Introduction
Mortality and morbidity due to infectious causes have decreased in spite of the re-emergent illnesses. There is an epidemiological transition in which the non-communicable diseases (NCDs) are the more frequent causes with a great impact on sanitary costs, disability and premature death. There is a marked evidence in developing countries due to inadequate lifestyles that have suffered a double burden of infectious and NCDs.1
The surveillance of NCDs has become a strategic need for the health systems, among them the CKD for their high human and social costs and the financial costs for the health systems. The CKD can be detected in the clinical practice with a simple analysis of urine, the presence of microalbuminuria, and the calculation of the glomerular filtration rate (GFR) by means of equations using the serum creatinine.2
The investigation in Cuban Health Services and Systems has the purpose to “increase the capacity for resolution and the excellence of the services depending on the development of science"3, Internationally, it is demanded to make them to improve the efficiency of the sanitary systems4, in accordance with the Strategy for Universal Health of the World Health Organization/Pan-American Health Organization (WHO/PAHO), reference for the equal access to health and quality, which is focused on people and the communities, like a contribution of health to the sustainable human development".5
CKD can be suffered by 10% of the adult population and it is recognized recently by the WHO like an illness of high epidemic impact, one of the main NCDs, and with more growth during the last years5, with evident influences on global mortality.6
There are evidences of the close biological and clinical relationship between CKD and cardiovascular diseases (CVD) that demonstrate how the early interventions directed to control the common risk factors to both of them, decrease the risks of CVD mortality and renal failure with dialysis requirements, kidney transplant, and costs.7 This explains the necessary early detection and the indispensable collaboration between Nephrology and Primary Health Care (PHC).
The basis of the NHS in Cuba lies in the PHC and the "dispensarization" process (registration, risk assessment, treatment, and patients' follow-up); it is the center for the individual´s ambulatory care in the community, which is carried out by the family doctor.
In 2011, the informatics system for the registration of the primary data was updated and improved by the National Direction of Statistical of the Ministry of Public Health; the information system of CKD (GFR <60 ml/min/m2) was extended, and a new information registry of CKD patients with Diabetes Mellitus in the PHC was added.8
In Cuba, the prevalence of CKD patients registered in the PHC was 2.16 per 1 000 inhabitants and the prevalence of CKD patients with Diabetes Mellitus was 0.48 per 1 000 inhabitants in 2015.9
The objective of this research is to evaluate and compare the “dispensarization” of CKD patients and CKD patients with Diabetes Mellitus between 2014 and 2017 as expression of the quality and acting of the National Health System (NHS) in general and the PHC in particular, as well as to establish considerations on the technological tools for its diagnosis and available treatment in our country.
Material and Methods
This report includes national data of the registered CKD patients and CKD patients with Diabetes Mellitus in the PHC in our country. The data source is the Registry of “dispensarized” patients in the PHC in the National Direction for Statistics of the Ministry of Public Health.
The analyzed variables were the groups of ages, gender, prevalence of CKD patients, and prevalence of CKD patients with Diabetes Mellitus.
The validation of the primary data of dispensarized patients was made by the Statistical Department of each polyclinic (Health Area) by means of the revision of the clinical records at the family doctor’s office, which are integrated to the polyclinic (verified mistakes, duplicities, inconsistencies), municipalities, provinces and at national level. In each level those consolidated data undergo validations. The results are expressed in measures of frequency and rates per 1 000 inhabitants.
The dispensarization respects the patient's privacy and it is sustained in the bioethical principles accepted in our society.
Definitions
CKD is defined by the presence of structural or functional abnormalities of the kidney, with or without decrease of the GFR, manifested by pathological alterations or markers of renal damage (alterations in the composition of the blood or the urine, or alterations in the renal images), for more than 3 months and with implications for health. Their causes can be distinguished as non-diabetic, diabetic or secondary to a renal transplant.
The earliest stages of CKD (stages 1 and 2), are the most important in face of the absence of significant alteration of the serum creatinine in spite of the risk of renal dysfunction. These stages are identified by the presence of abnormalities in the urine, albuminuria or hematuria of glomerular origin. The most advanced stages belong to rates of having decreased GFR <60 ml/minute/m2. For the stage CKD-3a, the GFR is 59-45 ml/minute/m2; for the CKD-3b, the GFR is 44-30 ml/minute/ m2); for the stage CKD-4, the GFR is 29-15 ml/minute/m2; and for the stage CKD-5, the GFR is <15 ml/minute/m2, and it corresponds to the necessity of methods of renal replacement therapy of renal function (hemodialysis, peritoneal dialysis, kidney transplant) or cares at the end of life.
