affects epithelial tissue, specifically the squamous cells in the skin. It has others names like epidermoid carcinoma and squamous cell epithelioma 90 % of all neck and head tumors are of squamous cell origin and the world annual incidence is an estimate of 363.000 with a mortality of 200.000.1,2 It believes that the etiology of all SCC lesions stats as an uncontrolled and repetitive epithelial mother cell divisions. The accumulation of these neoplasic cells causes a microscopic group of abnormal cells that initially stays confined in one tissue, where the original epithelial cell mutated. There is a great variety of risk and causes for the development of a neck and head cancer, age and gender, tobacco, alcohol, diet, exposure to certain chemicals and the human papilloma virus.1
The treatment for these cancers is for great medical and economic importance.2 Therapeutic strategies combine surgical resection of the tumor including a safety margin, continued with radiation at the original mutated zone and lymph drainage areas.2
Since the 1970´s, the conventional treatment for resectable tumors has been surgery with postoperative radiotherapy (with 5-year survival rates ranging from 10 % to 60 %).3
The Mohs surgical technic consists in a block resection of the tumor area and a sample of the area, then immediately a pathologist observes this sample at a microscope for neoplasic cells signs and gives the order of leaving a safety margin or make a bigger resection, repeating the technic until there are no signs of irregularities.4
In some small lesions, all the surgery can they done with regular resections, moretypically; however, a mandibulectomy or a mandibular lingual releasing approach is required to allow access for resection of larger carcinomas, with the appropriate micro vascular free flap reconstruction.5
The squamous cell carcinoma is treatable normally with a combination of surgery and radiotherapy. The election of the treatment method depends on the health center's protocol, and also the aggressiveness and location of the tumor. Generally, if you can obtain a normal tissue sample, the surgical resection is the habitual method, followed by radiotherapy. Currently, the tendency of adding chemotherapy is increasing with the surgical and radiotherapy treatment.6 The benefit of chemotherapy added to loco-regional treatment is well established. It they also known that chemotherapy should be administered concomitantly with radiation therapy, while the cytotoxic agent best suited for chemo radiation is still under investigation. An ideal agent should be a potent radio sensitizer, and it should be reasonably well tolerated.7
The research question they structured as follows: Is the radiotherapy and chemotherapy based treatment more effective than the radiotherapy treatment for patients with oral squamous cell carcinoma? The purpose and objective of this study is to determine the efficacy of chemotherapy and radiotherapy compared with only radiotherapy treatment. We want to know which one are effective clinical treatments for the patient.
METHODS
As at all meta-analysis implies, the study design, search strategy. It is a systematic analysis of published clinical trials, and then analyzed statistically using a meta-analysis that allows a clinical decision.
Inclusion criteria:
- The investigation includes only randomized trials, in any phase (I, II, III and IV),
- That include adult patients (human, age 18 or older) with histologically confirmed squamous cell carcinoma primary tumor site in the oropharynx (includes tonsil, soft palate, base of tongue, walls of oropharynx) and oral cavity that undergo surgery.
- Radiotherapy (in any kind) and/or chemotherapy( Chemotherapy, Docetaxel (Taxotere®), Carboplatin (Platinol ®, Platinol®-AQ), Vinorelbine(Navelbine®), 5-fluorouracil (Adrucil®), Erlotinib (Tarceva), Cetuximab (Erbitux)).
All trials must compare two types of treatment: Combination therapy of radiotherapy and surgery versus the same treatment plus any form of chemotherapy. All trials must have was properly randomized.
Exclusion criteria: All trials with no clinical events registered or available, trials without specific results (with only P value or percentage of registered events)
LITERATURE SEARCH
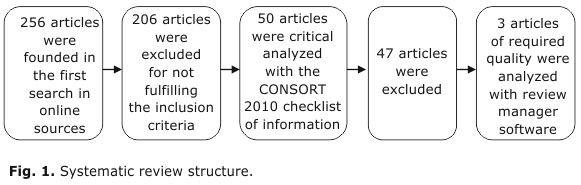
To limit publication bias, data from all published randomized trials evaluating the preceding comparisons were sought using electronic database searching for any randomized trial until 2013 (MEDLINE, Lilacs, Discovery Service (EBSCO), SpringerLink, Wiley - Blackwell Synergy, Cochrane Library and Journal Of Clinical Oncology) hand searching (review articles), and by contacting experts in the field. The search we made with two independent reviewers (Fig. 1). For the intervention, all trials that included a chemotherapy treatment plus the standard treatment and compares it is with a standard one was included. All trials that not fulfill the inclusion criteria we excluded.
