Revista de Ciencias Médicas de Pinar del Río
ISSN 1561-3194
01--2023
Articles
Characterization of patients diagnosed with vulvar lichen sclerosus
1"Julio Castillo" University Polyclinic. Chambas.Ciego de Avila. Cuba.
2"Camilo Cienfuegos" University Polyclinic. Chambas. Ciego de Avila. Cuba.
3Faculty of Medical Sciences. Arley Moreira. Morón, Ciego de Avila, Cuba, Cuba.
4"Roberto Rodríguez Fernández" Provincial Teaching Hospital. Morón, Ciego de Ávila, Cuba.
5Policlínico Universitario Sur de Morón, Ciego de Avila, Cuba.
ABSTRACT Introduction: Vulvar lichen sclerosus is a chronic and progressive inflammatory dermatosis, underdiagnosed and undertreated, with a tendency to malignancy. Timely diagnosis and early treatment are essential. Objective: To characterize patients with a diagnosis of vulvar lichen sclerosus attended in the health areas of Chambas municipality, Ciego de Avila. Methods: An observational, descriptive, cross-sectional, case series study was conducted. The sample coincides with the universe so the sampling was intentional non-probabilistic. Women with vulvar lichen sclerosus, treated in Chambas municipality from January 2015 to September 2022, were included, patients with incomplete medical histories were excluded. Absolute and relative frequencies (percentage) were used as a summary measure. Results: There was a predominance of the age group 60-69 years (66,7 %) and white skin color (71,4 %). 52,4 % belonged to the white group. The 52,4 % belonged to the Julio Castillo area. The mean age was 64,8±6,217 years. Vulvar pruritus and hypopigmentation were present in 100 % of the patients. Differentiated vulvar intraepithelial neoplasia developed in 61,9 % of the women. In 48,2 % of the cases the time of evolution was longer than three years. They received surgical treatment 71,4 %. Conclusions: The disease predominated in the elderly; Hypopigmentation and vulvar pruritus were a constant in the patients studied, most developed a differentiated vulvar intraepithelial neoplasia with more than three years of evolution of the lesions and surgical treatment was the most applied behavior.
Key words: VULVAR LICHEN SCLEROSUS; VULVAR PRURITUS; VULVAR NEOPLASMS.
INTRODUCTION
Lichen sclerosus (LS) is a chronic, progressive,1 and multifactorial inflammatory dermatosis of unknown etiology,2 affecting the anogenital region or other part of the body surface.3 It is underdiagnosed and therefore undertreated, so it tends to atrophy, scarring, functional deterioration and risk of malignant evolution, developing a differentiated vulvar intraepithelial neoplasia (VIN) or a spinocellular carcinoma (SCC).4
Francois Hallopeau first described the disease in 1887, as an atrophic form of lichen planus. Ferdinand Darier, five years later, named it lichen planus sclerosus. It received several denominations according to the specialty consulted and in 1976 the International Society of Vulvovaginal Disease adopted the term lichen sclerosus with which this disease is currently recognized.5
The disease is more frequent in childhood and peri- or post-menopause.4,6 The true prevalence is unpredictable because it is under-diagnosed. It is said to be 1 in 300 in adult women and 1 in 900 in girls.6 LE in 85-98 % of cases is located in the anogenital region and only 15-20 % in the extragenital region.6,7
Symptoms include pruritus associated with irritation and tenesmus, dyspareunia, dysuria and anal symptoms.4,7 The cutaneous picture is characterized by papules or maculo-papules, flat, depressed with atrophy, fragility, excoriations and lichenification with edema of the labia minora; telangiectasias and purpura. In final stages, the labia majora and labia minora are sealed with partial or total occlusion of the vaginal introitus.4,7
Considering the repercussions of this entity on skin, urinary and sexual health, as well as the potential risk of developing a differentiated VIN or CEC if not diagnosed and treated early, the interest arises to conduct the present research, with the aim of characterizing patients diagnosed with vulvar lichen sclerosus.
METHODS
An observational, descriptive, cross-sectional, cross-sectional, case series study was carried out on patients with a diagnosis of vulvar lichen sclerosus attended in dermatology and/or gynecology consultations belonging to the health areas of the municipality of Chambas, Ciego de Avila, in the period from January 2015 to September 2022.
The universe was constituted by all the patients attended in the place and period mentioned above (n=21). The sample coincides with the universe so the sampling was non-probabilistic of intentional type. The following inclusion and exclusion criteria were considered.
