Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Podium. Revista de Ciencia y Tecnología en la Cultura Física
versión On-line ISSN 1996-2452
Rev Podium vol.18 no.1 Pinar del Río ene.-abr. 2023 Epub 07-Abr-2023
Original article
Impact of physical exercises in the rehabilitation of patients with incomplete cervical spinal cord injuries, in Guinea-Bissau
1Universidad de Ciencias de la Cultura Física y Deporte "Manuel Fajardo". La Habana, Cuba.
People with cervical spinal cord injuries are two to five times more likely to die prematurely, these injuries are one of the most frequent causes of death in the world population regardless of religion, age, race, sex, nationality or social class; the lowest survival rates are found in low- and middle-income countries. In Guinea-Bissau, patients are unaware of their illness and the benefits of physical activity for their treatment; for this reason, a study was carried out with ten patients who attend the area of Motor Neuro-rehabilitation, Bissau, where the objective was: to determine the impact of physical exercises on the rehabilitation of patients with incomplete cervical spinal cord injury. Qualitative (documentary review) and quantitative (measurement) and expert criteria methods were used, which allowed the study of the object and the theoretical and practical evaluation of the physical exercises, which were validated by 17 experts, among whom 95% they evaluated the indicators as adequate and very adequate and it was applied in practice to ten patients with very satisfactory results, which confirmed the relevance of the study carried out. 100% of the participants reached a significant level in activities of daily living, physical and functional capacities. This study responded to the research needs of the "Manuel Fajardo" University of Physical Culture and Sports Sciences, of Cuba and the Sanca Neuro - Physical Motor Rehabilitation Center, of Guinea-Bissau.
Keywords: physical exercises; incomplete cervical spinal cord injury; physical rehabilitation.
INTRODUCTION
Traumatic spinal cord injury can affect all functions of the spinal cord, leading to activity limitations and participation restrictions. Knowing one's own epidemiological profile is imperative to plan care, resources and act in prevention (Arriola et al., 2021 and Silva, 2021). In addition, it can lead to a spectrum of neurological problems that includes loss of motor and sensory function, bladder and bowel dysfunction, spasticity, neuropathic pain and autonomic dysreflexia and impacts in the family and in society with high care requirements in the short and long term (specialized human resources, long treatment times) and high direct and indirect costs.
Spinal cord injury affects a small but significant part of the population. Reviewing all causes of disability in the US from 1976-1980, it was found that the rate of spinal cord injuries was 17 per 100,000 population with an average age of 12-42 years and approximately 10,000 new spinal cord injuries occur usually every year (Echemendía, 2021).
The treatment is based on the coordination of a group of specialized professionals: doctors, nurses and health professionals among which physical rehabilitation specialists stand out, headed by Graduates in Physical Culture and Rehabilitation Technicians. They provide optimal care, thanks to the experience gained in specialized centers. These groups of trained personnel are committed to providing continuity of care from the scene of the accident and throughout the life of the spinal cord injured person.
The elements of this therapeutic approach are based on prevention, pre-hospital care, acute care, rehabilitation and lifelong medical follow-up (Miller et al., 2016). Although in recent years it has been the focus of study with technological advances, such as nanotechnology or robotics and scientific advances, such as the application of stem cells with great results in the reconstruction of nervous tissue (Chasman et al., 2019).
In neuro-rehabilitation, gait training in spinal cord injuries is adapted to the existing residual musculature, so that the type of gait to be achieved, the orthoses and technical aids for gait (walker or Canadian canes) depend on the strength present in different muscle groups. Physical work is aimed at working or re-educating the muscles that determine gait; that is, to maintain or release joint arches, to strengthen the muscles, to control high tone and to re-educate coordination and balance. At the same time that gait determinants are specifically worked on, compensation strategies are developed that facilitate movement based on limitations (Echemendía, 2021).
