INTRODUCTION
Rabies is a zoonotic disease, and it spreads in many countries around the world and causes economic burdens, especially in developing countries. Rabies is fatal to humans, however, can be controlled and eliminated. According to World Health Organization (WHO), World Organization for Animal Health (OIE), and Food and Agriculture Organization (FAO), rabies is a disease that can be controlled and prevented by vaccination.1 According to WHO, every year, about 59 000 people get rabies in more than 150 countries, of which 95 % occurs in Asia and Africa.1 Dogs are the primary reservoir of the rabies virus in Southeast Asia in humans through bites and/or scratches.2,3 People usually get rabies from the bite of a rabid animal. It is also possible, but rare, for people to get rabies directly from open wounds.4,5,6 In Vietnam, most rabies deaths are caused by dog bites, so vaccine coverage in the total dog population plays an important role in reducing the number of death cases.
According to data reported by provinces and cities in 2015, the country had 9 million dogs, but the number of dogs vaccinated against rabies was 3.89 million, accounting for 42.9 %.7 Mountainous and rural areas in Vietnam saw a low vaccination coverage in dogs due to a lack of knowledge on disease prevention and low income. In addition, free-range animal husbandry increases the risk of rabies transmission for dogs and other animals. As a result, rabies continues to become a threat to humans.
People who are bitten by animals identified as at risk for rabies should receive post-exposure prophylaxis.8 WHO recommends that people bitten by an animal should wash the wound immediately with soap and warm water or with an antiseptic, followed by simultaneous injection of rabies vaccine and human rabies immune globulin (RIG), and complete the recommended vaccination schedule.9 The first dose of the rabies vaccine and rabies immune globulin should be administered at the same time, because RIG can inhibit the entry of the virus to the nervous system. RIG is administered as a passive immune treatment in order to provide immediate access to rabies-virus neutralizing antibodies until the patient's immune system can begin to produce its own neutralizing antibody after vaccination.10 It is therefore important for the public to understand the role of post-exposure prophylaxis in reducing the risk of death from rabies in humans.
The objective of this research is to evaluate knowledge, attitudes and practices towards rabies prevention and factors related to vaccines for both, patients exposed with rabies and dogs.
METHODS
Research location
Duc Co district, Gia Lai and Ea Sup district, Dak Lak: areas with lowest vaccination coverage in dogs and a high number of patients with pot-exposure prophylaxis. The research period was from January 2020 to June 2021.
Research design and sample size
The research design is descriptive, cross-sectional, using questionnaires about the knowledge, attitudes, prevention practices and risk of rabies, based on the availability of references from Tran Thi Anh's previous research11 regarding the percentage of good practices in rabies prevention. We chose the rate as 0.595, the level of statistical significance was 0.05, the absolute error of 0.05 and design effect was 2. The calculated sample size was 742. Thus, on average, each province surveyed 742 households, equivalent to 2 provinces, interviewing 1,484 households. Research subjects were representatives of households living in Duc Co district, Gia Lai and Ea Sup district, Dak Lak.
Questionnaire design: it was partly similar to previous studies that have been carried out in Vietnam, and consisted of 4 parts:
Part 1: related to the general characteristics of interviewees.
Part 2: general characteristics of households raising dogs and cats, and people's behavior after being bitten by them.
Part 3: an assessment of knowledge and attitudes related to rabies control.
Part 4: questions related to rabies prevention practices.
Variables studied: general characteristics of interviewees (gender, age groups, ethnics, academic level, occupation, households with dogs/cat); status of households with cats and dogs, and people's actions after a pet bites; knowledge and attitude of people to prevent rabies; practice and prevention of rabies among people, and factors related to vaccines for both patients exposed with rabies and dogs.
Data management and analysis: logistic regression analysis was performed for each outcome variable, and the adjusted odds ratios (AOR), CI (confidence interval) with a 95 % confidence interval were calculated. In addition, multivariable logistic regression was used to determine factors related to vaccination rates for both patients exposed with rabies and dogs. Any variable with p < 0.05 is considered to be statistically significant. SPSS v. 22.0 software was used to detect relationships and compare ratios.
RESULTS
Demographic and social characteristics of the respondents
The Kinh ethnic group participated in the survey the most with 831 people and most of the households participating in the survey own cats and dogs (table 1).
Table 2 shows that the number of victims being bitten by dogs and cats was 361 people, most of which were caused by dogs. A large percentage of people bitten by pets had knowledge about animal bites. More than 68 % of the survey respondents received rabies vaccine and went to a health facility for post-exposure treatment. The percentage of people going to a traditional healer was 7.48 %, doing nothing 18.28 % and taking other actions after exposure 5.54 %. Over 68 % of the respondents said that they let their dogs free or only occasionally kept them in cages.
