Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de Ciencias Médicas de Pinar del Río
versión On-line ISSN 1561-3194
Rev Ciencias Médicas vol.26 no.3 Pinar del Río mayo.-jun. 2022 Epub 01-Mayo-2022
Original Article
Chronic diseases and smoking in SARS-CoV-2 infection in Pinar del Rio
1University of Medical Sciences of Pinar del Río. Provincial Pediatric Teaching Hospital "Pepe Portilla". Pinar del Río, Cuba.
2University of Medical Sciences of Pinar del Río. Faculty of Medical Sciences "Dr. Ernesto Che Guevara de la Serna". Pinar del Río, Cuba.
3University of Medical Sciences of Havana. Finlay-Albarrán School of Medicine. Havana, Cuba.
4Ministry of Public Health. Havana, Cuba.
5University of Medical Sciences of Pinar del Río. Provincial Directorate of Health. Pinar del Río, Cuba.
Introduction:
the world deals with a new pandemic because of SARS-CoV-2 outbreak initiated in Wuhan, China in December 2019. Host genetic differences and risk factors such as: personal history, lifestyles and environmental factors may contribute to the marked inter-individual clinical variability in COVID-19.
Objective:
to identify personal pathological history (chronic diseases and smoking) associated with SARS-CoV-2 infection.
Methods:
analytical, observational study of cases and controls in Pinar del Rio in the period from March 2020 to March 2021. Personal history of chronic diseases and smoking as an environmental factor were explored.
Results:
personal pathological history of allergies and asthma constituted risk factors to develop symptoms. History of active smoking is presented as a risk factor for infection.
Conclusions:
the contribution of personal pathological history (allergy and asthma) and environmental (active smoking) to SARS-CoV-2 infection and to the development of symptoms in COVID-19 patients in Pinar del Rio is confirmed.
Key words: COVID-19; SARS-COV-2; CORONAVIRUS; CHRONIC DISEASE; SMOKING
INTRODUCTION
More than 100 years after the 1918 influenza pandemic that caused 50 million deaths, the world is facing a new pandemic with the outbreak of SARS-CoV-2 causing COVID-19 that has spread to all continents.1 The new coronavirus appeared at the end of the 1918 influenza pandemic in Pinar del Rio.
The new coronavirus appeared at the end of December 2019, in Wuhan, a commercial city in central China.1
SARS-CoV-2 disease is clinically similar to other CoV infections in humans. Eighty percent of CoVID-19 sufferers have a mild respiratory clinical picture and are more common in children, adolescents and young adults. Fifteen percent present a severe picture, and 5 % require intensive care and are frequently seen in those over 65 years of age and in persons with non-communicable diseases such as diabetes mellitus, chronic obstructive pulmonary disease, cardiovascular or cerebrovascular disease, and arterial hypertension.2
Mortality from the disease affects 1 in 1,000 infected persons younger than 50 years with no underlying conditions, but more than 1 in 10 patients older than 80 years with multiple comorbidities.2
In SARS-CoV-2, host genetic variation may be a key factor influencing susceptibility, severity, and overall clinical outcomes of COVID-19 patients. In addition, gene expression also differs according to an individual's sex, lifestyles, and biological age.3
Aging is associated with the accumulation of molecular and cellular changes that reduce certain biological functions and decrease the immune response. It is also associated with an increased incidence of non-communicable diseases and low-grade inflammation.4
On the other hand, the environment also has an impact on susceptibility to infection. It comprises all non-genetic factors that modulate the phenotype and may include both random environmental factors (climatic, geographic, demographic and socioeconomic) and lifestyle (diet, smoking, alcoholism and physical activity), which can be modified by the individual.5
Over the last decades, evidence has linked short- and long-term exposures to environmental pollution to the development of respiratory diseases and mortality from them.6
Permanent exposure to particulate matter compromises respiratory health status and weakens immunity, which promotes exposure to infectious particles and stimulates stress, which also favors epidemiological peaks of respiratory disease. In SARS-CoV-2 infection, there is evidence of association with environmental pollution.6
Smoking is a risk factor for many viral and bacterial respiratory infections that increase their severity. It has been shown that smokers, as well as those exposed to smoke (passive smokers), are more likely to contract influenza, pneumonia and tuberculosis. It is also observed that smokers had a higher morbidity and mortality during the MERS outbreak originating from MERS-CoV.7
In this sense, smoking could play a deleterious effect on SARS-CoV-2 infection. Active or passive smokers could have a greater vulnerability to infection or an unfavorable evolution of COVID-19.