The main objective of rehabilitation in the spinal cord injury is to provide all the tools to the patient to achieve maximum independence based on their neurological injury, age and co-morbidity. The other great objective is the reintegration of the patient into the family, social and work environment (Battler et al., 2021).
To distinguish between the different disabilities, the ASIA Assessment Scale is generally used, which is applied based on the absence or presence of motor and sensory function.
Complete lesion A: Absence of motor and sensory function extending to sacral segments S4-S5.
Incomplete injury B: preservation of sensory function below the neurological level of the lesion extending to sacral segments S4-S5 and with absence of motor function.
Incomplete injury C: preservation of motor function below the neurological level and more than half of the key muscles below the neurological level have a muscle balance of less than 3.
Incomplete injury D: Preservation of motor function below the neurological level and more than half of the key muscles below the neurological level have a muscle balance of 3 or greater.
Normal E: sensory and motor functions are normal.
In the results of its international application, a greater predominance of grade A lesions is observed, followed by those of grade B and C and less frequently those of grade D and E (Hernández, Rodríguez, 2014).
Studies carried out in 2015 by the World Health Organization in Guinea-Bissau determined that 60 % of spinal cord injury patients are young, 40 % of them were affected with cervical spinal cord injuries and 95 % were due to traumatic causes, who have not been able to return to their social activities, due to a long recovery period that, on many occasions and for dissimilar reasons, is incomplete (Ministerio de Salud Pública, 2021).
According to Zeca (2019), in Guinea Bissau, there is a lack of strict control of patients with motor incomplete cervical spinal cord injuries at the national level. Added to this is the absence of a health strategy for the Guinean population to become aware of the benefits that physical activity brings to health; on the other hand, there are no specific works that link the practice of physical activity with the health of the population.
Patients with motor incomplete cervical spinal cord injuries have as their only reference, for their treatment, a medical prescription and they only follow pharmacological procedures; 95 % are of low economic resources and 5 % can follow the treatment in hospitals. There is an almost total ignorance of the benefits of physical exercise for its treatment, which is why the development of health strategies regarding the practice of physical exercises for these patients is considered insufficient.
The objective of the study presented is focused on determining the impact of physical exercises in the rehabilitation of patients with incomplete cervical spinal cord injuries in Guinea-Bissau.
MATERIALS AND METHODS
The research is structured as follows: longitudinal, prospective, pre-experimental type of study, with follow-up of a single group. The population was made up of patients admitted to the therapeutic area of the National School of Physical Education and Sports, Bissau, in Guinea-Bissau and are carriers of incomplete motor cervical spinal cord injuries and the sample, ten patients: six male and four female. female, all between 13 and 58 years of age, with spinal cord injuries at level C4 to C8.
Methodology
The methods used within the qualitative order were:
Documentary review, this method was used to review the medical records and documents based on the rehabilitation of said disease.
Quantitative:
Measurement, as one of the most used methods, was used in a large part of the study to specify aspects related to gait and activities of daily living. It was evaluated with the ASIA scale, modified by the Julio Díaz Hospital National Rehabilitation Center, of Cuba.
The experiment was organized with the following steps:
a) Four Physical Education teachers were selected who had the best performance during the training course that was carried out in order to prepare the professionals, as one of the actions for the implementation of physical exercises. b) The inclusion and exclusion criteria for the selection of the 10 patients that made up the sample were elaborated.
Inclusion criteria
No more than two years of evolution with the disease.
Patients with motor incomplete cervical spinal cord injuries classified in ASIA between level C4 to C8.
Patients who have not participated in physiotherapeutic treatment in another similar space.
Level I pressure sore.
Signed informed consent.
Exclusion criteria
Inability to attend sessions.
The patient may suspend their participation in the study at any time they wish.