Among dog-raising households, 60.03 % of them vaccinated against rabies for dogs. The number of households vaccinated against rabies for dogs was more than 5 times higher than that for cats. Among pet-owners, 843 respondents agreed to inject vaccine for their dogs and cats.
There were 1 196 interviewed households raising one or more dogs, showing that the dog density is high, and the rate of rabies vaccination for pets is 60 %. However, there were still many unvaccinated dogs that pose a public health risk in the event of a rabies outbreak.
Knowledge, attitude, practice of rabies prevention among people in the studied areas
Most of the participants identified dogs as subject to rabies, followed by cats with respectively 1 269 and 899 responses. Only 370 respondents understood that humans were the primary target for rabies. 53.43 % knew that vaccines could prevent rabies. Just over a third of respondents knew that rabies was an incurable disease. Still, less than 1/5 of the respondents lacked knowledge about this fatal disease, they answered that it is a treatable disease and only targets dogs and cats.
The results in our study on attitudes related to rabies prevention were mentioned in the last three questions in table 3. Many interviewees (70.62 %) had a positive attitude toward post-exposure prophylaxis. Although 999 respondents had enough knowledge of rabies prevention, the figure for lack of knowledge was 485 people. In contrast, while the number of respondents with a satisfactory level about rabies prevention was 655, the other number was 829.
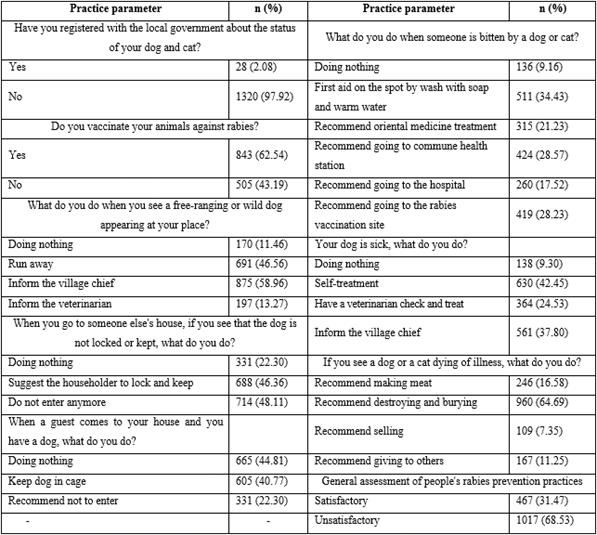
The practices of the interviewees on local rabies prevention and control are shown in table 4. When a dog or cat bites someone, what do you recommend? The correct action was that going to the commune health station and getting vaccinated have nearly equal rates with results of 28.57 % and 28.23 %, respectively. Some people recommended giving first aid on the spot and going to the hospital. There was still a large percentage of inexperienced people with the wrong answer to doing nothing and treating traditional medicine.
When assessing rabies prevention practices, the percentage of households that did not meet the rabies practice was 68.53 %, which almost doubled the number of households with the practice (31.47 %).
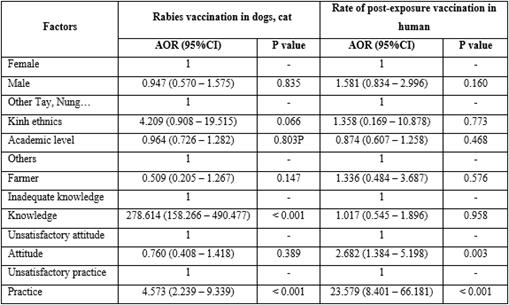
Factors related to the rate of post-exposure vaccination and rabies vaccination in dogs
Table 5 shows the results of multivariable logistic regression analysis. The factor most strongly associated with rabies vaccination rates for pets is ethnicity. The Kinh people had the highest vaccination rate (AOR= 4.209; 95 % CI: 0.908-19.515). The higher the education level, the higher the rabies vaccination rate in dogs, while farmers got the lowest rabies vaccination rate in dogs (AOR= 0.509; 95 % CI: 0.205 - 1.267). Only knowledge and practice met the criteria on rabies prevention, those with good knowledge and practice had a high vaccination rate with AOR and CI AOR = 278.614 (95 % CI: 158.266 - 490.477, p< 0.001) respectively, and AOR = 4.573 (95 % CI: 2.239 - 9.339, p< 0.001).
Another element strongly related to the vaccination rate after being bitten by an animal were gender, with the male having a greater proportion (AOR= 1.581; 95 % CI: 0.834-2.996), followed by Kinh ethnicity (AOR= 1.358); 95 % CI: 0.169 - 10.878). Those with good attitudes and practices have a high post-exposure vaccination rate with AOR and CI respectively AOR = 2.682, (95 % CI: 1.384 - 5.198, p= 0.003) and AOR = 23.579 (95 % CI: 8.401 - 66.181, p < 0.001).