Inclusion criteria
Female population with a diagnosis of vulvar lichen sclerosus, who were attended in the health areas of the municipality of Chambas during the established period of time.
Exclusion criteria
Patients with incomplete clinical histories.
The following variables were taken into account: age group; skin color; health area; symptomatology; physical examination findings; tendency to malignancy, according to histopathological study; time of evolution of the lesions, taking into account the time elapsed from the onset of symptoms to diagnosis and treatment received.
Methods of obtaining information
The necessary information was collected from the individual clinical histories of the patients, using a data collection instrument created for this purpose by the authors of the research with the objective of organizing the variables to be analyzed, being the result of a correct anamnesis and physical examination of the patients, in adequate conditions of hygiene and illumination.
Statistical processing
The results were entered into a Microsoft Excel database, which was processed in the SPSS 18.0 statistical package for Windows. Descriptive statistics were used. Absolute frequencies, relative percentages, and measures of central tendency and dispersion (mean, median, mode and standard deviation) were used to summarize the information.
Ethical considerations
The research was approved by the institution's Scientific and Ethics Council. It complied with the principles of medical ethics and the aspects established in the Declaration of Helsinki.8
RESULTS
There was a predominance of the 60 to 69 years age group with 14 patients representing 66,7 %, those with white skin color (71,4 %), and those belonging to the Julio Castillo health area (52,4 %). The mean age was 64,8±6,217 years (Table 1).
Table 1 Distribution of patients diagnosed with vulvar lichen sclerosus according to age group, skin color and health area to which they belonged.
| Variables | N (%) | |
|---|---|---|
| Age group | ||
| 50-59 | 3(14,3) | |
| 60-69 | 14(66,7) | |
| 70 y más | 4(19,0) | |
| Mean: 64.8 Median: 65 Mode: 67 Standard Deviation: 6,217 | ||
| Skin | ||
| White | 15(71,4) | |
| black | 4(19,0) | |
| Mestizo | 2(9,5) | |
| Healthcare | ||
| Polyclinic Julio Castillo | 11(52,4) | |
| Polyclinic Camilo Cienfuegos | 5(23,8) | |
| Polyclinic Máximo Gómez | 5(23,8) | |
Source. Medical records
About 100 % of the patients presented symptoms of vulvar pruritus and hypopigmentation as physical examination findings. The most affected age group was 60 to 69 years old (Table 2).
Table 2 Distribution of patients according to symptomatology, findings on physical examination and age group.
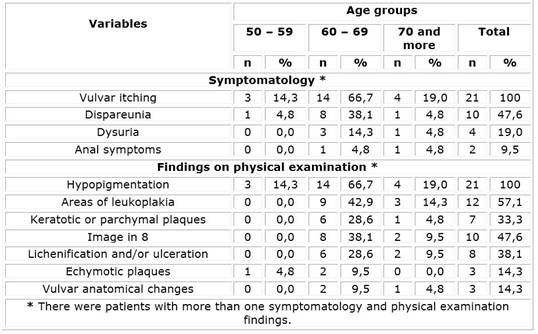
Source. Medical records
It was observed that 61,9 % of the women developed a differentiated vulvar intraepithelial neoplasia. (Table 3).
Table 3 Distribution of patients according to tendency to malignization of the lesions
| Malignant tendency | Frequency | ||
|---|---|---|---|
| n | % | ||
| Differentiated vulvar intraepithelial neoplasia | 13 | 61,9 | |
| Spinocellular carcinoma of the vulva | 2 | 9,5 | |
| Lichen sclerosus without malignancy | 6 | 28,6 | |
Source. Medical records
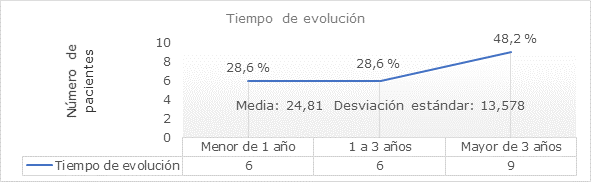
About 48,2 % of patients presented more than 3 years of lesion evolution. The mean time of evolution of the lesions was 24,81±13,578 months (Figure 1).
