Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Cubana de Estomatología
versión On-line ISSN 1561-297X
Rev Cubana Estomatol vol.54 no.2 Ciudad de La Habana abr.-jun. 2017
PRESENTACIÓN DE CASO
Oral Burkitt's lymphoma associated with human immunodeficiency virus
Linfoma de Burkitt oral asociado con el virus de inmunodeficiencia humana
Rafaela Maia Cardoso Almendra,I Graziele Beanes da Silva Santos,I Natália Nascimento Odilon,I Leonardo Francisco Provedel de Sousa,I Viviane Almeida Sarmento, I Luiza Cavalcanti Fadul,II Luciano Espinheira Fonseca JuniorII
I Department of Dentistry. "Professor Edgard Santos" Hospital, Federal University of Bahia-UFBA, Salvador, BA, Brazil.
II Department of Anatomic Pathology. "Professor Edgard Santos" Hospital, Federal University of Bahia, BA, Brazil.
ABSTRACT
Introduction: Burkitt's lymphoma is an aggressive form of B cell lymphoma generally diagnosed in children and young adults. This tumor has three variants: African (endemic), American (sporadic), and immunodeficiency-associated.
Objective: present a case of Burkitt's lymphoma that manifested as a tumor mass in the upper right maxillary region of a patient with AIDS treated at Professor Edgar Santos University Hospital in Salvador, Bahia, Brazil.
Clinical case: a male 20-year-old HIV-positive patient was referred from another hospital with a possible odontogenic infection that persisted after drainage and antibiotic therapy. The patient presented a tumor growth in the upper right gingival mucosa. After biopsy, histopathological findings were suggestive of Burkitt's lymphoma. An immunohistochemical panel was positive for CD20 and Bcl6 and negative for CD3, Bcl2, and terminal deoxynucleotidyl transferase antibodies. The Ki67 expression level was 80 %. The final diagnosis was immunodeficiency-associated Burkitt's lymphoma. The patient was successfully treated with cytoreductive chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisone), followed by high-dose methotrexate, cyclophosphamide, doxorubicin and vincristine, alternating with high-dose cytarabine, ifosfamide and etoposide. No signs of recurrence have been noted during the follow-up period.
Conclusions: Burkitt's lymphoma is an aggressive neoplasia with a rapidly progressing clinical course. Therefore, differential diagnosis from other benign oral diseases is of great importance.
Keywords: Burkitt's lymphoma; mouth neoplasms; HIV.
RESUMEN
Introducción: el linfoma de Burkitt es una forma agresiva de linfoma de células B generalmente diagnosticado en niños y adultos jóvenes. El tumor tiene tres variantes: africana (endémica), americana (esporádica) y asociada con la inmunodeficiencia.
Objetivo: presentar un caso de linfoma de Burkitt que se manifestó como una masa tumoral en la región maxilar superior derecha en un paciente con SIDA tratado en el Hospital Universitario Profesor Edgard Santos en Salvador, Bahia, Brasil.
Caso clínico: un hombre VIH-positivo de 20 años de edad fue remitido de otro hospital con una posible infección odontogénica que persistió después del drenaje y tratamiento antibiótico. El paciente presentaba un abultamiento tumoral en la mucosa gingival superior derecha. Después de la biopsia, los resultados histopatológicos sugirieron la presencia de linfoma de Burkitt. Un panel inmunohistoquímico fue positivo para CD20 y Bcl6, y negativo para CD3, Bcl2 y para anticuerpos contra la desoxinucleotidil transferasa terminal. El nivel de expresión del Ki67 fue de 80 %. El diagnóstico final fue linfoma de Burkitt asociado a la inmunodeficiencia. El paciente fue tratado con éxito con quimioterapia citorreductiva (ciclofosfamida, doxorrubicina, vincristina y prednisona), seguida de ciclofosfamida, doxorrubicina, vincristina y metotrexato en altas dosis, alternando con ifosfamida, etopósido y citarabina en altas dosis. No se observaron señales de recurrencia durante el período de seguimiento.
Conclusiones: el linfoma de Burkitt es una neoplasia agresiva con rápida evolución clínica. Por lo tanto, el diagnóstico diferencial de otras enfermedades bucales benignas es de gran importancia.