In any disease, the combined effect of genetic and environmental factors is observed. SARS-CoV-2 infection and COVID-19 depend on SARS-CoV-2 interaction/host/environmental factors or history.3 Hence, the present investigation aims to identify personal pathological history (comorbidities and smoking as an environmental factor) associated with SARS-CoV-2 infection and clinical course of COVID-19 patients.
METHODS
An epidemiological, observational analytical investigation of cases and controls was performed; according to four groups: cases/controls, asymptomatic/controls, symptomatic/controls, symptomatic/asymptomatic; for all analyses. The research was carried out in the municipalities affected by COVID-19 in Pinar del Río province during the period from March 2020 to March 2021 (Pinar del Río, Consolación, San Luis, Guane, Viñales, La Palma and Sandino).
A sample size of 450 individuals was taken, including 150 cases of autochthonous transmission with diagnosis of COVID-19 by polymerase chain reaction (PCR) and 300 controls selected from the same population that gave rise to the cases, paired in sex and age group.
To obtain the controls, a simple random sampling was also performed, matched by sex and age, from the same population that gave rise to the cases, complying with the 1:2 ratio.
A questionnaire was applied in primary health care that collected the general data of the cases, personal history of non-communicable diseases, and smoking as an environmental factor. (Table 1)
Table 1 Variables used to explore personal history in the study of risk factors in SARS-CoV-2 infection and in the clinical presentation of COVID-19 in Pinar del Río.
| Joint or general variables | Variables |
|---|---|
| Personal pathological history of NCD | Hypertension, diabetes, obesity, asthma, allergy, other cardiac diseases, vascular diseases, autoimmune diseases, chronic obstructive pulmonary disease (COPD). |
| Smoking (environmental factor) | Active smoker, passive smoker, former smoker. |
In the analysis of the frequency of personal history of communicable diseases and smoking, an analysis of association was performed for each variable individually, using Pearson's Chi-square test of homogeneity and independence, with a significance level equal to 0.05. The Odds ratio and its confidence interval were determined as the magnitude of association.
The principles of medical ethics and the aspects established in the Helzinki Declaration were complied with.
RESULTS
Analysis of personal history of noncommunicable diseases in SARS-CoV-2 infection and the clinical presentation of COVID-19
Of the nine diseases explored in the frequency analysis of personal history of non-communicable diseases, it was observed that arterial hypertension (26,9 %), allergy (20,0 %), autoimmunity (14,9 %) and asthma (12,9 %) were the entities with the highest percentages for both cases and controls. In the cases, these morbidities were more frequent in the group of symptomatic patients compared to the asymptomatic ones.
The frequency of allergy, asthma and autoimmune diseases was higher in cases than in controls with values of 24,7 %, 15,3 %, 14,7 % respectively, although only the proportions of allergy and asthma showed significant results (Fig. 1).
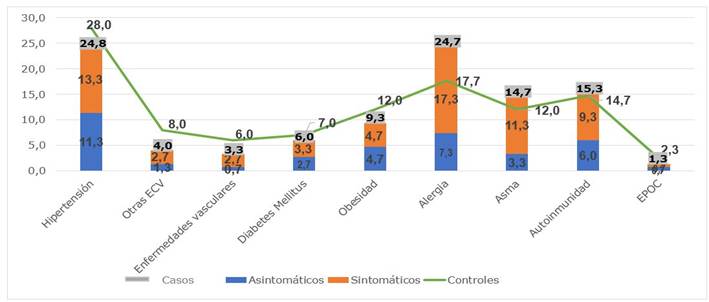
Fig. 1 Frequency distribution of non-communicable diseases in cases and controls in the study of risk factors in SARS-CoV-2 infection and in the clinical presentation of COVID-19.
In the analysis of the case/control and asymptomatic/control groups, no significant results were found for any of the comorbidities evaluated. However, for the symptomatic/control and symptomatic/asymptomatic groups, significant results were found for allergy and asthma. For allergy, in the symptomatic/control group a predominance was found in symptomatic cases with an OR of 2.054 and for asthma an OR of 1.833 was observed. In the symptomatic/asymptomatic group allergy and asthma also predominated in symptomatic for an OR of 2.241 and 3.096 respectively.
Table 2 Frequency analysis of history of allergy and asthma in the study of risk factors in SARS-CoV-2 infection and in the clinical presentation of COVID-19, Pinar del Río.