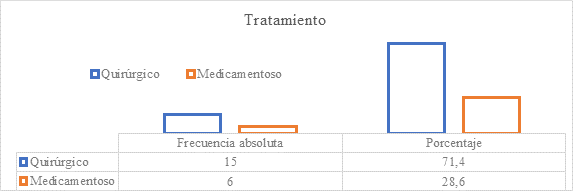
Fifteen patients received surgical treatment, representing 62,5 %. (Graph 2)
DISCUSSION
LE has two peaks of incidence in prepubertal girls and in perimenopausal or postmenopausal women.4,9) It occurs in 10 % to 15 % in prepubertal patients.3,9) In this study, the women treated with LE are older than 50 years, with a predominance between 60 and 69 years of age, a fact that coincides with the literature consulted.
Of the three health areas that make up the municipality of Chambas, the highest incidence of the disease occurred in the Julio Castillo health area, as it is the area with the largest population.
The disease has a higher incidence in white-skinned women,1,4,7) as was the case in this study. In a study carried out in Brazil by Castro do Rego Barros,10) 83,1 % of LE predominated in black women, due to the fact that the research was carried out in an area with an Afro-American population.
It is described that vulvar pruritus and hypopigmentation of the genital area are a constant in most patients.4,7,10) Cabrera-Acea G et al.,11) found that the clinical aspects of LE are diverse, but the predominant symptom is a pruritus of variable intensity, intermittent or permanent, at vulvar and/or perianal level. Barchino Ortiz L,12) found pruritus as the predominant symptom in 85,9 % of patients, followed by itching, dyspareunia, pain and presence of fissures. This fact coincides with the present investigation where pruritus is a constant symptom followed by dyspareunia.
The most frequent cardinal sign in this disease is hypopigmentation, followed by leukoplakia plaque, as described by Cortés-Ros O et al.13) and Cabrera-Acea G et al.,11) in their respective investigations, which coincides with this study. Another research that yields similar results is the Doctoral Thesis of Barchino Ortiz L,12) where pearly-white plaques predominated (93,39 %).
LE appears to be an independent promoter of human papillomavirus (HPV) for carcinogenesis, which corroborates its potential for malignant degeneration,14,15) hence the importance of long-term follow-up of these patients.15)
Gutiérrez-Pascual M et al,16) refer to the relationship of differentiated VIN with genital CEC. Both are entities highly linked to genital LE and independent of HPV infection. In addition, oncogenic molecular alterations independent of HPV infection have been demonstrated that could explain the malignant potential of LE itself.
Differentiated VIN is not causally related to HPV, this entity is associated with chronic inflammatory dermatoses such as lichen sclerosus and lichen simplex chronicus. Immunosuppression, advanced age and chronicity of lesions are associated with an increased risk of progression to CEC vulva.17,18,19) Falcón M F et al,17) agree that differentiated VIN occurs in postmenopausal women and is usually associated with lichen sclerosus.
All of the above discussed corresponds to what was found in this investigation where 61,9 % of the women with a diagnosis of vulvar LE developed a differentiated VIN.
The association between genital LE and CEC is widely documented in the literature, the estimated risk is 5 % of the cases, mainly in those of long evolution,16,17) in the present investigation most of the women had a period of more than three years of evolution of the disease, which is considered to be related to the development of malignant processes.
The use of high potency steroids, such as clobetasol propionate 0,05 % is considered first line treatment.14,20) In refractory cases methotrexate, cyclosporine and other immunosuppressants are used. Physical therapy is applied in cases of malignization or scar sequelae.10) Cabrera-Acea G et al.,11) presented a case with LE, successfully treated with high potency local steroids, conjugated estrogens and psychological support.
Surgery remains the first-line therapy in the face of the development of a differentiated VIN, a CEC and to correct scar defects that severely interfere with the patients' quality of life.14,16
In the present investigation the highest percentage of patients underwent surgical treatment because of the tendency of the lesions to malignize, which was in correspondence with the late diagnosis of the disease and the absence of treatment.
It is not possible to say whether medical treatment can prevent progression to malignization, but early diagnosis and initiation of treatment of these patients could not only reverse the lesions and reduce the rate of malignant transformation, but also prevent scarring and long-term sequelae. The present research is one of the outputs of an Institutional Project entitled: Predictive factors of malignant transformation in vulvar lichen sclerosus.
Being an infrequent pathology, a limitation of the study was the small size of the universe, which prevents the extrapolation of the results with other investigations.