The calculation of the GFR <60 ml/minute/1,73 m2 is made by means of a simple mathematical formula; the Cockroft-Gault formula; which is adjusted according to corporal surface, (140-age [years] x weight [kilograms] / serum creatinine (mg/dl) x 72 [x 0.85 in women]. If the serum creatinine is measured at the laboratory by micromol/l it is divided between 88.4 for its conversion in mg/dl). There is international consensus for the employment of several formulas to calculate the GFR.10,11
The GFR<60 mL/min/1.73 m2 is related to, at least, the loss of more than one half of the adult's normal renal function. From this level of GFR, the complications of CKD are increased(1) and in our country those patients are registered in the PHC, under the terminology of “chronic renal failure”.
CKD patients with diabetes mellitus follow the same mentioned classification.
We consider to accept the year 2014 as the “baseline”, starting with this methodology for its registration.
Results
The summary of the Cuban population data in 2017 according to Dispensarial Groups, shows that 17,6% corresponds to supposedly healthy persons (Group-1), persons with risk 36.9% (Group-2), sick persons 42,3% (Group-3) and persons with sequel 3,2% (Group-4). The CKD patients and CKD patients with Diabetes Mellitus belongs to Group 3.
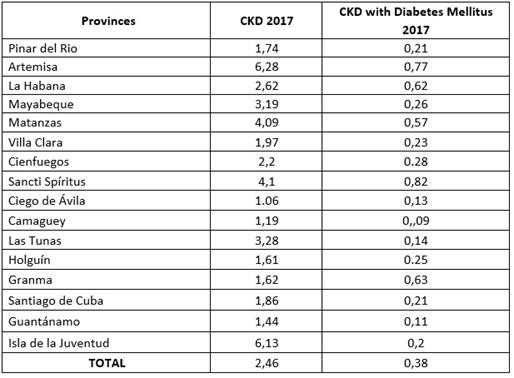
The number of dispensarized patients increased in 2017 in comparison with 2014 of the total prevalence of CKD patients (21%), but the total prevalence of the CKD patients with Diabetes Mellitus increased 47,21%, without appreciable differences according to sex. (Table 1).
Table 1: Dispensarized patients with CKD (GFR<60ml/minute/m2), and of them CKD patients with Diabetes Mellitus
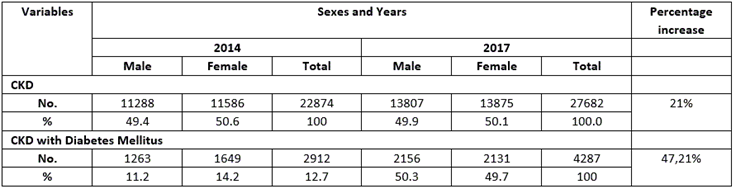
Table 2 shows the progressive increased prevalence of CKD patients and the prevalence of CKD patients with Diabetes Mellitus according to the elderly ages. There is not important increase at pediatric ages regarding the prevalence of CKD patients and the prevalence of CKD patients with Diabetes Mellitus.
There was an increase regarding adult patients from the 19 years; among 25-59 years the prevalence of CKD patients has also increased 6,2% as well as the prevalence of CKD with Diabetes Mellitus which increased 31.0%.
The prevalence of CKD patients from 60 to 64 years reached the maximum rate 8.99 per 1 000 inhabitants, (With regard to 2014, the increase was 17,98%). The prevalence of CKD patients with Diabetes Mellitus was 1.32 per 1 000 inhabitants (An increase of 21,7% with regard to 2014).
The prevalence of CKD patients older than 65 years reached a rate of 7.5 per 1 000 inhabitants, (Increase of 25.42% with regard to the year 2014); and for the prevalence of CKD patients with diabetes mellitus, the prevalence was 1.35 per 1 000 inhabitants (Increase of 53,4% with regard to the year 2014).
Table 2: Prevalence Rates of dispensarized patients per 1 000 inhabitants with CKD (GFR<60ml/minute/m2),

Note: the main percentages increases are in parentheses.
In the period 2010-2015, the purposes and guidelines of the Cuban Public Health were to reach a dispensarization rate of CKD patient (GFT<60ml/min/m2) of 1.74 per 1 000 inhabitants. The dispensarization increased in all provinces as well as in the Special Municipality of Isla de la Juventud at the end of 2017; 68,8% of them reached the previous rate.