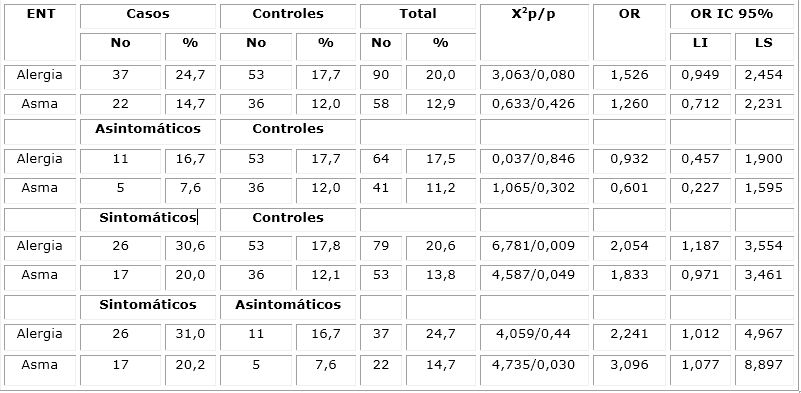
Symbology: NCD: non-communicable diseases, X2p: Pearson's Chi-Square, OR: Odds Ratio, OR 95 % CI: 95 % confidence interval, p: probability.
Analysis of personal smoking history in SARS-CoV-2 infection and clinical presentation of COVID-19.
Of the three smoking variables analyzed: active smoker, passive smoker, ex-smoker; results of statistical significance were obtained only for the history of active smoking.
The most representative results are exposed, the rest shows the frequency of active smokers in cases and controls in the study of risk factors associated to SARS-CoV-2 infection and to the course of COVID-19 in Pinar del Río, four groups are analyzed (case/control, asymptomatic/control, symptomatic/control, symptomatic/asymptomatic). (Table 3).
A predominance was found in the cases with respect to the controls for the variable active smoker, which showed an OR 1.427.
Table 3 Frequency analysis of active smoking as an environmental factor in the study of risk factors in SARS-CoV-2 infection and in the clinical presentation of COVID-19.
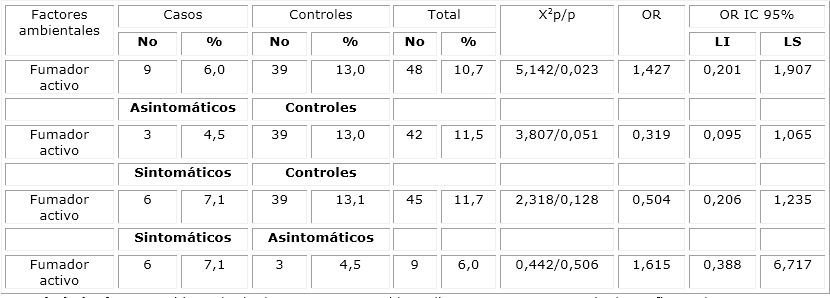
Symbology: X2p: Pearson's Chi Square, OR: Odds Ratio, OR 95% CI: 95% Confidence Interval, p: probability.
An individual with a history of being an active smoker has a higher risk of presenting the infection when compared to non-smokers.
DISCUSSION
Since the emergence of SARS-CoV-2 and COVID-19, the highest mortality of cases is observed in patients with non-communicable diseases, and in those over 60 years of age are considered populations ten times more likely to die.8
A Medscape meta-analysis compiling studies from the year 2020 shows the prevalence of arterial hypertension and its exponential increase with age together with other cardiovascular diseases that contribute to the severe and critical evolution of cases with COVID-19.9
In China, with the first 44,672 confirmed cases, the case fatality rate reached 4,7 %. Studies in these cases show that patients without comorbidities have a lower case fatality rate (0,9 %). For those with cerebrovascular disease, diabetes mellitus and arterial hypertension have higher rates (10,5 %, 7,3 %, 6,5 % respectively).10
Arterial hypertension is a health problem that affects 45 % of the world population, and in Cuba 30 % of the population. In Pinar del Río, the prevalence of arterial hypertension is 269,9 per 1,000 inhabitants, which is higher than in the rest of the provinces.11
In the study by Zhang et al, arterial hypertension is the most frequent comorbidity with 30% of the patients, it is also associated with lethality and states that hypertensive patients have a 3.48 times higher risk of suffering complications.12
Another investigation considers arterial hypertension as a risk factor for severe or fatal COVID-19, without clarifying the underlying mechanism. However, it hypothesizes that the virus enters the host cell through the angiotensin-converting enzyme receptor 2 (ACE2) and endocytosis of the virus-ACE2 complex reduces its function. All of this leads to overactivation of the renin/ angiotensin/ aldosterone complex; and complications such as acute respiratory distress syndrome and multiorgan failure.13
In this research, arterial hypertension constituted one of the most frequent diseases due to its high rate in the population of Pinar del Río, with no predominance of cases with respect to controls. It is necessary to emphasize that the study is carried out with the first cases of COVID-19 in Pinar del Río province, months after the beginning of the pandemic in most of the countries. Therefore, the sample is scarce with a reduced number of symptomatic patients.
