Introduction
Nuclear medicine (NM) is a medical practice in which unsealed radioactive substances are used for diagnosis, therapy and clinical research. The major part of this discipline, diagnosis, involves two different approaches: in vivo studies, in which radioactive substances are administered to the patient either the function of an organ or to provide an image of it and in vitro methods, in which body fluids or tissues are analyzed by radioimmunoassay and allied techniques.
A significant contribution to the safety of the worker can be made by appropriate planning of the clinical nuclear medicine department. ICPR Report 57 [1] and other specialized publications suggest a method to determine the broad requirements for planning a nuclear medicine facility[2-8].
The shielding requirements for a NM facility fall into two categories - structural shielding for the various rooms in the department and local shielding of the radionuclide sources used. Protecting against radiation emitted from patients who have been administered a radionuclide must be achieved by structural shielding and department design. Shielding requirements for the scanning area, the waiting room, patient toilets and other areas will be determined by the number of patients imaged, the activities administered, the radiopharmaceuticals used, the time each patient remains in each part of the facility, and the location of the facility and its environs.
The present work shows the results of the shielding assessment of the rooms of the nuclear medicine department of the "Marie Curie" Oncological Hospital in Camagüey. This was done in order to check whether existing structural barriers, devices for the shielding of the sources, and the planned organizational measures, will ensure compliance with the radiation protection requirements needed to ensure the protection of occupationally exposed personnel, members of the public and the environment due to this practice. In order to carry out this evaluation, the methodology, of the 5 steps, proposed by Canadian Nuclear Safety Commission [6] was used.
Materials and methods
The method, used in this assessment, considers the following parameters when calculating the dose estimates resulting from NM intended operations: Layout and construction of rooms, locations at which these radioactive substances and activities will be used, distances between the radioactive substance or patient and the occupied locations of other persons, occupancy of the other rooms in the nuclear medicine department and surrounding areas by persons other than the patient, radiopharmaceuticals and activities (Bq) to be used for the nuclear medicine procedures performed, and maximum number of patients per procedure to be treated, annually.
The following 5-step method for calculating dose estimates for Nuclear Medicine Room is the used approach [6,7]:
Step 1) Obtain architectural drawings or make an accurate, scaled and dimensioned drawing of the facility and surrounding areas.
Step 2) Identify the key locations where radioactive substances are to be used and the number of procedures, as well as the typical activity per procedure, for each of these locations [9-12].
Step 3) Identify the purpose, type of occupancy and occupancy factor of those areas within, or in the immediate vicinity of, the nuclear medicine department, that will be occupied while radioactive substance are in use [9,10].
Step 4) Estimate the radiation dose rates produced in each potentially occupied area.
The following approach assumes the source/patient can be approximated as a point source. A general formula for performing dose rate calculations for a point source is:
Where:
Dij |
is the dose rate produced by radioactive substance i at location j, µSv.h-1 |
Γi |
is the specific gamma ray constant for radioactive substance i from a patient, µSv.h-1.MBq-1.m2[13] |
Ai |
is the activity of radioactive substance i, MBq |
dij |
is the distance between radioactive substance i and location j, m |
Sm |
is the thickness of shielding material m in any shielded barrier between radioactive substance i and location j, mm |
TVLmi |
is the “Tenth Value Layer” thickness of material m for radioactive substance i,mm. |
Step 5) Extrapolate the measured or calculated dose rates at each location to annual doses for the persons who may occupy each area, based on the projected facility workload and the occupancy factor.
Where:
Hij |
is the annual dose produced by radioactive substance i at location j, (mSv.year-1) |
N |
is the number of procedures per year. |
T |
is the occupancy factor |
Dij |
is the dose rate produced by radioactive substance i at location j, (µSv.h-1) |
ti |
is the duration of time in which the source or injected patient is present at the designated position. |
Results and discussion
Using the method outlined above of the 5 steps, the following approach has been used to estimate the doses to persons (other than the patient) in and around a nuclear medicine room.
