Introduction
First described by Stoneman and Worth in 1983, mandibular buccal bifurcation cyst (MBBC) is a rare case of inflammatory odontogenic cyst that develops predominantly on the buccal surface of the permanent mandibular first molar or, occasionally, on the second mandibular molar in children aged 6 to 15 years old.1,2,3
In 1992, the World Health Organization (WHO) included this lesion into the category of paradental cyst and named it “mandibular infected buccal cyst”.4 As early as 2005, this pathological entity was listed into the category of “inflammatory cysts”5) due to four major clinical features in the involved tooth: altered tooth eruption, lingual inclination of the root tips, increased probing depth on the buccal surfaces (>3mm) and positive pulpal sensitivity.4
After 2017, according to the new classification of odontogenic cysts and tumors by the WHO, this lesion was eventually named MBBC and was listed into the category of inflammatory collateral cysts, together with the paradental cyst, as they are found buccal to the roots of partially or newly erupted teeth.6
The pathogenesis of MBBC remains uncertain; however, it is believed that an inflammatory response may occur around the follicular tissue concomitantly with dental eruption, stimulating cyst formation. Additionally, this cyst may cause pain or sensitivity to palpation or percussion as well as local abscess.7
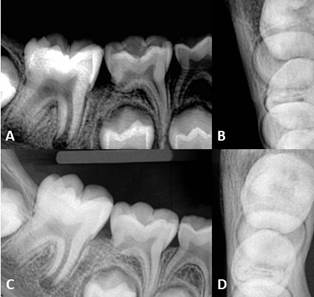
Radiographically, MBBC is characterized by a well-circumscribed unilocular radiolucent area in the buccal furcation area, with intact periodontal ligament space and lamina dura. An occlusal radiograph may be useful to demonstrate the cyst, and reports indicate that one-third of the individuals have bilateral involvement of the first molars.2,8
The histopathological aspects of the MBBC are not specific: it is lined with non-keratinized stratified squamous epithelium with areas of hyperplasia.5 This lining may be adhered to the cementum-enamel junction or along the epithelium of the pericoronal tissues, forming an invagination or pocket that is projected buccally to the dental root.1 Therefore, the diagnosis of this lesion is obtained from its clinical and imaging characteristics.1,3,6
The treatment usually includes cystic enucleation, without extraction of the involved tooth.2 There are also other therapeutic procedures such as enucleation with extraction and non-surgical treatment (micro-marsupialization).2 This consists of the daily irrigation of the buccal pocket with saline solution and/or hydrogen peroxide.1,2,7,8 Few publications have reported cases with no need for intervention.7,9,10,11
Given the rarity of this cyst and the controversy around its treatment, the aim of the current paper is to report a case of spontaneous involution of a unilateral mandibular buccal bifurcation cyst.
The study was approved by the Research Ethics Committee of the Professor Edgard Santos Hospital, Federal University of Bahia (CAAE: 27139614.9.0000.0049).
Case presentation
A 6-year-old girl was referred to the Pediatric Department at Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador, Bahia, Brazil. The patient was admitted with fever and productive cough due to bacterial pneumonia. During hospitalization, the patient was examined by the dental team and reported discomfort in the right lower dental arch. Extraoral examination revealed no remarkable changes (Fig. 1, A). In the intraoral exam, the permanent lower right first molar (tooth #46), partially erupted, did not show any carious lesions (Fig. 1, B). Notably, the mandibular buccal surface was slightly increased in volume and hardened on palpation. The pulp sensitivity test was positive and the probing depth was approximately 4.5 mm in the buccal aspect of the involved tooth (Fig. 1, C).
After the clinical examination, we performed imaging examinations to improve diagnostic elucidation. The periapical radiograph showed discrete radiolucency involving the bifurcation area of tooth #46 (Fig. 1, D).
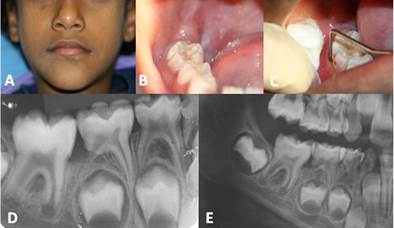
Fig. 1 Clinical presentation of the MBBC: (A) Clinical photograph of the face in which there is no alteration of volume in the affected region. (B) Intraoral aspect showing tooth #46 (C) Periodontal probing demonstrating a probing depth at mid-buccal site of approximately 4.5 mm. Radiographic views: (D) Periapical radiograph of the lower right molar region showing radiolucent area in the furcation region of the involved tooth. (E) Partial view of the panoramic radiograph showing circular radiolucent area superimposed on the furcation region of tooth #46.