The higher proportion of autoimmune diseases and rheumatologic manifestations in the cases could complicate the clinical course of the patients, given that robust immune reactions participate in the pathogenesis of both diseases.14
Results from a cross-sectional study in northeastern Italy indicate that patients with autoimmune diseases have infection rates similar to the general population in contrast to the research presented.15
However, an exaggerated immune response is known to mediate the more severe complications induced by SARS-CoV-2. Results from studies in China and Spain agree that patients with autoimmune diseases could be more prone to SARS-CoV-2 infection and have a more severe course when compared to controls.15 In the current study, even with a high frequency of autoimmunity, no statistical association is observed. The lack of description of the type of autoimmune disease is a limitation.
Historically, the relationship between viral infections, immune response, allergy and asthma has been proposed. Several viruses, such as rhinoviruses and respiratory syncytial virus, have been the main focus of research.16
Asthma affects 4,4 % of the world population and allergic diseases increase with time and the industrial revolution. In Cuba, studies show that 45 % of the adolescent or young adult population suffers from allergies and that one out of every two people is asthmatic.17 The prevalence of asthma in Pinar del Río is 8,9 per 100 inhabitants,18 which could explain the frequency of this disease in the study population.
In respiratory allergies, genetic predisposition, deficient antiviral response with reduced levels of INF-β and INF-γ, deterioration of immune cells, together with epithelial damage and cytokine response may contribute to increased susceptibility to viral infection, incomplete viral clearance and persistence of airway inflammation, leading to adverse clinical outcomes.19 A study in 182 children with COVID-19, shows that 43% were allergic, with lower elevation of acute phase reactants and no deaths reported. 20
In previous respiratory virus epidemics, there are contrasting results regarding the influence of asthma on clinical course and prognosis. Data from the 2003 SARS epidemic report that asthmatics have a reduced susceptibility to the coronavirus, with good prognosis while, in 2009, the H1N1 pandemic associates asthma with severe disease and need for ventilation.19
Furthermore, the study findings are consistent with the U.S. weekly mortality and morbidity report showing that 27 % of patients with moderate/severe COVID-19 symptomatology had asthma, which is higher than the U.S. asthma prevalence rate of 10 %.21
According to the World Health Organization (WHO), tobacco causes the death of 8 million people worldwide annually, and more than 7 million of these deaths are from direct tobacco use.22
Smoke exposure modulates innate and adaptive immune responses in humans. Systemic levels of inflammatory markers in smokers are reduced when compared to non-smokers.23
Graufi et al. in their review state that the vast majority of patients hospitalized for COVID-19 are non-smokers,23 contrary to the findings obtained in the study. However, the study by Graufi et al. refers only to hospitalized patients. The prevalence of smoking in asymptomatic non-hospitalized patients is not known, which is a bias in the research.23
For its part, the WHO highlights the likelihood that smokers are more vulnerable to infection by the new CoV because of cigarette handling and contact of cigarettes with lips,24 which is consistent with the results achieved in the study.
There are several reasons to assume that smokers are at higher risk for acquiring SARS-CoV-2 infection:
(a) There is evidence that infections by other viruses of the same family, such as MERS-CoV-2 affect smokers more frequently. 24
b) There is evidence in the medical literature that respiratory infections caused by bacteria or viruses are more frequent in active smokers 24
c) Toxic substances in tobacco smoke damage the immunologic, cellular and humoral mechanisms of the upper respiratory system. 24
d) In smokers, the hand-mouth movement is repeated frequently, making them more likely to suffer from an orally transmitted infection. 24It is also important to note that social isolation and social isolation are also important in smokers.
It is also important to note that social isolation and the quarantined state of the home, which encourages active smokers to expose non-smokers to secondhand smoke. Unfortunately, the latter can cause homologous harms to passive smokers.7
The research results demonstrate the contribution of personal (allergy and asthma) and environmental (active smoking) pathological history to SARS-CoV-2 infection and symptom development in COVID-19. Much remains to be clarified regarding this relationship, so more in-depth national and international cohort and experimental studies are required.