Step 1) Nuclear medicine department layout: construction of rooms; locations at which these radioactive substances and activities will be used.
Figure 1 shows a nuclear medicine department layout. Key locations where nuclear medicine patients (with administered activity), occupationally exposed workers and members of the public will be present for significant periods of time over the course of the workday are identified using red, blue and green circles, respectively.
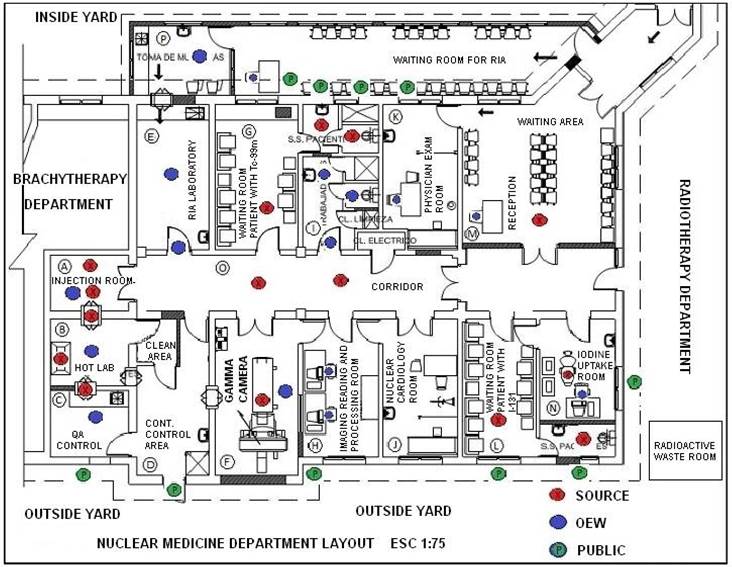
Figure 1 Nuclear medicine service layout, location of sources, and annual dose calculation points for REWs and members of the public.
It was assumed that the nuclear medicine department shown in Figure 1 primarily performs two types of outpatient diagnostic procedures: diagnostic bone scans and thyroid uptake analysis. The typical yearly workload and details of the nuclear substances and activities used are presented in Table 1 and Table 2 show principal working rooms and location of radioactive sources. The annual number of procedures performed is estimated from the daily procedure performed by assuming five days of operation per week and 50 weeks per year.
Table 1 Main expected diagnostic procedures, radionuclides to be used and annual workload.
| Procedure | Radionuclide | Number of procedures per year | Average Procedure duration, h | Average Activity Per Treatment, MBq | (No. of Proc.) x (Duration) x (Activity), MBq.h per year |
|---|---|---|---|---|---|
| Bones cans | 99mTc | 2000 | 0.75 | 740 | 1110000 |
| Thyroid uptake | 131I | 2500 | 2 | 0.925 | 4625 |
Step 3) Identification of the local purpose and occupancy factor of the areas within or in the immediate vicinity of the nuclear medicine department, which will be occupied while the sources are in use.
For each location in and around the facility where a significant contribution to the total dose received by a person would be expected, the dose to each representative person, assuming an appropriate occupancy factor, has been determined. The presence of REWs, non-REWs, or both, at these locations has been specified. If an individual that occupied several of these locations, the dose from all locations were computed (this scenario should be considered when assigning occupancy factors). Occupancy factors have been taken from NCRP 151[9].
Table 2 Nuclear medicine department room and location of sources.