The highest frequency of vulvar lichen sclerosus was in elderly patients, white and belonging to the Julio Castillo health area; hypopigmentation and vulvar pruritus were a constant in the patients studied, most of them developed a differentiated vulvar intraepithelial neoplasia with more than three years of evolution of the lesions and surgical treatment was the most applied conduct.
BIBLIOGRAPHIC REFERENCES
1. Torres M, Dubeibe P, Pareja M. UVA-1 phototherapy for the treatment of genital lichen sclerosus. Dermatol Rev Mex [Internet]. 2021 [citado 12/04/2022]; 65(2): 159-165. Disponible en: Disponible en: https://dermatologiarevistamexicana.org.mx/article/fototerapia-uva-1-en-el-tratamiento-del-liquen-escleroso-y-atrofico-vulvar/ 1. [ Links ]
2. Gómez Chaves G, Sequeira Araya A, Rodríguez Vega MF. Actualización en liquen escleroso vulvar en población adulta. Rev.Méd.Sinerg [Internet]. 2022 [citado 12/04/2022]; 7(8): e853. Disponible en: Disponible en: https://revistamedicasinergia.com/index.php/rms/article/view/853 2. [ Links ]
3. Macías Yanes JC, Trujillo Betancourt M, Galván Sánchez L, Leonard Díaz D, Estrada Sánchez T, Leyva Almeida H. Liquen escleroso atrófico con vitiligo en pediatría. Rev. Finlay [Internet]. 2021 [citado 12/09/22]; 11(1): 59-65. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2221-24342021000100059 3. [ Links ]
4. Rucci-Bentancor N. Monografía: Manejo terapéutico del Liquen Escleroso vulvar [Internet]. Uruguay. Facultad de Medicina de la República Oriental del Uruguay; 2018 [citado 26/03/2021]. Disponible en: Disponible en: https://www.ginecotocologicab.hc.edu.uy/images/Monograf%C3%ADa_Liquen.pdf 4. [ Links ]
5. Arias Florez F, Sehtman A, Navajas D, Allevato M. Liquen Escleroso. Dermatol Argent [Internet]. 2016 [citado: 26/03/2021]; 22(1): 05-12. Disponible en: https://www.dermatlolarg.org.ar/index.php/dermatolarg/article/view/1466 [ Links ]
6. Caussade A. Liquen escleroso: actualización. Archivos de Ginecología y Obstetricia [Internet]. 2019 [citado 26/03/2021]; 57(1): 31-54. Disponible en: Disponible en: https://ago.uy/publicación/1/numeros/6/article/liquen-escleroso-actualización-lichen-sclerosus-an-update 6. [ Links ]
7. Cararach M, Castro M, García A, Juliá M, Mascaró JM, Quílez JC, et al. AEPCC-Guía: Dermatosis inflamatoria de la vulva (liquen escleroso, liquen plano y liquen simple crónico) [Internet]. Publicaciones AEPCC; 2016 [citado 26/03/2021]. p.1-52. Disponible en: Disponible en: https://www.aepcc.org/wp-content/uploads/2016/12/AEPCC_revista06-DermatosisInfVulv.pdf 7. [ Links ]
8. Asociación Médica Mundial. Declaración de Helsinki de la AMM. Principios éticos para las investigaciones médicas en seres humanos. Ratificada en la 64ª Asamblea General, Fortaleza, Brasil, octubre 2013 [Internet]. Helsinki: 18ª Asamblea Mundial; 1964 [citado: 26/02/2022]. Disponible en: Disponible en: https://www.wma.net/es/policies-post/declaracion-de-helsinki-de-la-amm-principios-eticos-para-las-investigaciones-medicas-en-seres-humanos/ 8. [ Links ]
9. Singh N, Ghatage P. Etiología, características clínicas y diagnóstico del liquen escleroso vulvar: una revisión de alcance. Obstet Gynecol Int [Internet]. 2020 [citado 26/02/2022]; 2020(7480754). Disponible en: Disponible en: https://www.hindawi.com/journals/ogi/2020/7480754/ 9. [ Links ]
10. Castro do Rêgo Barros C. Aspectos clínicos e epidemiológicos de mulheres com líquen escleroso atendidas no Hospital das Clínicas [Internet]. Brasil: Universidade Federal de Pernambuco. Recife; 2019 [citado: 26/02/2022]. Disponible en: Disponible en: https://repositorio.ufpe.br/bitstream/123456789/35344/1/DISSERTA%c3%87%c3%83O%20Cl%c3%a1udia%20Renata%20Castro%20do%20R%c3%aago%20Barros%20Albuquerque.pdf 10. [ Links ]