However, it is confirmed that host factors play a crucial role in SARS-CoV-2 infection: genes and comorbidities; those inherent to the virus; lifestyles and environmental factors (smoking) that regulate the clinical heterogeneity and evolution of patients affected by COVID-19.
REFERENCES
1. Cajamarca Baron J, Guavita Navarro D, Buitrago Bohorquez J, Gallego Cardona L, Navas A, Cubides H, et al. SARS-CoV-2 (COVID-19) en pacientes con algún grado de inmunosupresión. Reumatol Clínica [Internet]. 2021 [citado: 21/10/2020]; 17(7): 408-419. Disponible en: Disponible en: https://doi.org/10.1016/j.reuma.2020.08.004 1. [ Links ]
2. Min Z, Jun C, Fu F, Shu Q, Hu Y, Chun C, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr [Internet]. 2020 [citado: 15/03/2020]; 16: 240-246. Disponible en: Disponible en: https://doi.org/10.1007/s12519-020-00345-5 2. [ Links ]
3. Ovsyannikova IG, Haralambieva IH, Crooke SN, Poland GA, Kennedy RB. The role of host genetics in the immune response to SARS- CoV-2 and COVID-19 susceptibility and severity. Immunol Rev [Internet]. 2020 [citado: 21/10/2020]; 296(1): 205-19. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7404857/ 3. [ Links ]
4. Hanif M, Haider MA, Xi Q, Ali MJ, Ahmed MU. A Review of the Risk Factors Associated With Poor Outcomes in Patients With Coronavirus Disease 2019. Cureus [Internet]. 2020 [citado: 21/10/2020]; 12(9): e10350. Disponible en: Disponible en: https://doi.org/10.7759/cureus.10350%0A 4. [ Links ]
5. Radzikowska U, Traidl-hoffmann C, Akdis C, Sokolowska M, Au N, Ca A. Distribution of ACE2, CD147, CD26 and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy [Internet]. 2020 [citado: 21/10/2020]; 75(11): 2829-45. Disponible en: Disponible en: https://doi.org/10.1111/all.14429 5. [ Links ]
6. Rosas Arango SM, Ángel Caraza A, Del Ángel Caraza J, Soriano Vargas E. Infección por COVID-19 , una mirada a los factores ambientales relacionados con la pandemia. NOVA [Internet]. 2020 [citado: 21/10/2020]; 18(35): 101-5. Disponible en: Disponible en: https://doi.org/10.22490/24629448.4193 6. [ Links ]
7. Piñera Castro HJ, Ruiz Gonzalez LA. Implicaciones del tabaquismo en el contexto de la COVID-19. Rev cub med Mil [Internet]. 2022 [citado: 10/01/2022]; 51(1): e02201457. Disponible en: Disponible en: http://www.revmedmilitar.sld.cu/index.php/mil/article/view/1457/1014 7. [ Links ]
8. Wang, Dawei, Bo Hu, Chang Hu FZ, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA [Internet]. 2020 [citado: 21/10/2020]; 323(11): 1061-1069. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7042881/ 8. [ Links ]
9. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the Novel Wuhan Coronavirus (COVID-19) infection: a systematic review and meta-analysis. J Inter Infect Dis [Internet]. 2020 [citado: 21/10/2020]; 94(10): 91-5. Disponible en: Disponible en: https://www.sciencedirect.com/science/article/pii/S1201971220301363?via%3Dihub 9. [ Links ]
10. Costa de Lucena T, Fernandes da Silva Santos A, de Albuquerque Borborema ME, de Azevedo Silva J. Mechanism of in fl ammatory response in associated comorbidities in COVID-19. Diabetes Metab Syndr Clin Res Rev [Internet]. 2020 [citado: 21/10/2020]; 14(4): 597-600. Disponible en: Disponible en: https://doi.org/10.1016/j.dsx.2020.05.025 10. [ Links ]
11. Pérez Caballero MD, León Alvárez JL, Dueñas Herrera A, et al. Guía cubana de diagnóstico, evaluación y tratamiento de la hipertención. Rev Cuba med [Internet]. 2017 [citado: 21/10/2020]; 56(4): 242-231. Disponible en: http://scielo.sld.cu.php [ Links ]
12. Zhang JJ, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy [Internet]. 2020 [citado: 21/10/2020]; 75(7): 1730-41. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32077115/ 12. [ Links ]