The researcher may decide to withdraw a patient from the project if he or she does not comply with the rules of the protocol or for their safety.
c) Application of the initial evaluation of the selected patients, using the following instruments:
Spanish version of the spinal Cord Independence Measure version III (SCIM III), modified by the Julio Díaz Hospital National Reference Center of Cuba and the ASIA scale (Garrido et al., 2015) . From the SCIM III scale, some items related to other activities were excluded and only the items related to: food and care (feeding, bathing, dressing, and grooming) were analyzed; breathing and sphincters (bladder, intestine and toilet); strength in all key muscles; mobility (interiors and exteriors, on any surface) through them, the patient's gait was evaluated in certain environments with levels of complexity that would allow the Physical Culture specialist to foresee the displacement capacity that a patient could achieve, as well as the reduction of barriers that allow their social integration.
Feeding, toileting and bathing: illustrated the patient's ability to use basic materials for this purpose, with a scale of 0 to 3 points.
Dress: related to the use of changing rooms, with a scale of 0 to 4.
Breathing and sphincter management:
Breathing: control of respiratory capacity, with a score from 0 to 10.
Bladder management: linked to control of the urinary system, with a scale of 0 to 15.
Bowel management: indicated the patient's ability to control bowel function, scores from 0 to 10
Use of the toilet, with a scale of 0 to 5 points.
Interior mobility: which defined the patient's ability to move within their home and was scored from 0 to 8.
Mobility over moderate distances: which represented the patient's ability to move over distances between 10 and 100 meters and was scored from 0 to 8.
Outdoor mobility: which represented the patient's ability to move over distances greater than 100 meters and was scored from 0 to 8.
Handling of stairs: which evaluated the patient's ability to go up and down stairs that was scored between 0 and 3.
Scales for the evaluation of 32 key muscles, scored from 0 to 5 for each one and the overall score is 160 points.
d) Application of physical exercises for the rehabilitation of patients with spinal cord injuries: it consisted of the application of physical exercises by four Physical Education teachers in Guinea-Bissau, qualified in neuro -rehabilitation, selected for 24 months for each patient, with the following organization by stages:
In the treatment process, the essential basis was physical exercises and for the description of the exercises, the CIREN program (Echemendía & Gómez, 2021) was taken into account, which served as a tool to determine the stages, the methodological indications and the parts that make up the treatment sessions through physical exercises; they were described in detail with the characteristic of being able to be executed in a simple way and with few material resources, in any center that has as a fundamental requirement the adequate preparation of a rehabilitator.
As a general objective, it was proposed to promote functional independence in patients with incomplete cervical spinal cord injuries through physical exercises and as specific objectives:
Stages of the system of physical exercises
When preparing the program for patients with these characteristics, the division into stages of different revised neurological rehabilitation programs was taken into account, it was considered to structure it into three fundamental stages.
General preparation stage: the general physical preparation of the patient began. We worked on the recovery of movement and joint amplitude, as well as the development of motor qualities, therefore, the objectives of the same were: to improve posture, normalize muscle tone and improve joint amplitude, increase physical work capacity and improve balance in sitting and standing positions, with the necessary orthopedic technical aids.
Special preparation stage: the objectives of this stage were aimed at continuing the work of the previous stage, improving strength endurance and muscle tone, developing endurance, improving activities of daily living, establishing static gait patterns and dynamic and develop capacities such as balance and coordination.
Functional preparation stage: it was aimed at perfecting static and dynamic gait patterns, balance and coordination, maintaining the strength and muscle tone achieved in previous stages, carrying out a functional gait with the least number of accessories and perfecting the activities of daily life.
The stages, although directed at different objectives, were closely related; this allowed a continuous, dynamic and flexible process.
Contents that were included in the program.
First stage. General preparation
Neck exercises.
Exercises for upper limbs.
Trunk exercises.
Hip exercises.
Exercises for balance.
Exercises to strengthen the lower limbs.
Second stage. Special preparation.
Arm strengthening exercises.
Exercises with apparatus.
Shoulder strengthening exercises.
Exercises with apparatus.
Trunk strengthening exercises.