| Department rooms | Location of sources | Source Code |
|---|---|---|
| Dose administration room (A) | Syringe in the center of the room # 1 and the patient post administration on the table # 2: total residence time 2 minutes | A1 y A2 |
| Hot room (B) | Hot cell (radiochemical cell) and transfers to local A and C (B5 and B6) | B1, B2, B3, B4, B5 y B6 |
| Quality Control room (C) | In stainless steel table with Pb shield to carry out the chromatographic analyzes. Measurements in the well counter. | C1 |
| Radiological control room (D) | There should be no sources | D |
| Room of study "In vitro"(E) | Sources of 125I excepted due to low activity. | E1 |
| SPECT room (F) | The patient lying on the patient table in the center of the room | F 1 |
| Patient waiting room for administered doses of 99mTc-MDP (G) | In the center of the room and in patient bathroom in front of the toilet and handwasher. | G1, G2 y G3 |
| Patient waiting room for administered doses 131I (L) | In the waiting room and in the patient toilet. | L1 y L2 |
| Thyroid Iodine uptake room (N) | Patient in position to perform the measurement | N1 |
| Inside corridor of the department (O) | Several points through which patients with incorporated doses will transit. | O1,O2,O3 y O4 |
Table 3 Summary of rooms and sources of a significant contribution to the dose in each room.
| REWs | Members of thepublic | Areas where the permissible dose limits for REWs or members of the public must be guaranteed. | Source Location(s) Making Significant Contribution to Dose | Rationale of the proposal and comments. |
|---|---|---|---|---|
| Yes | No | Room of study "In vitro" | G1,G2,O1 | The sources A1, A2, B1, B2, B3, B4, B5, C1, F1, L1, L2, L3, O1, O2, O3, and O4 are excluded because the distance to which they are located, the walls and shields present will significantly attenuate their influence. |
| Yes | No | dose administration room | A1,A2, G1 | The sources BI, B2, B3 and B4 are excluded because they are adequately shielded and L1, L2, L3 because the distance to which they are located, the walls and shields present will attenuate their influence significantly. O1, O2, O3, O4 are also not taken into account because they must not occur simultaneously in the organization of the work. C1 is prior to the administration of radiopharmaceuticals. |
| Yes | No | Hot room | A1,A2,B5, F1, G1 | The rest of the sources are not taken into account because the distance to which they are located and the walls present will attenuate their influence in the point of calculation. |
| Yes | No | Radiopharmaceutical quality control room | C1 | In this particular case, only the sources that are inside the hot cell will be present. They will be properly shielded. |
| Yes | No | SPECT room | G1, F1, A1, A2 | The rest of the sources are not taken into account, because the shields and walls present attenuated significantly its influence, C1 is prior to the administration of the radiopharmaceutical. |
| Yes | No | Image acquisition and processing station | F1, G1,O2,O3 | The sources B1, B2, B3, B4, O1 and O4 are not taken into account because the distance and walls present attenuated their influence, and the sources C1, B6 because it is prior to the administration of the radiopharmaceutical. |
| Yes | Yes | Waiting room | G1,O4,L1, L2,N1 | The rest of the sources are not taken into account since the radiation emitted by the patients present in those premises must cross several walls to reach this area and the others are also shielded. |
| Yes | No | Thyroid Iodine uptake room | N1,L1, L2 | The sources A1, A2, B1, B2, B3, B4, B5 G1, G2, and G3 are not taken into account because the distance and walls present will significantly attenuate their influence. |
| Yes | Yes | Nuclear physician consultation | G1, G3, L1 | The sources A1, A2, B1, B2, B3, B4, B5, F1, G2, L2, and N1 are not taken into account because the distance and walls present will significantly attenuate their influence. |
| Yes | No | Radioimmunoassay laboratory | G1,G2, O1 | The sources A1, A2, B1, B2, B3, B4, B5, B6, C1, O2, O3, O4, L1, L2, and N1 are not taken into account because the distance and walls present will significantly attenuate their influence. |
| No | Yes | Radioimmunoassay laboratory waiting area | G1,G2,O2 | The influence in the local D is neglected due to the low activity of 125I with which it is worked in the place. |
| No | Yes | Members of the public in areas outside the department | G1, G2, G3, F1,L1,L2 | Only sources whose proximity to the point of calculation will give a significant contribution to the annual dose will be taken into account. |
Description of sources:
| A1: | Syringe with 740 MBq of unprotected 99mTc-MDP at the administration site. (duration of the vein channeling procedure and injection of the radiopharmaceutical 1 minute approximately). |
| A2: | Patient with 740MBq of 99mTc-MDP, post-administration, (duration time 1 minute maximum in the room). |
| B1: | Bulb with the avoidance of 99mTc generator with maximum activity of 20 GBq (inside biosafety cabinet in a Pb container with 5 mm thickness), duration time 3 minutes, 5 times a week. |
| B2: | Bulb with eluate, with maximum activity of 20 GBq in the doses calibrator inside the hot cell, duration time 5 minutes per day, 5 times per week. |
| B3: | Bulb with the radiopharmaceutical already prepared placed inside a 5 mm Pb container, with a maximum activity of 20 GBq inside the hot cell (8 hours daily for 5 days a week). |
| B4: | Syringe with 740 MBq of 99mTc-MDP without protector during dose fractionation and measurement of activity within the hot cell. |
| B5: | Syringe with 740 MBq99mTc-MDP inside the syringe holder with a thickness of 2mm Pb, duration time 0.5 minutes in the transfer with room A. |
| B6: | Syringe with minimum dose of Radiopharmaceutical to carry out chromatography in transfer with the local C. |
| F1: | Patient with 555 MBq of 99mTc-MDP, post-administration lying on the patient table during positioning and carrying out the study for 45 minutes. (for the purpose of armor calculation the patient was considered a point source located in the center of the room at the height of the torso of a hypothetical patient in supine position on the patient table-stretcher). |
| F2: | Administration of 99mTc-MDP dose for renal dynamic study. (it will not be taken into account for the dose calculations in this work). |
| G1: | Three patients awaiting image acquisition with 740 MBq of 99mTc-MDP administered: duration time 2 h. (to calculate the contribution to the dose of this source all patients were considered as a point source located in the center of the waiting room). |
| G2: | Patient with 740 MBq of 99mTc-MDP administered in the restroom in front of the lavatory maximum time of stay 3 minutes. |
| G3: | Patient with 740 MBq of 99mTc-MDP administered in the bath versus the rate: maximum stay time of 3 minutes. (from the first hour of stay in the room the patient must make at least 4 mictions. |
| L1: | Eight patients with 0.925 MBq of 131I administered, awaiting measurement for determination of thyroid 131I uptake, waiting time 2h maximum. (to calculate the contribution to the dose of this source all patients were considered as a point source located in the center of the waiting room). |
| L2: | Patient with administered doses of 131I in the bath. (the 50 patients per week will be considered to have at least one micturition, with a maximum time of 3 minutes). |
| N1: | Patient at the measurement site to determine the percentage of thyroid 131I uptake. |
| O1: | Patient administered doses, in transit from room A, to room G. For the purposes of calculation, the patient will be considered as a point source located in the center of the hallway for 0.5 minutes. |
| O2: | Patient with doses administered, in transit from the local G, to the local F. For the purposes of the calculation the patient will be considered as a point source located in the center of the aisle for 0.5 minutes. |
| O3: | Patient with doses administered in transit from room F, towards the exit, at the moment that passes in front of the bathroom door. For the purpose of the calculation, the patient will be considered as a point source located approximately 1.2 m from the bathroom door and image processing room for 0.5 minutes. |
| O4: | Patient with doses administered in transit from the local F, towards the exit, in the moment that passes in front of the secretary in the waiting room. For the purpose of the calculation, the patient will be considered as a point source located 1.2 m from the secretary's desk for 0.5 minutes. |
General considerations
The 99mTc-MDP will be considered as the radiopharmaceutical that will contribute the most to the annual workload between all the expected diagnostic procedures due to the administered doses and the required radiological safety conditions.
Exceptionally 131I for thyroid iodine uptake will be included for the calculation of the doses received by the secretary, due to the proximity between the patient waiting room with administered doses of 131I and the waiting room of patients without administered doses.
99mTc-MDP average activity to be administered per patient for bone scintigraphy will be: 740 MBq, the hospital will mainly serve adult patients.
131I Average activity to be administered per patient for thyroid iodine uptake: 0.925 MBq (25 μCi).
