INTRODUCTION
The United Nations Conference on Trade and Development (UNCTAD) warns of dire consequences if poor communities are excluded, or exclude themselves from technological advances. It points to technology as the key to getting out of the effects of the crisis exacerbated by the COVID-19 pandemic1. One of those emerging and disruptive technologies that promotes change at an economic and social level, and one of the fundamental elements of Industry 4.0, is 3D (three-dimensional) printing, also known as additive manufacturing or rapid prototyping and defined as the set of processes used to make a three-dimensional physical object by applying layer by layer of a solid material at room temperature, with a known melting point, controlled by a computerized system2; allowing the construction of a tangible model from a virtual one, obtained from medical or not medical images3.
In medicine, 3D printing is used for surgical planning, prosthetic fabrication, education and training, tissue construction, and drug printing4,5. It’s the ideal method for creating complex patient-specific geometries from medical imaging modalities and 3D laser scanning. It offers the ability to design patient-specific devices and do so in a cost-effective manner. Although, due to the wide range of advanced materials available for 3D printing, the necessary mechanical durability requirements can be achieved; personalization in patient care is the mainstay that justifies the revolution experienced by additive manufacturing6,7.
This technology is one of those that most affects the improvement of production processes due to the personalization of products, their productivity, quality, efficiency and sustainability2. The impact of 3D printing in medicine rests on these reasons. It has existed for more than 30 years3; however, its notoriety has grown in the last seven and despite its advantages its exploitation in our environment is little less than incipient. Based on what was previously stated, the objectives of the research were to design and develop solutions based on three-dimensional technologies to respond to teaching and practice of biomedical sciences problems in order to achieve the goal of improving attendance. These problems by themselves, and the solutions they imply, add a significant burden on clinical practice and the health system. The article scope presupposes the promotion of closed-cycle research and development projects, which lead to the introduction of products based on the use of three-dimensional technologies.
MATERIALS AND METHODS
A collaborative research, of technological development, was carried out between the Center for the Study of Advanced and Sustainable Manufacturing (CEFAS, acronym of Centro de Estudios de Fabricacion Avanzada y Sostenible in Spanish) of the University of Matanzas and the Matanzas University of Medical Sciences, between September 2019 and July 2022. The fabrications were developed at CEFAS. For the cases of the trachea, the model for craniosynostosis repair and the mold for skull prosthesis, the development started from the acquisition of DICOM (digital imaging and communication in medicine) images―from computed tomography (CT)―, which were then processed ―segmentation included―, converted into standard tessellation language (STL) format and in the case of the mold for cranial prosthesis, it was printed and finally post-processed, the last step in the additive manufacturing process, where the support material is removed or cleaned, the model is cured and polished.
The virtual designs (for the prosthetic hand, O2 line splitters, tissue expander plate, scaffolds, and syringe holder for aspiration) were developed using computer-aided design software, specifically Solid Works, a CAD Software for Windows from SolidWorks Corp., a subsidiary of Dassault Systems, France. For the manufacture of the face shields, minimal changes were made to designs available, free of charge, on the Internet. The preprint processing, from the DICOM images for the cases of segmentation of a trachea, the model for the craniosynostosis and the frontal prosthesis were developed on InVesalius 3.1 and Mimics (Materialise’s Interactive Medical Image Control System) version 17.0, software for the processing of medical images and the creation of 3D models. For their conceptualizations, the anatomical and functional elements necessary in each respective case were taken into consideration.
For the manufacture of the anatomical bone figures, the customized external breast prosthesis prototype and the breast mold for autologous reconstruction, an XHCV3D model scanner was used to obtain the images that begin the workflow. From references placed in the selected place (right breast on a mannequin as a model and bones), the scan was performed by rotating the object each time an image was completed, to obtain as much information as possible. Then, through the self-scanning software, the images were integrated, obtaining a superficial mesh that was exported in STL format. The file was imported into Meshmixer software to crop out the region of interest, laminated with Cura software, and printed.
The material used to print the prototypes was polylactic acid (PLA), an inexpensive and biodegradable polymer that allows the original model to be perfected, sterilized in ethylene oxide below 40 degrees and subjected to chemical sterilization with glutaraldehyde8; an important fact for the specific case of the mold for autologous repair, since once the mold is in the surgical field it will be used to place the free flap, although a sterile cover could be used9. The printing process for all cases was by fused deposition using a Wanhao Duplicator 6 Desktop 3D printer.