Exercises in crawling position or support with hands, knees and feet.
Exercises to strengthen the lower limbs.
Exercises with apparatus.
Third stage. functional preparation
Gait with forearm crutches or a walker with or without orthoses (long, short, equine corrector, stabilizing knee pads).
Gait with forearm crutches or a walker (with or without the same attachments).
Gait with forearm crutches or cane (IDEM).
Static and dynamic gait pattern exercises in patients who do not need help.
Walking without forearm crutches.
Walking with obstacles.
March out of parallels and uneven terrain.
Go up and down stairs and inclined planes.
Walking on Frankel `s footprint.
Organizational structure of treatment sessions.
The treatment session should have lasted 120 minutes, divided into 3 parts:
Initial: basic preparation so that the patient could start work. It lasted 20 minutes.
Main: where the objectives of the session were fulfilled. It had a duration of 85 minutes.
Final: allowed the recovery of the loads received during the previous parts of the session and lasted approximately 15 minutes.
Dosage of the session that was established from the functional group.
The therapeutic physical exercises were applied in three stages and each one lasted eight months, due to the characteristics of the disease; the duration of each session was two hours with five weekly frequencies in a period of 24 months.
Methodological guidelines for the application of physical exercises
Recovery time: between sets of exercises two to five minutes.
Ensure that the patient or family members give informed consent and have a medical certificate from the patients to undergo the proposed treatment.
The place must be spacious, with adequate ventilation and lighting.
The technical-hygienic conditions necessary for this process must be respected.
The treatment must be suspended if any symptom appears that indicates a risk to health (fever, bleeding, pain, among others).
Patients should wear comfortable clothing to facilitate movement.
The treatment should be applied at least two hours after eating food, but not on an empty stomach.
The mobilizations must be done from the distal areas to the proximal ones.
In each session, the body's reaction to the loads should be recorded and the patient's variations periodically evaluated.
The rest during the session must allow the complete recovery of the patients.
To work on strength, it is recommended to execute between 40 % and 60 % of maximum effort, using the repetition method.
The patient must be explained what the activities to be carried out consist of before starting them.
Teach the relative to take the heart rate, to use it in the work sessions.
Patients should hydrate before, during and at the end of the exercises.
Breathing exercises should be performed at rest between series.
In the case of patients with spasticity, they should be relaxed and then start the mobilizations.
RESULTS AND DISCUSSION
In the experiment, physical exercises were applied during treatment in the rehabilitation process of patients with incomplete cervical spinal cord injuries. The results obtained provided elements that allowed knowing the positive influence of these exercises in these patients. The impact of these exercises on the patients was obtained from the comparative analysis, in the applied tests.
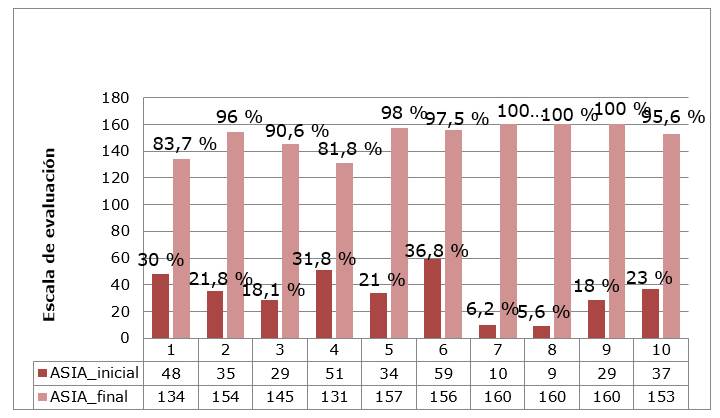
Comparative analysis of the initial and final test results of the key muscles
The results presented in figure 1 showed that all the patients participating in the study achieved a significant increase in physical and functional capacity after 24 months of practicing physical activity. Of all the participants, the patient with the lowest result was number four who began with 31.8 % in his initial test and reached 81.8 % in the final test. In the cases, patients' number seven, eight and nine were those who achieved the best results, patient seven began the treatment process with 6.2 % and ended with 100 %, and patient eight was the one who obtained the best result, because in his initial test he started with 5.6 % and ended with 100 %, it can be noted that patient nine obtained 18 % in the initial test and after receiving the treatment he reached 100 %.