13. Ravichandran B, Grimm D, Infanger M, Wehland M, Kopp S. SARS-CoV-2 and hypertension. Physiological Reports [Internet]. 2021 [citado: 06/10/2021]; 9(11): e14800. Disponible en: Disponible en: https://doi.org/10.14814/phy2.14800 13. [ Links ]
14. Li J, Liu HH, Yin XD, Li C. COVID-19 illness and autoimmune diseases: recent insights.pdf. Inflamm Res Off J Eur Histamine Res Soc [Internet]. 2021 [citado: 06/10/2021]; 70(4): 407-28. Disponible en: Disponible en: https://doi.org/10.1007/s00011-021-01446-1 14. [ Links ]
15. Zen M, Fuzzi E, Astorri D, et al. SARS-CoV-2 infection in patients with autoimmune rheumatic diseases in northeast Italy: a cross-sectional study on 916 patients. J Autoimmun [Internet]. 2020 [citado: 06/10/2021]; 112: 102502. Disponible en: Disponible en: https://doi.org/10.1016/j.jaut.2020.102502 15. [ Links ]
16. Michael RE, Stronf K, Cameron A, Walton RP, Jackson DJ, Johoston SL, et al. Viral Infections in allergy and immunology: How allergic inflamatio influences viral infections and illness. J Allergy Clin Immunol [Internet]. 2017 [citado: 06/10/2021]; 140(4): 909-20. Disponible en: Disponible en: https://doi.org/10.1016/j.jaci.2017.07.025 16. [ Links ]
17. L AF. Para la salud, debates científicos oportunos [Internet]. Granma [Internet] 2017 [citado: 06/10/2021]; (2): 2-3. Disponible en: Disponible en: https://www.granma.cu/todo-salud/2017-10-06/para-la-salud-dos-debates-cientificos-oportunos-06-10-2017-00-10-23 17. [ Links ]
18. Orraca O, Navarro E, Quintero W, Blanco TM, Rodríguez LR. Frecuencia de infecciones respiratorias agudas en niños y adolescentes con asma de la provincia de Pinar del Río. MEDISAN [Internet]. 2018 [citado: 06/10/2021]; 22(1): 33-9. Disponible en: Disponible en: https://scielo.sld.cu/scielo.php?script=sci-arttext&pid=S1029-30192018000100005&Ing=es 18. [ Links ]
19. Papadopoulos NG, Xepapadaki P. Papel de las infecciones virales en el asma. Salud(i)Ciencia [Internet]. 2017 [citado: 06/10/2021]; 22(6): 545-51. Disponible en: Disponible en: https://www.dx.doi.org/10.21840/siic/75594 19. [ Links ]
20. Licari A, Votto M, Brambilla I, et al. Allergy and asthma in children and adolescent during the COVID-19 ioutbreak: What we know and how we could prevent allergy and asthma flares. Allergy [Internet]. 2020 [citado: 06/10/2021]; 75(9): 2402-5. Disponible en: Disponible en: https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/es/covidwho-276469 20. [ Links ]
21. Hosoki K, Chakraborty A, Sur S. Molecular mechanisms and epidemiology of COVID-19 from an allergist ’ s perspective. J ALLERGY CLIN IMMUNOL [Internet]. 2020 [citado: 06/10/2021]; 146(2): 285-99. Disponible en: Disponible en: https://doi.org/10.1016/j.jaci.2020.05.033 21. [ Links ]
22. OMS. Declaración de la OMS: consumo de tabaco y COVID-19 [Internet]. 2020 [citado: 06/10/2021]. Disponible en: Disponible en: http://www.who.int/es/news/item/11-05-2020-who-statement-tobacco-use-and-covid-19 22. [ Links ]
23. Garufi Giovanna, Carbognin L, Orlandi A, Tortora G BE. Smoking habit and hospitalization for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)- related pneumonia: The unsolved paradox behind the evidence. Eur J Intern Med [Internet]. 2020 [citado: 10/01/2022]; 77(4): 121-2. Disponible en: Disponible en: https://doi.org/10.1016/j.ejim.2020.04.042 23. [ Links ]
24. Fernández Rúa JM. Nueva amenaza del tabaco en pacientes con COVID-19. Biotech Magazine [Internet]. 2021 [citado: 10/01/2022]; 3: 1-3. Disponible en: Disponible en: https://biotechmagazineandnews.com/nueva-amenaza-del-tabaco-en-pacientes-de-covid-19/ 24. [ Links ]