DISCUSSION
In our study, the respondents knew about the host of rabies: 85.51 % and 24,93 % of them answered that dogs and humans are rabies reservoirs and understood that pets and people could transmit this disease. Khadija B12 had slightly larger results than our study.
In our study, 53.43 % of people understood that rabies could be prevented by post-exposure vaccination, Amare B13 had greater results than our study.) When surveying people's knowledge about rabies that can be transmitted to humans and other animals, our results are consistent with the study of Lanada EB et al.14 In our report, 38.74 % of respondents is well-equipped with knowledge that rabies is a dangerous and fatal disease, authors Khadija B12 and Li15 had a much higher result than ours.
In this study, we found that some people were very ignorant about rabies. In China more than 40 % of the participant did not know that rabies is an infectious disease; this result is similar to our study.15 Stray dogs, if positive for the rabies virus, can be transmitted to other animals. Animals that are in contact with humans are at risk of transmitting disease to humans through the bite of an infected animal. Therefore, local authorities need to educate people about rabies to break the rabies transmission cycle. Controlling stray dogs is an important step in breaking the rabies transmission line. Register pets with local authorities is to mobilize dog owners to vaccinate against rabies and monitor vaccine coverage in dogs. Therefore, to break the cycle of disease transmission, it is necessary to educate people about rabies and increase the vaccination rate in domestic animals.
In this study, we found that the attitude related to rabies prevention of the interviewees was not good.
Vaccination rates for dogs in our study were less than previous evidence, they demonstrated that vaccination rates must reach at least 70 % of dogs and continuous vaccination for 3 years to control rabies.8,16 We found a significant association between people's knowledge, attitudes and practices related to rabies prevention. We find that the Gia Rai, Ede and low educated people see much lower vaccination rates for livestock than the Kinh and highly educated people, although this difference is not statistically significant. In addition, with their occupation as farmers, these people have poor knowledge and practice and have very low vaccination rates for livestock. In our study, 37.46 % of households did not vaccinate their pets. These animals may be infected with rabies. Vaccination in dogs is necessary to interrupt the animal-human transmission cycle of rabies. In our study, the low vaccination rate in dogs was due to the fact that people did not know about the village's vaccination plan and the distance from their house to the vaccination site was long. Therefore, provincial preventive health centers should deploy vaccination points near people's houses and health workers and should encourage people to vaccinate their pets.
In fact, the coverage of rabies vaccine in dogs varies widely between provinces and cities in Vietnam, which may be due to the ineffective communication method to raise public awareness about rabies in Vietnam. Specifically, this target is Duc Co district, Gia Lai in 2019 reaching 40 %-50 %, in Ea Sup Dak Lak 10 %-20 %. Low vaccination rates in animals can be attributed to modest household income and high vaccination fees, which lead to low vaccination rates for livestock, even though people understand the benefits of vaccination.
In this study, 34.43 % of the respondents took the correct action. They advised the victim to wash the wound with soap and warm water gently. Failure to wash wounds after exposure has been shown to increase the risk of rabies by 5 times.17 The second correct action, if bitten by a dog or cat is immediately taking the victim to the hospital or getting vaccinated.
Our results clearly show that the Giarai, Ede and people with low education have a much lower rate of post-exposure vaccination than the Kinh and highly educated people. However we found no difference in logistic regression analysis. Similarly, people with poor attitudes and practices had a much lower vaccination rate after being bitten by animals. Out of 361 people who dogs bite, 160 had good practice scores, and 155 people had been vaccinated against rabies, and this is the number of people with high practice scores. Out of the remaining 221 people who a dog bit, they did not reach the practice score, but 93 of them knew how to get vaccinated, proving that they had the right behavior to reduce the incidence of rabies in humans. However, among the interviewees who was bitten by a dog or a cat, still more than 30 % of those bitten by a rabid dog have acted wrongly. Therefore, ethnic minority people, with low education level, and people with inadequate knowledge, attitudes and practices need intervention to raise awareness about rabies prevention and control.
Data from the over-capacity health centers in the two provinces we are studying reported 12 deaths from rabies in 2018 and 13 cases in 2019. This indicates that, the village chief needs to propagate and raise public awareness about the consequences of dog bites and the need for vaccination to reduce the risk of death from rabies in humans. As a result, people can understand that human rabies is completely preventable through post-exposure prophylaxis. Taking victims of rabies bites for vaccination immediately after exposure and vaccinating dogs reached the rate of 70 %.18
Research limits: the sampling method cannot represent the entire Gia Lai and Dak Lak provinces.
In our study, while 999 and 655 respondents had enough knowledge and attitude of rabies prevention, the figure for rabies prevention practice was 467.
People with a high level of education, knowledge and practice, the rabies vaccination rate on pets is high. People with good attitudes and practices had a high rate of rabies vaccination after being bitten by an animal.