Palabras clave: linfoma de Burkitt; neoplasias de la boca; VIH.
INTRODUCTION
Burkitt's lymphoma (BL) is a malignant tumor derived from B lymphocytes that is generally diagnosed in children and young adults. The three clinical variants of Burkitt's lymphoma, described by the World Health Organization (WHO), are endemic, sporadic and immunodeficiency-associated types.1-9 These types are similar in morphology, immunophenotype, and genetic features.3
The endemic, or African, variant is considered a pediatric disease and is frequently associated with exposure to the Epstein-Barr virus (EBV).2,5-8 The immunodeficiency-associated variant is typically observed in patients who have acquired immunodeficiency syndrome (AIDS).2-4 BL is the second most common form of AIDS-associated lymphoma.10
BL is a rare tumor subtype, although it represents approximately 40 % of HIV-associated lymphomas.1,4-5 The mouth is an unusual site for extranodal lymphoid tissue neoplasms; however, individuals with AIDS more commonly present with oral lymphomas than do immunocompetent individuals.11
Considering the gravity of these lesions and the importance of early diagnosis and treatment, the objective of this study is to report a case of BL that manifested as a tumor mass in the upper right maxillary region in a patient with AIDS treated at the Professor Edgar Santos Hospital in Salvador, Bahia, Brazil.
PRESENTATION OF CASE
This case report was approved by the Ethics Committee of Professor Edgar Santos Hospital, Federal University of Bahia and the patient signed the consent form to the disclosure of history and images (Nº 796.365).
A 20-year-old HIV-positive man who was not treated with antiretroviral therapy (ART) prior to admission was admitted to the Professor Edgar Santos Hospital (Bahia, Brazil) with a growth on the face, suspected to be an abscess, that persisted after the use of amoxicillin, potassium clavulanate, cefazolin, cephalothin, and metronidazole. The patient reported undergoing a recent tooth extraction with mobility in the affected area.
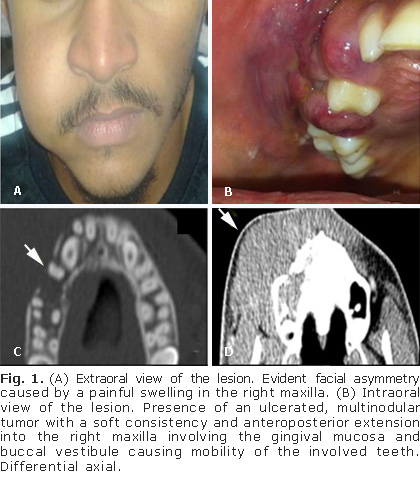
At Professor Edgar Santos Hospital, ceftriaxone and clindamycin were introduced. A physical exam showed painless volume increase of the middle third of the right side of the face (Fig. 1, A) corresponding to a tumor in the superior right gingival mucosa that was erythematous, purplish in color, and of a soft consistency upon palpation, measured approximately 6.7 × 5.7 × 4.4 cm, and was associated with mobility of the teeth of the right jaw (Fig. 1, B). Tomographic slices performed before treatment show images to bone tissue (Fig. 1, C) and soft tissue (Fig. 1, D).
He presented with a lymphocyte count of CD4+ T cells equal to 596 cells/µL and a viral load of 299,307 copies/mL and was started on lamivudine, tenofovir, and efavirenz-based ART.
The patient developed abdominal pain in the left upper quadrant, jaundice, and had increased levels of canalicular enzymes. An abdominal ultrasound showed obstruction of the biliary tract characterized as an extrahepatic cholestasis.
Contrast computed tomography (CT) of the face showed an expansive formation with soft tissue density and ill-defined borders in the right oral fascial space with infiltration of the muscle and adipose tissue that extended to the alveolar process of the maxilla, maxillary sinus, and inferior meatus of the ipsilateral nasal cavity.