Funding
REFERENCES
1. Cajamarca Baron J, Guavita Navarro D, Buitrago Bohorquez J, Gallego Cardona L, Navas A, Cubides H, et al. SARS-CoV-2 (COVID-19) en pacientes con algún grado de inmunosupresión. Reumatol Clínica [Internet]. 2021 [citado: 21/10/2020]; 17(7): 408-419. Disponible en: Disponible en: https://doi.org/10.1016/j.reuma.2020.08.004 1. [ Links ]
2. Min Z, Jun C, Fu F, Shu Q, Hu Y, Chun C, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr [Internet]. 2020 [citado: 15/03/2020]; 16: 240-246. Disponible en: Disponible en: https://doi.org/10.1007/s12519-020-00345-5 2. [ Links ]
3. Ovsyannikova IG, Haralambieva IH, Crooke SN, Poland GA, Kennedy RB. The role of host genetics in the immune response to SARS- CoV-2 and COVID-19 susceptibility and severity. Immunol Rev [Internet]. 2020 [citado: 21/10/2020]; 296(1): 205-19. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7404857/ 3. [ Links ]
4. Hanif M, Haider MA, Xi Q, Ali MJ, Ahmed MU. A Review of the Risk Factors Associated With Poor Outcomes in Patients With Coronavirus Disease 2019. Cureus [Internet]. 2020 [citado: 21/10/2020]; 12(9): e10350. Disponible en: Disponible en: https://doi.org/10.7759/cureus.10350%0A 4. [ Links ]
5. Radzikowska U, Traidl-hoffmann C, Akdis C, Sokolowska M, Au N, Ca A. Distribution of ACE2, CD147, CD26 and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy [Internet]. 2020 [citado: 21/10/2020]; 75(11): 2829-45. Disponible en: Disponible en: https://doi.org/10.1111/all.14429 5. [ Links ]
6. Rosas Arango SM, Ángel Caraza A, Del Ángel Caraza J, Soriano Vargas E. Infección por COVID-19 , una mirada a los factores ambientales relacionados con la pandemia. NOVA [Internet]. 2020 [citado: 21/10/2020]; 18(35): 101-5. Disponible en: Disponible en: https://doi.org/10.22490/24629448.4193 6. [ Links ]
7. Piñera Castro HJ, Ruiz Gonzalez LA. Implicaciones del tabaquismo en el contexto de la COVID-19. Rev cub med Mil [Internet]. 2022 [citado: 10/01/2022]; 51(1): e02201457. Disponible en: Disponible en: http://www.revmedmilitar.sld.cu/index.php/mil/article/view/1457/1014 7. [ Links ]
8. Wang, Dawei, Bo Hu, Chang Hu FZ, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA [Internet]. 2020 [citado: 21/10/2020]; 323(11): 1061-1069. Disponible en: Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7042881/ 8. [ Links ]
9. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the Novel Wuhan Coronavirus (COVID-19) infection: a systematic review and meta-analysis. J Inter Infect Dis [Internet]. 2020 [citado: 21/10/2020]; 94(10): 91-5. Disponible en: Disponible en: https://www.sciencedirect.com/science/article/pii/S1201971220301363?via%3Dihub 9. [ Links ]
10. Costa de Lucena T, Fernandes da Silva Santos A, de Albuquerque Borborema ME, de Azevedo Silva J. Mechanism of in fl ammatory response in associated comorbidities in COVID-19. Diabetes Metab Syndr Clin Res Rev [Internet]. 2020 [citado: 21/10/2020]; 14(4): 597-600. Disponible en: Disponible en: https://doi.org/10.1016/j.dsx.2020.05.025 10. [ Links ]
11. Pérez Caballero MD, León Alvárez JL, Dueñas Herrera A, et al. Guía cubana de diagnóstico, evaluación y tratamiento de la hipertención. Rev Cuba med [Internet]. 2017 [citado: 21/10/2020]; 56(4): 242-231. Disponible en: http://scielo.sld.cu.php [ Links ]
12. Zhang JJ, Dong X, Cao Y, Yuan Y, Yang Y, Yan Y. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy [Internet]. 2020 [citado: 21/10/2020]; 75(7): 1730-41. Disponible en: Disponible en: https://pubmed.ncbi.nlm.nih.gov/32077115/ 12. [ Links ]