50 articles were gathered that included the chemotherapy, radiotherapy and/or surgery treatment as a solution to oral squamous cell carcinoma. All included trials we analyzed with CONSORT 2010 ® checklist of information for a critical analysis of each article (all we checked for methodology quality), leaving all articles that fulfill all requirements to the analyzed with the Review Manager 5.0 ®, the software collects information from each individual study and makes a meta-analysis of data for the systematic review whit meta-analysis. The software Review Manager 5.0 ® performs a statistical analysis of heterogeneity and graphical analysis that enables clinical decision-making
ASSESSMENT OF METHODOLOGICAL QUALITY
Two reviewers assessed all articles that met the selection criteria, methodological quality and factors of the clinical process. Each included investigation they read for the topics: randomization, blinding and bias. It was not possible to blind patient and surgeons. We collected literature by searching in database, with a combination of the following keywords: Carcinoma, Squamous-cell, radiotherapy, chemotherapy and oral cancer
ARTICLE SELECTION AND REVIEW STRATEGY
The selection of studies involved an initial screening of the abstract for to find investigations, which were according to the selection criteria
The low number of randomized controlled studies published limits the reliability of the data. A larger number of investigations they needed to get conclusions. If it was not clear from the methodology in the abstract, the investigation should was rejected.
TYPES OF PARTICIPANTS
Patients with oral squamous cell carcinoma in two types of treatment: one with radiotherapy and surgery alone versus the same treatment plus any form of chemotherapy.
TYPES OF INTERVENTIONS
All interventions that assess the efficacy of radiotherapy and surgery alone versus the same treatment plus any form of chemotherapy in this type of oral cancer.
TYPES OF OUTCOME MEASURES
Evaluate the chemotherapy regimen in patients with oral squamous cell carcinoma comparing it with the standard treatment of radiotherapy alone, specifically in overall survival.
STATISTICAL ANALYSIS
Overall survival was the end of the meta-analysis. The meta-analysis they based on overall survival probabilitiesat the first year estimated from published Kaplan-Meiercurves. The evaluation they made in a fix model, considering that the variability of the studies was from a random origin. Mantel Haenszel they used for the results analysis; this is because this type of method supports studies with fewer samples and few events. Heterogeneity they assessed by the forest plot, the Cochran chi-squared (χ2), and the I2 statistic percentage, considering the values of 25, 50 and 75 % as low, moderate and high heterogeneity.
When I2 is moderate, establishing a sensitivity analysis and assessed the cause of the phenomenon. If it is low, we calculate the number needed to treat (NNT) to estimate the number needed for the analysis.
RESULT
The literature search identified 50 related articles relevant. 47 of these articles were excluded: 12 did not focus on the objective that we study, 15 have poor methodology, 11 have incomplete data for the meta-analysis and 9 articles have inappropriate statistical analysis.
Manual search did not reveal additional articles. The number of studies that fulfill all the inclusion criteria were 3 scientific articles (table), summing up 508 patients in total.
The fixed effect model was chosen for the statistical analysis, assuming that any observed variation in the score was an error of the specific article, with a confidence of 95 % (CI 1.13–2.77), the weight of the investigations are 19.5 %, 53 % and 27 %.8-10
With the selected studies, the meta-analysis was effectuated (Fig. 2) in which all analytic processes that in group derive in the evaluation of heterogeneity of the results, allowing the procedure recommendation. The I2 presents percentage of heterogeneity of 0 %, considering it as non-important heterogeneity of the data in analysis; with a significance of 0.44 (higher than 0.05) in the chi square test, it is proven that the data has no heterogeneity; this implies the low dispersion of the results of the specific studies.11
The plot summary is located in the experimental group (chemotherapy and radiotherapy), establishing the clinical recommendation of use (see the black diamond).
RISK FOR BIAS AND PUBLICATION BIAS
Six items determine the risk of bias for each investigation:
1. Sequence generation
2. Allocation concealment
3. Blinding
4. Missing data
5. Selective outcome reporting
6. Other sources of bias.12
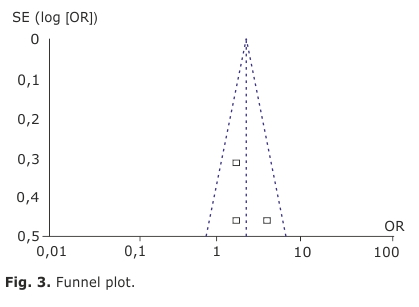
The publication bias they assessed by means of the funnel plot. This graphic displays the relationship between the sample size and the effect size of the investigations.
The funnel plot did not reveal evidence of asymmetry. The Egger test was used to statistical evidence of funnel plot. The results suggested the absence of publication bias (Fig. 3).