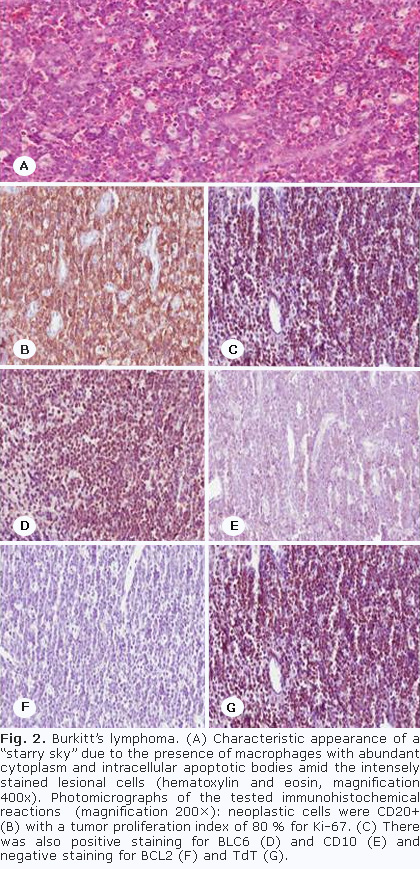
A fine needle aspiration biopsy (FNAB) of the buccinator muscle region revealed that 90% of the cells (CD45++/+++) of the lymphoid B lineage (CD 19+++, CD22+/++ and CD20++/++) co-expressed Calla antigens (CD10++/+++) and lymphoid T cells (CD5+/-). The cells also presented clonality for the light-chain kappa +/++. CD3 and CD23 T lymphoid antigens were negative. FNAB data suggested the possibility of B cell lymphomas derived from the germinal center, known as BL. An incisional biopsy of the superior right gingival mucosa region was performed to confirm these findings. The subsequent histopathological analysis revealed mucosal fragments that were partially coated by well-differentiated squamous epithelial cells whose underlying tissue showed extensive infiltration of lymphoid lineage cells with moderately pleomorphic and hyperchromatic nuclei with little broad and optically clear cytoplasm in addition to the numerous macrophages that phagocytose cellular debris of apoptotic tumor cells, which created the standard morphological appearance of a "starry sky" (Fig. 2, A).
An immunohistochemical panel of CD3, CD20, Ki67, TdT, Bcl2, and Bcl6 antibodies was positive for CD20 and Bcl6 and negative for CD3, Bcl2, and TdT antibodies. The Ki-67 expression rate was 80 %. The histopathological and immunohistochemical exams and immunophenotyping findings led to the diagnosis of immunodeficiency-associated BL (Fig. 2, B-G).
The patient underwent methylprednisolone pulse therapy for a total of 3 days with the objective of quickly curtailing disease progression. Standard ART was temporarily suspended at this time. The patient began chemotherapy with the cytoreductive therapeutic regimen of cyclophosphamide, vincristine, and prednisone followed by the cyclophosphamide, doxorubicin, vincristine, and high-dose methotrexate (CODOX-M) for a total of 38 days alternating with the ifosfamide, etoposide, and high-dose cytarabine (IVAC) regimen for 21 days.
While being treated with the CODOX-M regimen, the patient presented with febrile neutropenia and was given Tazocin® for 7 days. During the IVAC regimen, he developed severe thrombocytopenia requiring a platelet transfusion. During chemotherapy, he developed grade III mucositis and lock-jaw. Palliative therapies to alleviate painful symptoms were instated, such as oral analgesics and 2.0 % lidocaine mouthwash before meals.
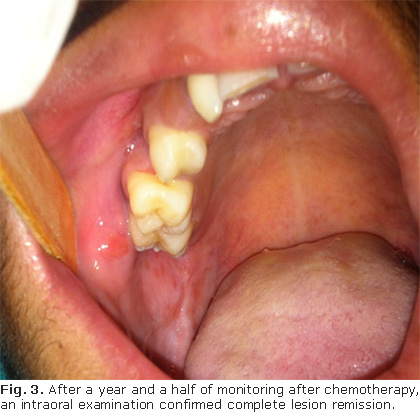
The oral tumor began to regress after four cycles of chemotherapy (Fig. 3). The patient was discharged in good clinical condition and was hemodynamically stable and afebrile. The cholestasis was resolved and the ART was reintroduced. The patient presented with an LT CD4 of 385 cells/µL and a viral load of 358 copies/mL. CT restaging performed after 6 months showed lesion regression in the soft tissues. The patient has been under observation for 12 months with no signs of tumor recurrence or opportunistic infections. He regularly uses ART and has a viral load of 40 copies/mL and a lymphocyte count of CD4+ T cells equal to 345 cells/µL.