11. Cabrera-Acea G, Hernández-Mompié J, Gómez-Cabrera C. Liquen escleroso y atrófico genital o craurosis de la vulva. Presentación de un caso. Medisur [Internet]. 2016 [citado 26/03/2021]; 14(6): 796-800. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2016000600018 11. [ Links ]
12. Barchino Ortiz L. Liquen escleroso vulvar: estudio descriptivo epidemiológico, clínico e histológico de las pacientes de una consulta monográfica de dermatología ginecológica. [Tesis Doctoral]. Madrid: Universidad Complutense de Madrid. Facultad de Medicina; 2021 [citado 26/02/2022]. Disponible en: Disponible en: https://eprints.ucm.es/id/eprint/67462/1/T42812.pdf 12. [ Links ]
13. Cortés Ros O, Matos Figueredo F, Gahona Kross T, Villacrés Medina L. Liquen escleroso atrófico genital y extragenital diseminado. Presentación de un caso. Medisur [Internet]. 2013 [citado: 26/03/2021]; 11(6): 685-689. Disponible en: Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2013000600010&lng=es 13. [ Links ]
14. Hinojal Toscano I, Zamorano Alanís B, Martínez Maestre M. Revisión del tratamiento actual del liquen escleroso vulvar. Arch Inv Mat Inf [Internet]. 2020 [citado: 26/03/2021]; 11(2): 82-90. Disponible en: Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=101555 14. [ Links ]
15. Manzo-Carrillo L, Ramírez-Fuentes K, Cabrera-Rivero KE. Liquen escleroso y atrófico asociado a cáncer vulvar (Carcinoma epidermoide moderadamente diferenciado, ulcerado e invasor de clítoris). Congreso Mexicano de Obstetricia y Ginecolóógía, Guadalajara; 2022 [citado: 26/02/2022]. Disponible en: Disponible en: https://femecog.org.mx/categoria5/CC-88.pdf 15. [ Links ]
16. Gutiérrez-Pascual M, Vicente-Martín FJ, López-Estebaranz JL. Liquen escleroso y carcinoma escamoso. Actas Dermo-Sifiliográficas [Internet]. 2012 [citado: 26/03/2021]; 103(1): 21-28. Disponible en: Disponible en: https://www.actasdermo.org/es-liquen-escleroso-carcinoma-escamoso-articulo-S0001731011002857 16. [ Links ]
17. Falcón MF, Paradeda ME, García KF, Maldonado V, Díaz L, Cardinal L. Inmunohistoquímica de p16 y p53 en cáncer de vulva. Medicina (B. Aires) [Internet]. 2020 [citado 26/03/2021]; 80(2): 127-133. Disponible en: Disponible en: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802020000300005&lng=es 17. . [ Links ]
18. Reolid PA, Muñoz AE, Rodríguez JP, Llamas MM, Gordillo C, Daudén E. Asociación del virus del papiloma humano tipo 6 con liquen escleroso hipertrófico. Med Cut Ibero-Latino-Am [Internet]. 2018 [citado 27/04/2021]; 46(1): 56-58. Disponible en:Disponible en:https://www.medigraphic.com/pdfs/cutanea/mc-2018/mc181k.pdf 18. [ Links ]
19. Vieira-Baptista P, Pérez-López FR, López-Baena MT, Stockdale CK, Preti M, Bornstein J. Riesgo de desarrollo de cáncer de vulva en mujeres con liquen escleroso o liquen plano: una revisión sistemática. J Enfermedad del tracto genital inferior [Internet]. 2022 [citado 27/04/2021]; 26(3): 250-257. Disponible en: Disponible en: http://journals.lww.com/jlgtd/fulltext/2022/07000/risk_of_development_of_vulvar_cancer_in_woman_with.9.aspx 19. [ Links ]
20. Álvarez Gil C, Sanz Baro R, Blanco Herraez I, Ferreira Borrego IM, Pineda Domínguez L, Redondo Guisasola C. Neoplasia intraepitelial vulvar: Cribado en población de riesgo. Clínica e Investigación en Ginecología y Obstetricia [Internet]. 2021 [citado 27/04/2021]; 48(2): 117-121. Disponible en: Disponible en: https://www.sciencedirect.com/science/article/abs/pii/S0210573X20301088 20. [ Links ]