DISCUSSION
This type of carcinoma is extremely sensitive to radiotherapy, and it can achieve 5-year survival rates of 75 % or higher, but adding the chemotherapy regimen can significantly increase the 1-year overall survival rates of patients. As for its toxicities, there were an elevated number of them in different grades in some studies. A 107 patients (48 %) experienced grade 3, 4, or 5 toxicity.
There were notably higher incidences of toxicity with chemotherapy than the radiotherapy alone, being the oropharyngealmucositis the most common problem.10
A for other articles, the addition of other type of chemotherapy (one with a low-dose daily regimen) did not cause a significant increase in these radiotherapy induced toxicities, and it caused a significant increase only in high-grade leukopenia, however, the mucositis is one of the most common problems in both arms (42 % in chemotherapy and 49 % in radiotherapy).8
As for the third article, the combined treatment produced toxic effects associated with both chemotherapy and radiotherapy (i.e., hematologic, gastrointestinal, and renal side effects); however, the incidence and severity of mucositis were similar to those observed with radiotherapy alone.9
Being all toxicities foreseen and controlled, it is an important point of discussion with the patients in all the treatment progress, clinical evidence shows some ways, 1 more effective than others.12-14 Some of the studies needed to delay the treatment 1 or 2 weeks for its effects in the patient.
There are other chemotherapy drugs that can improve the quality of life of patients; taken in conjunction with a significant improvement in loco-regional control and overall survival compared with radiotherapy alone. The apparent lack of a negative impact on quality of life of cetuximab combined with radiotherapy is noteworthy, from the clinical point of view as biochemical evidence with a direct impact on the patient.15,16
Although CRT has also demonstrated improved loco-regional control and survival compared with radiotherapy, the effects they achieved at the cost of increased toxicity, including dysphagia and mucosal and hematologic toxicities. In all studies, the overall survival rates of patients in the chemotherapy arm were higher at a 1-year outcome, but over the years of the disease progression, it decreases according to the evidence discussed.17,18
Different scheduling of chemotherapy and radiotherapy has been assessed by many investigators, using different types of chemotherapy drugs or using hyper fractionated radiotherapy.19-22 Aggregate results (as for loco-regional control or distant metastasis free) seem to indicate that concomitant chemotherapy is probably still the most effective way of improving survival outcome.
RECOMMENDATION
The usage of chemotherapy treatment in combination of radiotherapy regimen is highly recommended as for its promising results. Not also, the overall survival has improved, profession free survival and distant metastasis free rates improve, however, more research they needed for a methodologically more powerful conclusion.
As for all toxicities, most of them are foreseen and controlled, but still a main problem in the combination of treatments; being a long term treatment for all patients, their quality of life should always be evaluated. With all the new technology advances and the different types of chemotherapy drugs that have appeared in the last decade, it is highly recommended to keep investigating and evaluating the efficacy of this combination as for the quality of life of the patients.
BIBLIOGRAPHIC REFERENCES
1. Sapp J, Eversole L, Wysocki G. Patología oral y maxilofacial contemporánea. 2° edicion. España: Elsevier; 2005.
2. Huang S, O'Sullivan B. Oral cancer: Current role of radiotherapy and chemotherapy. Med Oral Patol Oral Cir Bucal. 2013;18(2):233-40.
3. Inohara H, Takenaka Y, Yoshii T, Nakahara S, Yamamoto Y, Tomiyama Y, Seo Y, Isohashi F, Suzuki O, Yoshioka Y, Sumida I, Ogawa K. Phase 2 study of docetaxel, cisplatin, and concurrent radiation for technically resectable stage III-IV. Squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2015;91(5):934-41.
4. Chagas F, Silva B, micrographic surgery: a study of 83 cases. Anais Brasileiros de Dermatologia. 2012;87(2):228-34.
5. Smee R, Broadley K, Bridger G, Williams J. Floor of mouth carcinoma: Surgery still the dominant mode of treatment. Journal of Medical Imaging and Radiation Oncology. 2012;56(3):338-46.
6. White S, Pharoah M. Radiologia oral, principios e interpretación. 4° ed. Editorial Harcourt; 2001.
7. Kovács A, Turowski B. Multimodality Treatment Including Postoperative Radiation and Concurrent Chemotherapy with Weekly Docetaxel is Feasible and Effective in Patients with Oral and Oropharyngeal Cancer. Strahlenther Onkol. 2005;181:26-34.
8. Jeremic B, Shibamoto Y, Milicic B, Nikolic N, Dagovic A, Aleksandrovic J, Vaskovic Z, Tadic L. Hyperfractionated Radiation Therapy With or Without Concurrent Low-Dose Daily Cisplatin in Locally Advanced Squamous Cell Carcinoma of the Head and Neck: A Prospective Randomized Trial. J Clin Oncol. 2000;18(7):1458-64.