This means that physical exercises had a positive influence on the improvement of self-validation of the patients participating in the research, which favored socioeconomic reintegration (Figure 1).
Descriptive statistical analysis of the initial and final test results of the patients
Table 1 shows the descriptive statistical data of the functional tests, analyzed in groups, carried out at the beginning and at the end of the treatment period of the patients. The most relevant thing that was observed in both tests is an improvement in the parameters of activity of daily living and gait of the final values in terms of the mean, it was also observed that the dispersion of the data decreased in both tests, as well as the range between the maximum and minimum values of the sample (Table 2).
Table 1. - Descriptive statistics
| No. | Means | Dev . Deviation | Minimum | Maximum | |
| AC1 | 10 | 2.60 | 3,273 | 0 | 10 |
| Res.Sph.1 | 10 | 32.20 | 3,011 | 26 | 35 |
| Mov1 | 10 | .80 | 1,932 | 0 | 6 |
| TP. SCIM.1 | 10 | 35.60 | 5,985 | 27 | 49 |
| AC4 | 10 | 16.40 | 1,578 | 12 | 17 |
| Res.Sph.4 | 10 | 39.10 | 1,449 | 36 | 40 |
| Mov4 | 10 | 38.10 | 2,807 | 31 | 40 |
| TP. SCIM.4 | 10 | 93.60 | 4,377 | 82 | 97 |
Legend: AC Food and Care. Res.Sph. Breathing-Sphincter. Mov. Motion
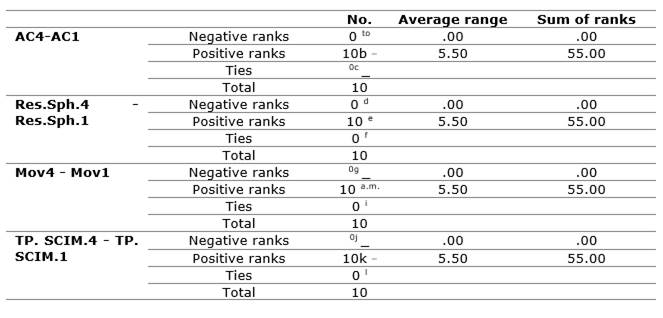
To verify the results, the non-parametric Wilconxon test was performed with a significance level of p<0.5 (Table 2), where it was clearly observed that statistically significant changes were obtained in both tests, from which it could be inferred that the improvement obtained by the patients in gait, activities of daily living and social reintegration, was due to the introduction of physical exercises.
Table 2. - Contrast statisticsª
| No. | Means | Dev . Deviation | Minimum | Maximum | |
| AC1 | 10 | 2.60 | 3,273 | 0 | 10 |
| Res.Sph.1 | 10 | 32.20 | 3,011 | 26 | 35 |
| Mov1 | 10 | .80 | 1,932 | 0 | 6 |
| TP. SCIM.1 | 10 | 35.60 | 5,985 | 27 | 49 |
| AC4 | 10 | 16.40 | 1,578 | 12 | 17 |
| Res.Sph.4 | 10 | 39.10 | 1,449 | 36 | 40 |
| Mov4 | 10 | 38.10 | 2,807 | 31 | 40 |
| TP. SCIM.4 | 10 | 93.60 | 4,377 | 82 | 97 |
When analyzing the results of the initial and final test, they were less significant, according to the Wilcoxon signed rank test (0.001< 0.05). At 24 months, the existence of differences in favor of the results of the final test was confirmed, where the ranges of the initial test were lower than the ranges of the final test, which meant that after the application of the strategy the change was significant (Table 3).