DISCUSSION
BL is a rare and rapidly progressing tumor that is responsible for 40% of all HIV-associated lymphomas.1,5 According to Fukunaga et al.,10 HIV-positive patients are at approximately 100× greater risk of developing lymphoma than immunocompetent individuals.
According to Balasubramaniam et al.2 e Rebelo-Pontes et al.6 immunodeficiency-associated BL is a variant that rarely develops in the oral cavity. BL has no specific clinical symptoms, and it is often misdiagnosed as odontogenic infections.2,9 The signs and symptoms of oral BL include tooth mobility, which are associated with the lesion, gingival enlargement, and bone cortical expansion.1,2,5,8 Gingival swelling or rapidly growing tumor masses in the oral cavity are regarded as the most common initial symptom.9 In the present case, the patient presented with an erythematous, purplish, and ulcerated legion that caused facial asymmetry, hard palate bulging, and mobility of the teeth adjacent to the tumor.
When the symptoms of BL develop in the oral cavity as a tumor mass resulting in facial asymmetry such as in the present case, the lesion is often clinically misdiagnosed as a dentoalveolar infection. This infection usually responds well to antibiotics, whereas oncologic infections do not.9 Our patient used several different antibiotics and underwent multiple drainage procedures in the region without clinical improvement.
HIV testing should be requested for patients with oral lesions for whom there is a clinical suspicion of BL.2 Our patient already had an AIDS diagnosis prior to hospitalization; therefore, new exams were performed for CD4+ T lymphocyte counts and viral load to determine the immunosuppression degree.
AIDS-associated BL presents many characteristics that differentiate it from other forms of lymphoma. BL is recognized histologically as having intermediate-sized, monomorphic, noncleaved cells imparted with numerous macrophages appearing as a "starry sky pattern".12 Histologically, it exhibits diffuse epithelial growth and cellular pleomorphism and is derived from B lymphocytes. It also commonly presents with a high level of mitotic figures and the tendency to produce necrosis. These characteristics imply a high cell proliferation rate and rapid growth rate, which are accompanied by an aggressive clinical course and poor prognosis.13
The histological findings from routine staining are suggestive but not conclusive of BL, necessitating an immunohistochemical study. The tumor cells expressed membrane immunoglobulin M with light chain restriction and antigens associated with CD19, CD20, CD22, CD10, and Bcl-6 B cells. The cells are negative for CD5, CD23, and TdT, and Bcl-2 is not expressed,5,7,14 corroborating the findings of this case. The Bcl-6 expression favors the origin of the germinal center. It is also possible to detect marked Ki-67 positivity, demonstrating high-grade tumor proliferation. Considering that this fraction of proliferation is almost 100 %, tumor doubling time is very short (approximately 24 hours).1,3,8 In the present case, the marking by Ki-67 indicated a cell proliferation index of 80 %.
In the BL immunophenotype, a negative response is observed in the terminal deoxynucleotidyl transferase (TdT), an enzyme involved in the cellular repair pathway.2,13 This result is in accordance with the immunohistochemical findings of this report. The TdT study is opportune for the histological differential diagnosis of BL from lymphoblastic leukemia since its findings are generally negative for the former and positive for the latter.2
BL presents important biological characteristics, since it was one of the first human tumors to be consistently associated with a viral infection, to present a chromosomal translocation that activates an oncogene (c-MYC) and to be correlated with human immunodeficiency virus (HIV) infection.3 The molecular alterations characteristic of immunosuppression-associated BL are associated with an immunosuppression focus on the presence of a translocation involving the c-MYC oncogene, which has an essential role in cell cycle control.3,13
Despite its aggressive behavior, BL is very chemosensitive and, several intensive multiagent chemotherapeutic programs have resulted in excellent long-term remission rates and long-term survival.7 The prognosis for patients with AIDS-associated has improved significantly due to the administration of high-intensity combination chemotherapy including the CODOX-M/IVAC regime consisting of cyclophosphamide, doxorubicin, vincristine, high-dose methotrexate alternating with ifosfamide, etoposide and high-dose cytarabine, the same course we used here.7,10,12
In addition to drug therapy, prognosis varies with the disease extent, patient age, time since diagnosis, and gravity of the comorbid diseases. The prognosis is excellent for children, approaching 100 % disease-free survival rates in the early stages, while 75-85 % of patients survive disease-free into adulthood. In contrast, adults are almost always HIV-positive patients and may die of other causes.1,13
BL is an aggressive neoplasia with a rapidly progressing clinical course. Therefore, the differential diagnosis from other benign oral diseases is of great importance. BL-underlying tumor lesions in immunocompromised patients should be suspected and the definitive diagnosis should be made by pathological examination complemented by an immunohistochemical study.