9. Merlano, M. Benasso M, Corvò R, Rosso R, Vitale V, Blengio F, Numico G, Margarino G, Bonelli L, Santi L. Five-Year Update of a Randomized Trial of Alternating Radiotherapy and Chemotherapy Compared With Radiotherapy Alone in Treatment of Unresectable Squamous Cell Carcinoma of the Head and Neck. J Natl Cancer Inst. 1996;88(9):583.
10. Wee J, Tan E, Tai B. Randomized Trial of Radiotherapy Versus Concurrent Chemoradiotherapy Followed by Adjuvant Chemotherapy in Patients With American JoiInternational Union Against Cancer Stage III and IV Nasopharyngeal Cancer of the Endemic Variety. J Clin Oncol. 2005;23:6730-8.
11. Altman D, Higgins J, Thompson S, Deeks J. Measuring inconsistency in metanalysis. BMJ. 2003;327(7414):557-60.
12. Higgins J, Green S. The Cochrane Library Volume 4. Chichester, UK: Cochrane Handbook for Systematic Reviews of Interventions; 2006.
13. Curran D, Giralt J, Harari P, Kian K, Roger B. Quality of Life in Head and Neck Cancer Patients After Treatment With High-Dose Radiotherapy Alone or in Combination With Cetuximab. J Clin Oncol. 2007;25:2191-7.
14. Nair V, Maeda L, Loannidis J. Clinical outcome prediction by microRNAs in human cancer: a systematic review. Natl Cancer Inst. 2012;104(7):528-40.
15. Li M, Ma X, Li M, Zhang B, Huang J, Liu L, Wei Y. Prognostic role of microRNA-210 in various carcinomas: a systematic review and meta-analysis. Dis Markers 2014;12(123):106-97.
16. Babji D, Kale A, Hallikerimath S, Kotrashetti V. Histomorphometric study to compare histological changes between oral squamous cell carcinoma and apparently normal adjacent oral mucosa. Indian J Otolaryngol Head Neck Surg. 2015;67(1):21-8.
17. Santos M, Servato J, Cardoso S, de Faria P, Eisenberg A, Dias F, Loyola A. Squamous cell carcinoma at maxillary sinus: clinicopathologic data in a single Brazilian institution with review of literature. Int J Clin. 2014;7(12):8823-32.
18. Akhlaghi F, Esmaeelinejad M, Shams A, Augend A. Evaluation of neo-adjuvant, concurrent and adjuvant chemotherapy in the treatment of head and neck squamous cell carcinoma: a meta-analysis. J Dent (Tehran). 2014;11(3):290-301.
19. Soares J, Cançado H, Sousa A, Moraes G, Carvalho J, Silva G, Porcaro-Salles J. Prognostic factors for surgically resected squamous cell carcinoma of the lower oral cavity. Minerva Stomatol. 2014;63(10):341-9.
20. Budach V, Stromberger C, Poettgen C, Baumann M, Budach W, Grabenbauer G, Marnitz S, Olze H, Wernecke K, Ghadjar P. Hyperfractionated accelerated radiation therapy (HART) of 70.6 Gy with concurrent 5-FU/Mitomycin C is superior to HART of 77.6 Gy alone in locally advanced head and neck cancer: long-term results of the ARO 95-06 randomized phase III trial. Int J Radiat Oncol Biol Phys. 2015;91(5):916-24.
21. Katsaounis P, Kotsakis A, Agelaki S, Kontopodis E, Agelidou A, Kentepozidis N, Vamvakas L, Christopoulou A, Karachaliou N, Hatzidaki D, Georgoulias V. Cisplatin in combination with metronomic vinorelbine as front-line treatment in advanced non-small cell lung cancer: a multicenter phase II study of the Hellenic Oncology Research Group (HORG). Cancer Chemother Pharmacol. 2015;75(4):821-7.
22. Shenouda G, Zhang Q, Ang KK, Machtay M, Parliament MB, et al. Long-term results of radiation therapy oncology group 9903: a randomized phase 3 trial to assess the effect of erythropoietin on local-regional control in anemic patients treated with radiation therapy for squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys. 2015;91(5):907-15.
Recibido: 21 de octubre de 2013.
Aprobado: 26 de junio de 2015.
Jaime Irisarri Arévalo. Facultad de Ciencias de la Salud, Universidad del Desarrollo. Concepción, Chile. Barros Arana 1734, Fono: 041-2268544.
Correo electrónico: jaime.irisarri@gmail.com; patricioolivamella@gmail.com