There was a variation among the provinces for the prevalence rate, the prevalence of CKD patients was: maximum 6.28 per 1000 inhabitants, and minimum 1.06; and the prevalence of CKD patients with Diabetes Mellitus (maximum of 0.82, minimum of 0,11) (Table 3).
After the analysis of the percentage of CKD patients with Diabetes Mellitus vs the diabetic population of each territory, a similar variation is appreciated among different provinces: CKD patients with Diabetes Mellitus (maximum of 1.25%, minimum of 0.1%)
Discussion
It has been demonstrated that the NCDs, represent a global health problem, which was recently recognized in the official documents of the WHO/PAHO.2,5
NCDs associated to vascular damage, (cardiovascular disease, diabetes mellitus, cerebral vascular disease or peripheral vascular disease, and the CKD) are “specific organs” for their onset, but they are considered systemic diseases; therefore, other systemic damages may be detected in patients who have suffered heart or kidney damage. Also, these different organs are affected by similar risk factors (hypertension, diabetes, hyperlipidemia, obesity, tobacco), all of them are modifiable risk factors.1,12
Therefore, health surveillance on NCDs is important in order to know the burden of these diseases and in case of CKD, to carry out its early detection to apply the effective treatments and avoid its progression to stage 5 of kidney failure. This is the main objective of the national and international strategic actions in order to avoid this epidemic at the PHC. 13,14,15,16
The Ausdiab Study, (Australia), regarding CKD, diabetes, obesity and lifestyle found a prevalence of GFR <60 ml/min of 11,2%.17
In the United States, according to the surveillance of CKD and other illnesses through the National Health and Nutrition Examination Survey (NHANES), an increase of 14,5% to 16,8%. during the period 1999-2004 compared with 1988-1994, was demonstrated in adults older than 20 years. It is detected with more frequency in women; it increases with age (mainly ( 60 years old: 40%; and the main etiological cause is the diabetes (40 to 55% of the patients), followed by hypertension (15 to 30%).18
The Spanish epidemiological study of the CKD points out the epidemic increase of obesity, with its two main consequences: type 2 diabetes and arterial hypertension, which are the determinant ones, together with the population aging of the growing prevalence of CKD and the diabetic kidney disease, and finds the CKD-DM as the first etiological cause.19
The results of our studies with selected populations are according to these studies, but less women with CKD are detected, as well as less diabetic patients with CKD.
Since 2014, the guidelines of the European Society of Cardiology defined CKD as an independent risk factor for coronary events; either in diabetics or in non- diabetics. CKD is associated to mortality and progression to renal failure.15,18,20
On the other hand, the presence of advanced CKD increases the economic costs to a 195%, and in the stage using dialysis methods it reaches 771%21 it was ratified in 2014 by the consensus conference of the American Association of Diabetes.7
CKD at any stages, constitutes an independent risk factor for higher cardiovascular morbidity and mortality recognized since 2003 in the VII Report of the National Joint Committee; in definitions of the American Heart Association; by Go et. al, (2004) in which more than 1.1 million adults were studied, and in 2008 when a re-analysis of the Framingham study was made.22,23,24
There are some limitations for the early diagnosis of CKD, one of them is the limited evaluation of the serum creatinine level due to its low sensibility as a marker for renal dysfunction and the need of its use for calculating the GFT. There are other problems such as the lack of serum creatinine standardization in the laboratories; the report of calculation of the GFR has not been stablished in the laboratories, there is no application of the current guidelines, and the need of applying mathematical formulas for calculating the GFT is unknown by some medical doctors.10,11
The Cockcroft and Gault formula for calculating GFR is the easiest and more extended formula in Cuba, but it is influenced by the advanced age, gender, race, weight, diet, employment of some drugs and used laboratory methods, that’s why it is not the most recommended one, but, its simplicity to be used by medical doctors with a simple calculator allows it to be a plausible option.10,11
Applications for cellular phones allow the professionals to use formulas of higher degree of precision and predictive power for cardiovascular events and progression to end stage renal disease25. It is possible to consult the Cuban software developed by Professor Mañalich and collaborators through the search in the web page of Nephrology which is available at INFOMED.
The community projection of nephrologist care and the reference against reference of our Unique Health System guarantees to consult with a Nephrologist for a second option.