The panoramic radiograph also showed a well-defined radiolucent area on the buccal surface of the involved tooth (Fig. 1, E). On the multislice computed tomography (Fig. 2, A-F) with 3D reconstruction (Fig. 2, G), we observed a hypodense unilocular and well-circumscribed image on the buccal surface of tooth #46, with perforation of the buccal cortical bone.

Fig. 2 Multislice computed tomographic evaluation: (A and B) Axial section. (C) Coronal section. (D) Panoramic reconstruction. (E and F) Cross section. (G) Three-dimensional reconstruction of the mandible showing a hypodense area with well-defined limits in the buccal bone of tooth #46, with discrete bulging and solution of continuity in the cortical bone.
The association of the clinical and imaging findings led to the diagnosis of MBBC, opting for cystic enucleation without extraction. About 45 days after the first evaluation, the patient returned to perform the surgical procedure. However, during this consultation, a reduction of the lesion could be observed, possibly indicating spontaneous involution of the lesion. Thus, considering the new findings, the procedure adopted included clinical and radiographic follow-up.
In the first re-evaluation, three months after the first consultation, the lesion already showed signs of clinical and radiographic involution: periodontal probing depth of 3 mm at the buccal site and reduced radiolucent area (Fig. 3, A and B). The involved tooth was responding to the pulp sensitivity test, an indication of vital pulp.
The patient returned to follow-up examination approximately 1 year after the first consultation, when no evidence of residual lesion was found, with complete bone regeneration (Fig. 3, C and D) as well as a normal eruption pattern of the involved tooth, without any signs of recurrence.
Discussion
This is a case report about the diagnosis and spontaneous involution of a unilateral MBBC. In agreement with the literature,1,2,12 this case presents some typical clinical features: site-specific lesion with predominance in the first decade of life, increased volume in the affected area and lingual root inclination.
Treatment for MBBC is controversial in the literature. The two major treatment approaches described are: enucleation of MBBC with dental extraction and curettage of the lesion,8 or enucleation and curettage without extraction of the involved tooth.(1,2, 3,7,8,12) However, a more conservative approach has been described by David et al.9, with a non-surgical resolution, by periodontal probing and/or daily irrigation of the buccal pocket with saline solution. This technique aims to induce a small rupture in the cyst (“micro-marsupialization”), allowing depressurizing and spontaneous cure. These authors reported treatment of 5 MBBCs in 3 patients with bilateral MBBCs with up to 15 months of follow-up, with only one lesion surgically removed (enucleation without extraction).
Additionally, David et al.9 described another conservative approach, which basically consisted of follow-up, and proposed that MBBC could be self-limiting. They also speculated that the microtrauma and subsequent inflammation of the buccal gingival tissues and the lining of the cyst might induce a slight rupture of the lesion, defined as “automarsupialization” and “self-resolution”. This may explain the spontaneous involution described in the present report. Another hypothesis is that spontaneous involution of MBBC can be explained by the fact that patients in the pediatric age group have faster healing and bone remodeling capacity, which is justified by the excellent blood supply and the continuous process of growth.13 However, to date there is still no reliable evidence in the scientific literature explaining its self-resolution.
More recent publications, such as the studies conducted by Corona-Rodriguez et al.11 and Zadik et al.7, reported spontaneous involution of cases of bilateral MBBCs. In these studies, the left lesion was surgically enucleated and the right lesion was only followed up, with radiographic involution observed at 3 and 6 months, respectively. In our report, we observed bone repair with radiographic evidence of cyst involution. There was no recurrence during the follow-up period. All teeth remained vital and erupted normally.
Here, the self-resolution of the case can be assured by the involution of the cystic area confirmed by radiographic examinations, associated with the remission of clinical signs and symptoms.
Considering that the histopathological features are non-specific and are microscopically similar to other inflammatory odontogenic cysts such as the radicular cyst,1,12) the diagnosis is made through clinical findings and radiographic features. The pathogenesis of MBBC is only hypothetical. In this report, the radiographic evidence associated with the clinical characteristics confirmed the diagnosis and, consequently, the choice of a conservative treatment.
The diagnosis of MBBC is unanimously agreed upon in the literature and is based on clinical and imaging evaluation. However, there is controversy around its treatment. More conservative therapeutic options should be considered, given that more invasive surgical procedures can be traumatic among pediatric patients, because of their magnitude, duration of operation,14 potential aesthetic and functional damages, as well as possible psychological/behavioral consequences.15,16
Based on the findings of this report and the available literature, we recommend that conservative and minimally invasive procedures should be considered as a therapeutic option in cases of small-sized MBBCs.
Conclusions
Knowledge of MBBC's clinical and radiographic characteristics is essential for the differentiation of other inflammatory cysts and, consequently, for proper management. The possibility of spontaneous involution is a characteristic that must always be observed, in order to avoid unnecessary surgical procedures.