Total, maximum patients per week for diagnosis with 99mTc-MDP: 40 (8 per day)
Total, maximum patients per week for diagnosis with 131I: 50 (10 per day)
Patient waiting time with administered 99mTc-MDP in the room: 120 min
Patient waiting time with administered 131I in the room: 120 - 240 min
Patient stay time in the SPECT room will be 45 minutes (patient positioning acquisition of the images)
Patient residence time in the measurement site of 131I: 5 min uptake
Doses restriction limit for occupationally exposed workers (OEWs): 6 mSv/year = 0.12 mSv/week = 120 µSv/week
Doses restriction limit for members of the public: 0.2 mSv/year = 0.004 mSv/week = 4 µSv/week
Annual work time: 50 week/year, 5 day/week, 8 h/day.
The occupancy factors were obtained from the report No.151 of the NCRP and in the cases that was necessary for not being foreseen in the above mentioned report, it was estimated on the basis of the nuclear medicine service experience in the realization of the practices, as well as the characteristics of the rooms and their use.
It is considered that the patient receives instructions previously about his preparation for the diagnostic study and that after receiving the dose in the administration room will be explained again the behavior that must follow within the department and its importance.
Points were identified within the rooms of the Department of Nuclear Medicine, where the sources that have a significant contribution to the annual dose will be located.
Points were identified at the rooms of the nuclear medicine department and in the areas surrounding it where annual dose control is important for both occupationally exposed workers and members of the public, taking into account the technological flow of the service.
Following the 5 step approach and general consideration described above, equation 1, considerations for calculations below and data showed in the Table 4, the dose rate calculations were carried out assuming that the source/patient can be approximated as a point source. For most distances, the point source is a sufficiently accurate representation.
Considerations for calculations
In all cases, the data will be maximized to obtain the greatest workload.
For the purposes of calculations, Bone Scan is considered as the only imaging study performed in the service at the rate of 8 patients per day during the 5 days of the week, this will maximize the workload.
The criteria for the shielding of the different types of barriers were taken: the number of walls that must pass through the radiations to the point of calculation, the Pb devices available for the shield and also the technological flow of each procedure to avoid as long as their temporal coincidence is possible.
To determine the influence on the annual dose of each of the sources at the selected points, the calculations were initially performed using only the contribution to the shielding of existing Pb devices in the service (1TVL Pb for 99mTc = 1mm) and did not take into account the contribution of the walls in the attenuation of radiation beam, then in a process of decanting were eliminated those sources whose contribution did not significantly modify the total annual dose obtained. Then the shielding provided by the walls based on a well-grounded approach was applied because the TVL of 99mTc is not available for clay bricks or for veneering in tiles but they were estimated from results of mass attenuation coefficients reported by Singh-Mann (2013) for clay bricks, [14].
It will be assumed in the contribution to the shielding of the walls that they are only brick covered with a thick layer of cement-sand: the inner walls with their thickness of 16 cm provide the equivalent of 1 TVL of Pb and 2 TVL in the case of exteriors that has a thickness of 29 cm, did not take into account the contribution to the shielding of the tiles and doors.
For the purposes of the calculation, the patient with administered doses will be considered a point source located in the center of the patient's torso (60 cm from the head).
Table 4 Half life, typical equivalent dose rates constant and Tenth value layer (TVL) thicknesses for used gamma-emitting radionuclides [7].
| Radionuclide | T1/2, d | Equivalent dose rate (μSv.h-1/MBq) at 1 m from a: | TVL(Pb), mm | |
|---|---|---|---|---|
| point source | patient | |||
| 99mTc | 6.02 | 0.0195 | 0.0075 | 1.0 |
| 131I | 8.06 | 0.0575 | 0.0230 | 11.0 |
An example of dose rate calculation is showed in the Table 5.