RESULTS
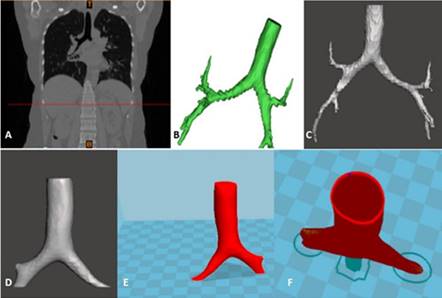
Among the products obtained, five biomodels were developed. Four didactic, three prints (femur, pelvis, and left foot) and one preprint, of a trachea (figure 1, where A is a coronal CT reconstruction. B and C are segmentation from A. D, smoothed. E and F are models to print: E, solid; F, with light); and finally, a personalized one for the planning of the surgical repair of a craniosynostosis.
A custom cranial implant mold was also designed and fabricated from DICOM images. Additionally three models of cheap mechanical hand prostheses, easy to produce and assemble, were developed (figure 2). In a similar way were manufactured O2 line splitters―a device that allows several patients to be connected to the same oxygen regulator―as well as facial protectors, with a simple design that facilitated the assembly of the components and their sterilization. Several prototypes of scaffolds for cell cultures were also obtained.
In addition, a syringe holder with ergonomic support was designed and manufactured. It must be the first printed in Cuba. (Fig. 3)
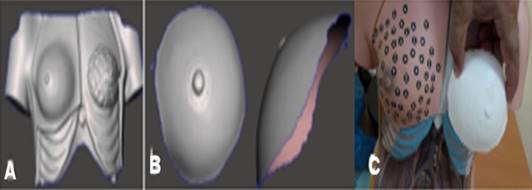
Furthermore, a prototype of external breast prosthesis was obtained [figure 4; where (A) corresponds to the scan of the frontal region of the thorax; (B), the cutting out the region of interest (right breast) and (C), is a visual control of the prototype obtained]. A breast mold for autologous reconstruction and a tissue expander plate that allows the use of vascularized tissue of local origin, avoiding the use of flaps in reconstructions were obtained as well.
DISCUSSION
Despite the limitations indicated to additive manufacturing―delayed printing time, a debatable fact according to the authors; high initial cost and of the creation processes, also quickly recoverable according to the authors; as well as the limitation of materials10; to which copyright infringement and harmful use, such as the manufacture of firearms, can be added―, this technology is an economical and sustainable solution, but beyond that, it guarantees the independence of the industry1,2, basically in times of supply crises as in the case of the post-pandemics. Among its benefits should be mentioned11,12:
Manufacturing speed. Reduce production times by up to 90%. This makes it possible to intensify the manufacturing pace and reduce the cost of each part;
Production on demand. This manufacturing model allows for smaller-scale and tailored runs, maintaining profitability at all times;
Reductions of costs due to the fact that the digital processes of additive manufacturing also have an impact on storage and logistics costs. With this solution, a virtual stock is available and each piece is manufactured on the spot. In addition, the printers and materials used are getting cheaper;
Energy saving. Digitally fabricated parts are much lighter. That is why this type of production requires less energy to operate and consumption is significantly reduced;
Sustainability. It provides a cleaner and more respectful production with the environment. It also provides a reduction in both energy consumption and transport costs. It also benefits the logistical apparatus since the raw material occupies less space than the pieces themselves and, by betting on local production, dependence on those furthest away producers is eliminated.
Replicas of human body sections [trachea (figure 1) and bones], were obtained, which preserve the proportions and morphological veracity―the color depends on the color of the material used―, without the possibility of decomposition or contamination. This solution allows access to the anatomy avoiding availability, biosecurity, cultural and religious problems, without detrimental of teaching, by having an exact replica, which avoids the bias of models previously manufactured as teaching aids. In addition, it shows that it is possible to create a file or atlas of three-dimensional images obtained by surface scanner or CT. Likewise, tests on animal models, mannequins or cadavers are eliminated. It directly and positively impacts the teaching-learning process and the economy of this process in terms of the acquisition, creation and maintenance of conservation, storage and biosafety conditions.
Although for the development of curricular competencies in bronchoscopy there are low and high fidelity (virtual) simulators, each one with its advantages and disadvantages13,14, these authors agree with Gando13 in the sense that 3D printing technology, in addition to being easily available since it does not have to be shared with other specialties, allows the creation of simulation models with greater realism and new pathological situations that cannot be reproduced in low-fidelity models, but with the advantages of this method: its low cost and high availability. And, on the other hand, the same for bronchoscopy as for surgical planning, the simulators manufactured by 3D printing outperform the virtual format in that they give the possibility of analyzing the piece in its real size, adding spatial and tactile dimensions.
In the case of the trachea, and since it was only intended to demonstrate its preprint processing, the authors worked with the region of interest from which only the trachea and main bronchi were obtained. If it were enlarged, more branches of the bronchial tree would be obtained, which would facilitate anatomical learning and endoscopic orientation.