13. Ravichandran B, Grimm D, Infanger M, Wehland M, Kopp S. SARS-CoV-2 and hypertension. Physiological Reports [Internet]. 2021 [citado: 06/10/2021]; 9(11): e14800. Disponible en: Disponible en: https://doi.org/10.14814/phy2.14800 13. [ Links ]
14. Li J, Liu HH, Yin XD, Li C. COVID-19 illness and autoimmune diseases: recent insights.pdf. Inflamm Res Off J Eur Histamine Res Soc [Internet]. 2021 [citado: 06/10/2021]; 70(4): 407-28. Disponible en: Disponible en: https://doi.org/10.1007/s00011-021-01446-1 14. [ Links ]
15. Zen M, Fuzzi E, Astorri D, et al. SARS-CoV-2 infection in patients with autoimmune rheumatic diseases in northeast Italy: a cross-sectional study on 916 patients. J Autoimmun [Internet]. 2020 [citado: 06/10/2021]; 112: 102502. Disponible en: Disponible en: https://doi.org/10.1016/j.jaut.2020.102502 15. [ Links ]
16. Michael RE, Stronf K, Cameron A, Walton RP, Jackson DJ, Johoston SL, et al. Viral Infections in allergy and immunology: How allergic inflamatio influences viral infections and illness. J Allergy Clin Immunol [Internet]. 2017 [citado: 06/10/2021]; 140(4): 909-20. Disponible en: Disponible en: https://doi.org/10.1016/j.jaci.2017.07.025 16. [ Links ]
17. L AF. Para la salud, debates científicos oportunos [Internet]. Granma [Internet] 2017 [citado: 06/10/2021]; (2): 2-3. Disponible en: Disponible en: https://www.granma.cu/todo-salud/2017-10-06/para-la-salud-dos-debates-cientificos-oportunos-06-10-2017-00-10-23 17. [ Links ]
18. Orraca O, Navarro E, Quintero W, Blanco TM, Rodríguez LR. Frecuencia de infecciones respiratorias agudas en niños y adolescentes con asma de la provincia de Pinar del Río. MEDISAN [Internet]. 2018 [citado: 06/10/2021]; 22(1): 33-9. Disponible en: Disponible en: https://scielo.sld.cu/scielo.php?script=sci-arttext&pid=S1029-30192018000100005&Ing=es 18. [ Links ]
19. Papadopoulos NG, Xepapadaki P. Papel de las infecciones virales en el asma. Salud(i)Ciencia [Internet]. 2017 [citado: 06/10/2021]; 22(6): 545-51. Disponible en: Disponible en: https://www.dx.doi.org/10.21840/siic/75594 19. [ Links ]
20. Licari A, Votto M, Brambilla I, et al. Allergy and asthma in children and adolescent during the COVID-19 ioutbreak: What we know and how we could prevent allergy and asthma flares. Allergy [Internet]. 2020 [citado: 06/10/2021]; 75(9): 2402-5. Disponible en: Disponible en: https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/es/covidwho-276469 20. [ Links ]
21. Hosoki K, Chakraborty A, Sur S. Molecular mechanisms and epidemiology of COVID-19 from an allergist ’ s perspective. J ALLERGY CLIN IMMUNOL [Internet]. 2020 [citado: 06/10/2021]; 146(2): 285-99. Disponible en: Disponible en: https://doi.org/10.1016/j.jaci.2020.05.033 21. [ Links ]
22. OMS. Declaración de la OMS: consumo de tabaco y COVID-19 [Internet]. 2020 [citado: 06/10/2021]. Disponible en: Disponible en: http://www.who.int/es/news/item/11-05-2020-who-statement-tobacco-use-and-covid-19 22. [ Links ]
23. Garufi Giovanna, Carbognin L, Orlandi A, Tortora G BE. Smoking habit and hospitalization for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)- related pneumonia: The unsolved paradox behind the evidence. Eur J Intern Med [Internet]. 2020 [citado: 10/01/2022]; 77(4): 121-2. Disponible en: Disponible en: https://doi.org/10.1016/j.ejim.2020.04.042 23. [ Links ]
24. Fernández Rúa JM. Nueva amenaza del tabaco en pacientes con COVID-19. Biotech Magazine [Internet]. 2021 [citado: 10/01/2022]; 3: 1-3. Disponible en: Disponible en: https://biotechmagazineandnews.com/nueva-amenaza-del-tabaco-en-pacientes-de-covid-19/ 24. [ Links ]
Additional Material
Received: February 25, 2022; Accepted: April 19, 2022











 texto en
texto en 