Table 5 Dose rate received by REW due to the use of 99mTc in the dose administration room during activity injection process.
| Exposedperson | Place where it is located | Sourcelocation | dij(m) | Sm (mm) | A (MBq) | Dij (µSv/h) |
|---|---|---|---|---|---|---|
| OEW | doseadministrationroom | A1 | 0.64 | 0 | 740 | 13.66 |
| A2 | 1.06 | 0 | 740 | 4.96 | ||
| G1 | 6.38 | 1 | 22201 | 0.04 | ||
| 18.65 |
1 Three (3) patients with 740 MBq administered activity.
The total effective dose estimated per year (equation 2), for any given combination of procedure, source location, occupied location and exposed person, is given by the product of the total number of procedures performed per year (N, see Table 1); the occupancy factor for the exposed person and occupied location (T, see Table 3); the dose rate (Dij, see Table 5); and the duration of time (ti) the source/injected patient is present at the designated source location (in hours). The annual dose (Hij) is summarized in the Table 6.
Table 6 Summary of results: Annual effective dose.
| Calculation point | T | ti (h) | H (mSv/y) | Observations |
|---|---|---|---|---|
| REW: At the door of local E during the dose administration | 1/16 |
|
0.045 | The annual dose at this point is below the dose restriction limit (6 mSv/year) for the practice of nuclear medicine. |
| REW: Doses administrationroom | 1/2 |
|
0.56 | The annual dose at this point is below the dose limit of 6 mSv, however it may be reduced if the syringe guard is used to administer the dose, and if a rotation of the staff is also established to perform this procedure. |
| REW: Hot room | 1/2 |
|
0.47 | The annual dose at this point is well below the dose restriction limit 6 mSv/y |
| REW:SPECT room | 1 |
|
0.47 | The annual dose at this point is well below the dose restriction limit 6 mSv/y |
| REW: Imaging processing station | 1 |
|
0.28 | The annual dose at this point is well below the dose restriction limit 6 mSv/y |
| REW: Secretary in the waiting room | 1 |
|
0.43 | The annual dose at this point is well below the dose restriction limit 6 mSv/y |
| REW: Physician Consultation | 1/2 |
|
0.81 | The annual dose at this point is well below the dose restriction limit 6 mSv/y |
| REW: RIA laboratory | 1 |
|
2.18 | The annual dose at this point is below the dose limit of 3 mSv/y, however, organizational measures have to be implemented to reduce it. |
| REW: Workers bathroom in front the handwasher | 1/16 |
|
0.66 | The annual dose at this point is below the dose limit of 6 mSv/y,however, organizational measures have to be implemented to reduce it. |
| REW:Workers bathroom in front of the toilete | 1/16 |
|
0.17 | The annual dose at this point is below the dose limit of 6 mSv/y. |
| REW: Workers bathroom in the shower. | 1/16 |
|
0.14 | The annual dose at this point is below the dose limit of 6 mSv/y, however, organizational measures have to be implemented to reduce it. |
| Public: Outside area in front of the wall facing the room L. | 1/4 |
|
0.12 | The annual dose at this point is close to the dose limit of 0.2mSv/a. However, it is necessary to take measures to avoid the presence of members of the public when working on the premises. Limit traffic in this area. |
REW - Occupationally exposed worker to radiation.
In all other locations: outside area in front of the wall that give to the room N, outside area in front of the wall that gives to the bathroom of the room L, outside area in front of the corner that forms the wall that gives to the room of the SPECT and the one of the place of the image acquisition, outside area in front of the wall that gives to the SPECT room, person in front of the desk of the RIA laboratory receptionist and patient 1 and 2 waiting for extraction;the annual effective dose are not significant, they are between 0.012 and 0.069 mSv/y.
Conclusions
The shields provided for the radioactive sources and walls of the rooms ensure the protection of occupationally exposed workers and members of the public to radiation, however there are procedures where the annual dose can be reduced, such as the administration of radiopharmaceuticals where the use of the syringe protector to administer the dose of radiopharmaceuticals and implement organizational measures in the rooms and outside areas where it is necessary to achieve the reduction of doses to the levels that can reasonably be achieved, such as the exterior areas of the room L.