Conflict s of interests
The authors declare no conflicts of interests.
BIBLIOGRAPHIC REFERENCES
1. Jan A, Vora K, Sándor GKB. Sporadic Burkitt's Lymphoma of the Jaws: The Essentials of Prompt Life-saving Referral and Management. J Can Dent Assoc. 2005 Mar;71(3):165-8.
2. Balasubramaniam R, Goradia A, Turner LN, Stoopler ET, Alawi F, Frank DM, et al. Burkitt lymphoma of the oral cavity: an atypical presentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Feb;107(2):240-5.
3. Molyneux EM, Rochford R, Griffin B, Newton R, Jackson G, Menon G, et al. Burkitt's lymphoma. Lancet. 2012 Mar 31;379(9822):1234-44.
4. Komatsu N, Kawase-Koga Y, Mori Y, Kamikubo Y, Kurokawa M, Takato T. HIV-associated Burkitt lymphoma in a Japanese patient with early submandibular swelling. BMC Res Notes. 2013 Dec 26;6:557.
5. Pinisetti S, Nalabolu GRK, UVR C, Tadi DP. HIV Associated Intra-oral Burkitt's Lymphoma: A Case Report. J Clin Diagn Res. 2013 Dec;7(12):3088-9.
6. Rebelo-Pontes HA, Abreu MC, Guimarães DM, Fonseca FP, Andrade BAB, Almeida OP, et al. Burkitt's lymphoma of the jaws in the Amazon region of Brazil. Med Oral Patol Oral Cir Bucal. 2014 Jan 1;19(1):e32-8.
7. Casulo C, Friedberg J. Treating Burkitt Lymphoma in Adults. Curr Hematol Malig Rep. 2015 Sep;10(3):266-71.
8. Patankar S, Venkatraman P, Sridharan G, Kane S. Burkitt's lymphoma of maxillary gingiva: A case report. World J Clin Cases. 2015 Dec 16;3(12):1011-6.
9. Kılınç A, Saruhan N, Tepecik T, Gündoğdu B. Burkitt's Lymphoma Presenting as Maxillary Swelling: Case Report. MBSJHS. 2016;2(2):29-32.
10. Fukunaga A, Yoshiro I, Shojiro I, Sueki Y, Yoshinaga N, Yanagida S, et al. Immune reconstitution inflammatory syndrome mimics a relapse of AIDS-related Burkitt lymphoma. Intern Med. 2013;52(19):2265-9.
11. Goto M, Onizawa K, Yanagawa T, Yamagata K, Shinozuka K, Nishikii H, et al. Human immunodeficiency virus-associated Burkitt's lymphoma in oral cavity of Japanese patient. J Oral Maxillofac Surg. 2012 Aug;70(8):1885-90.
12. Johnson DH, Reske T, Ruiz M. Case Report and Review of Immunodeficiency-Associated Burkitt Lymphoma. Clin Lymphoma Myeloma Leuk. 2015 Jun;15(6):e121-5.
13. Carbone A. AIDS-related non-Hodgkin's lymphomas: from pathology and molecular pathogenesis to treatment. Hum Pathol. 2002 Apr;33(4):392-404.
14. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4 th ed. Lyon: IARC Press; 2008. p. 260-1.
Recibido: 5 de septiembre de 2016.
Aprobado: 20 de abril de 2017.
Rafaela Maia Cardoso Almendra . Department of Dentistry. Rua Augusto Viana, s/nº, Canela, Professor Edgard Santos Hospital, Federal University of Bahia-UFBA, Salvador, BA, Brazil. . E-mail: rafaelaalmendra@gmail.com