DISCUSSION
The physical exercises socialized with the professionals in the sample guaranteed a methodical functional process for the treatment of patients with motor incomplete cervical spinal cord injuries in an organized, planned, oriented, systematic and controlled manner; which allowed to establish a common work guide for all the rehabilitators of the Therapeutic Area of the National School of Physical Education and Sport. The results of the preliminary study showed an increase in the functional capacity of the patients, without the presence of complications, this positively influenced the improvement of self- validation and social and labor reintegration. All the patients met the objective in the 24 months foreseen and 100 % of the patients participating in the treatment process achieved functional independence, according to the final SCIM scale of the assessed items.
With this study, it was possible to verify that when the instruments selected for the evaluation of patients with ASIA spinal cord injuries (SCIM III) are available and there is adequate organization and control, satisfactory results can be obtained as demonstrated by the Echemendía studies (2021) and De Oliveira, et al. (2021) who present similar results. Another achievement of the study was to highlight the positive changes that can be obtained in patients through intensive physical exercise in spinal cord injuries, supported by different studies such as that of Gaspar et al. (2019) and Hicks (2020), which represented the achievement of greater independence for the quality of life of patients, as corroborated by the research by Amtmann, et al. (2019); Da Silva (2019) and Ribeiro, et al. (2020).
CONCLUSIONS
The physical exercises allowed the improvement of the functional physical capacity, the motor skills and the socio-occupational integration of the patients with incomplete cervical spinal cord injuries in Guinea-Bissau.
The analysis of the results revealed the existence of significant differences between the results of the post- test in relation to the pre-test, which positively influenced the improvement of self-validation in them.
REFERENCIAS BIBLIOGRÁFICAS
Amtmann, D., Bocell, F. D., Bamer, A., Heinemann, A. W., Hoffman, J. M., Juengst, S. B., Rosenberg, M., Schneider, J. C., Wiechman, S., & McMullen, K. (2019). Psychometric Properties of the Satisfaction With Life Scale in People With Traumatic Brain, Spinal Cord, or Burn Injury: A National Institute on Disability, Independent Living, and Rehabilitation Research Model System Study. Assessment, 26(4), pp. 695-705. https://doi.org/10.1177/1073191117693921 [ Links ]
Arriola, M., López, L., Camarot, T. (2021). Perfil epidemiológico, clínico y funcionalidad alcanzada de la población con lesión medular traumática asistida en el Servicio de Rehabilitación y Medicina Física en el Hospital Universitario. Revista Médica del Uruguay 37(2): e37208. http://www.scielo.edu.uy/scielo.php?pid=S1688-03902021000201207&script=sci_arttext [ Links ]
Bataller, B. E. et al ., (2021). Factores predictivos de destino al alta tras una lesión medular. Neurologia (Barcelona) [ISSN 0213-4853]. https://www.elsevier.es/es-revista-neurologia-295-avance-resumen-factores-predictivos-destino-al-alta-S0213485321002735 [ Links ]
Chasman, D., Iyer, N., FotuhiSiahpirani, A., Estevez Silva, M., Lippmann, E., McIntosh, B., Probasco, M. D., Jiang, P., Stewart, R., Thomson, J. A., Ashton, R. S., & Roy, S. (2019). Inferring Regulatory Programs Governing Region Specificity of Neuroepithelial Stem Cells during Early Hindbrain and Spinal Cord Development. CellSyst, 9(2), pp. 167-186 e112. https://doi.org/10.1016/j.cels.2019.05.012 [ Links ]