The other element for the early diagnosis of CKD and the risk stratification is the microalbuminuria. The magnitude of it presence and the deterioration of the GFR predict not only the evolution of the GKD, but also its complications.26,27
The presence of microalbuminuria is also a marker of inflammatory endothelial damage, it also announces some possible cardio-cerebrovascular events for which it should be used at the PHC.28 It is also recommended to measure the albumin/creatinine index (ACI) and protein/creatinine index (PCI) with a unique sample of urine, which is very important for the prognosis.29
Cuba has laboratory equipment of national production that guarantee the measurement of microalbuminuria in the PHC, and it has also standardized both tests, the ACI and the PCI in urine.
The analysis of this Investigation in Systems and Services of Health, from the family doctor´s office to the province, will allow to improve the mangement for the diagnosis and appropriate treatment of the CKD5.
The use of both diagnostic tools as well as non-complex interventions, like strict control of the glycemia (HbA1c between 6,5-7,5%) in diabetics, control of the high arterial pressure (130/80 mm Hg) and of the proteinuria using angiotensin-converting enzyme inhibitors (ACEI) drugs to full dose, as well as the early remission to the nephrologist, has been recognized internationaly.30,31
In relation to the cardio-nephrology preventive therapies, the scientific evidences demonstrate that an appropriate control of the hypertension, the dyslipidemia, the glycemia in diabetics, an appropriate diet, together with favorable changes in the lifestyles and reduction of the body weight in obesity patients, are beneficial to reduce the progression of diabetic CKD and non-diabetic CKD for the reduction of the mortality due to cardiovascular cause.32,33,34,35
Cuba has the main groups cardio-renal protection medications for the control of the risk factors and the illnesses that cause CKD and its progression to more advanced stages, and a national politics of medications that guarantees them. At the same time Nephrology as a specialty has a clear strategy and works on the appropriate management of the CKD and its progression factors by means of multiples interventions from the PHC.12,36,37
The “family doctor” institution settles at the community where each patient lives for the development of its preventive-healing activities in connection with the other levels of the NHS. The glucometer for monitoring the periodic level of glycemia as a complement of the medical care is also guaranteed to each diabetic patient.
In 2011 the III National Survey of Risk Factors was carried out in Cuba, as part of the health surveillance in NCDs, a probabilistic sample of 4 150 adults of the total Cuban population was studied. The renal profile of the survey, has shown the necessary information of the possible prevalence of CKD with none hospitalized adults.
A unique blood sample for creatinine was studied, and the GFR was calculated according to the MDRD formula, in order to know the prevalence and the stratification of the renal damage. CKD (Chronic Renal Failure) was defined as a high presumption diagnosis for persons with a GFR <60 ml/minute/1.73 m2; it was demonstrated that the 5.2% of the population was at risk of suffering it, according to epidemic elements and traditional risk factors that cause it and for the diabetics in 13.2%, it is predominant in the female sex.38
This research paper points out a low number of registered patients of CKD and CKD with Diabetes Mellitus in the PHC as one of the main limitations, compared with the estimated number of CKD patients as results of the III National Survey of Risk Factors and the international reports.
Our NHS, resilient, compromised with the universal sanitary covering and the inclusion of the health in the Calendar of Development in accordance with the WHO, has as final objective to decrease the mortality for NCD in 25% for the year 2025, at the stage of transformations with the purpose of improving the population's health and maintaining the quality of the services, it has much in common with the “Pattern of Integrated Chronic Cares” as innovative strategy, centered in the patient and praised by the PAHO/WHO.39
The PHC, through the management of the “Basic Group of Work” and family doctors, can contribute to avoid the appearance of the risk factors of NCDs with strategies of health promotion and the participation of the community, they can also modify or identify and treat in a proactive way for an early detection and treatment of the patients, by means of interventions to the high risk, subclinical, or dispensarized patients with strategies that have demonstrated to be effective.
Cuba has integrated the National Commissions for Prevention of NCDs, at national and provincial level, among them the National Commission for the Prevention of CKD, has been working for more than 30 years, which is claimed internationally as a strategy, and it was only approved in Spain in 2015.40
Conclusions
An improvement is observed in the dispensarization of patients suffering from CKD, especially for CKD with Diabetes Mellitus.
The guarantee of the sustainability is sustained by the advice given to the community and the patients; the low-cost diagnostic tests (microalbuminuria and creatinine to calculate the GFR); the interest of the State to guarantee the necessary medications; and in the organizational thing, by the dispensarization and the analysis of the health care of each community for the improvement and certification process and the permanent training by Nephrology to the doctors of the PHC, and also at secondary and tertiary levels.