Da Silva, L. H. (2019). Programa de treinamento de HIIT combinado com exercício resistido e seus efeitos sobre a capacidade física e composição corporal de adultos com lesão medular/ Layenne Hellen Lima da Silva. - João Pessoa. https://repositorio.ufpb.br/jspui/handle/123456789/17840 [ Links ]
De Oliveira, C. A., et al., (2021). Lesões neurológicas: da fisiopatologia à repercissao social. Ponta Grosso Paraná Brasil. https://educapes.capes.gov.br/handle/capes/585578 [ Links ]
Echemendía, A., & Gómez, R. (2021). Programa de rehabilitación física para lesiones raquimedulares. (Actualización). Centro Internacional de Rehabilitacion Neurológica. [ Links ]
Echemendía del Valle, A. (2021). Metodología para el entrenamiento de la marcha convencional en pacientes con lesiones medulares. Estudio preliminar. PODIUM - Revista de Ciencia y Tecnología en la Cultura Física, 16(3), pp. 757-771. https://podium.upr.edu.cu/index.php/podium/article/view/991. [ Links ]
Hernández, D. M. L., & Rodríguez, G. M. (2014). Electroestimulación en Músculos Rectos Abdominales Para el Aumento de la Capacidad Respiratoria Proporcional Para el Habla en Personas con Lesiones Medulares Cervicales. Revista Ecuatoriana de Neurología, 23(1-3). http://revecuatneurol.com/wp-content/uploads/2016/01/Electroestimulacio%CC%81n-en-mu%CC%81sculos-rectos-abdominales_REN-Vol-23-N%C2%BA1-3-2014-5.pdf [ Links ]
Garrido, A. G., Espitia, A. M. L., Magraner, L. M., Galceran, L. R., Canudes, E. S., & Viejo, M. A. G. (2015). Validación española del cuestionario International Spinal Cord Injury Pulmonary Function Basic Data Set para valorar la repercusión de la lesión medular en el sistema respiratorio. Medicina Clínica, 145(11), pp. 477-481. https://www.elsevier.es/en-revista-medicina-clinica-2-articulo-validacion-espanola-del-cuestionario-international-S0025775315002511 [ Links ]
Gaspar, R., Padula, N., Freitas, T. B., de Oliveira, J. P. J., & Torriani-Pasin, C. (2019). Physical Exercise for Individuals with Spinal Cord Injury: Systematic Review Based on the International Classification of Functioning, Disability, and Health. J Sport Rehabil, 28(5), pp. 505-516. https://doi.org/10.1123/jsr.2017-0185 [ Links ]
Hicks, A. L. (2020). Locomotor training in people with spinal cord injury: is this exercise? SpinalCord. https://doi.org/10.1038/s41393-020-0502-y [ Links ]
Ministerio de Salud Pública de guinea- Bissau, (2021). Informe nacional: Traumas en columna vertebral. Empresa, archivo número 191. P. 58. Djimital (Bissau). Avenida Antigoscombatentes. [ Links ]
Miller, L. E., Zimmermann, A. K., Herbert, W. G. (2016). Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: systematic review with meta-analysis. MedDevices, 9, pp.455-466. https://pubmed.ncbi.nlm.nih.gov/27042146/ [ Links ]
Ribeiro, N. F., Gomes, C. R. R., Tanhoffer, R. A., Leal, J. C., Bottaro, M., &Carregaro, R. L. (2020). Muscle Strength Cutoff Points for Functional Independence and Wheelchair Ability in Men With Spinal Cord Injury. Arch Phys Med Rehabil, 101 (6), pp. 985-993. https://doi.org/10.1016/j.apmr.2020.01.010 [ Links ]
Zeca, S. B. (2019). Factibilidad teórica de un programa de ejercicios físicos para la rehabilitación de los pacientes con lesiones medulares cervicales en Guinea-Bissau. Universidad de Ciencias de la Cultura Física y el Deporte. La Habana. 16(34). pp. 30-43. https://dialnet.unirioja.es/servlet/articulo?codigo=7000692 [ Links ]
Received: November 07, 2022; Accepted: January 17, 2023











 texto en
texto en