Coinciding with de Frutos Marcos et al.15 the impression of the model for surgical repair in a case of craniosynostosis and from it, the planning of surgery, improved the surgeon's ability to clearly differentiate the spatial relationship of the anatomy and adjacent vital structures. It likewise improved the understanding of the scale, shape, and correct identification of the spatial geometry of affected bone structures. The intraoperative validation of the model confirmed the fidelity of its obtaining and the precision of the pre-surgical work. It had a positive impact on the outcome of the surgery and with it, impacts on the psychomotor development of the child.
Contrary to precise 3D printed and custom templates for intraoperative molding of implants in cranioplasty, manual molding, while feasible, does not always produce aesthetically pleasing results and may compromise concordance16. For this reason, a mold for a personalized cranial prosthesis was also designed and manufactured from DICOM images for a patient who suffered severe head trauma. Based on these images, a 3D printed model was obtained that served as a mold to create a personalized Subiton Surgical G implant, achieving adequate concordance and effective repair of the defect.
Mechanical hand prosthesis. Although an established trend points to the manufacture of myoelectrically controlled prostheses17, mechanical ones, working through a system of cables or harnesses, have the advantage of manufacturing time and the absence of complex components such as motors, batteries, electronic boards and sensors that are extremely expensive and difficult to obtain in different contexts. On the other hand, cosmetic prostheses would only aim to replace a member or part of it, taking into account its aesthetics rather than its functionality. Prostheses also contribute to tissue protection and psychomotor development in the case of children18. One of the development models was personalized according to the characteristics of the left hand of a male patient with a congenital malformation. This prosthesis allowed the patient to perform basic functions such as pincer and cylindrical grasp. Its implementation and use will improve the quality of life for specific patients19. This solution also has an economic impact due to the savings that non-importation represents knowing that the cost of a prosthetic arm―although really variable―, can be in the range of USD $5 000 for the simplest prosthetic arm and approximately USD $100 000 for a neuro-prosthetic model20, however, those manufactured at CEFAS are significantly cheaper.
O2 line splitters are devices that allow several patients to be connected to the same oxygen regulator, thus multiplying the possibility of using the available gas in patients with an indication of supplemental O2. This solution was of great help in combating the health crisis experienced during the COVID-19 pandemic. It directly impacted by improving emergency care and avoiding the transit of patients to stages of greater respiratory compromise and deterioration of the general state, thereby reducing the human and economic cost that serious illness and intensive care represent.
Also, during the COVID-19 pandemic, there was a major shortage of masks and face shields. In collaboration with colleagues from Brazil, Canada and Germany, CEFAS manufactured protective masks that were donated to the Cuban health system in the midst of the health battle against the disease. It supplied the non-existence at a certain time, reduced the cost of its purchase and increased the security of the providers, improving care.
Of paramount importance for filling bone lesions are scaffolds for cell cultures. The function of a scaffold is to provide a biometric environment for cell attachment, proliferation, and secretion of extracellular matrix to replace or regenerate tissues, functionally and structurally21,22. Several scaffolds, orthohedral and cylindrical, were built to order and in coordination with another scientific institution. Some were coated with calcium hydroxyapatite for biological testing.
A syringe holder model (figure 3) was designed and manufactured with ergonomic support, light material (and therefore lighter than traditional ones)―although with similar performance―, customized size, ambidextrous and significantly cheaper than models existing on the market. In addition to the marked economic impact, it has an impact on the improvement of diagnostic and therapeutic processes―related in the first instance, to the care of cancer patients―, also on the working conditions of the medical practitioner, morbidity and mortality and with all this, in health-care. Its unavailability hinders the interventional radiologist's freedom of action and definitively, the diagnostic or therapeutic procedure, according to the case. The tests showed the easy handling of the device. Although what really must be sterile is the syringe that will be used, the device is sterilizable. In the consultation of the state of the art carried out by the authors, a prototype like this had not been printed.
The first prototype of external breast prosthesis (figure 4) made by the authors, demonstrated the efficacy of the existing surface scanner at CEFAS given the inconvenience of obtaining images by tomography for these cases. With this, the algorithm of the process was established, which obeys the need to achieve personalized breast prostheses for mastectomized patients and to respond to the non-existence and discomfort manifested by carriers of prostheses that are marketed by standard sizes. Mastectomized women who can’t, or don’t want to have a breast implant would also benefit. The economic and psychological impacts―and with the latter, the improvement in the quality of life―are the most significant. In this case, the designs are obtained from anatomical data of the contralateral healthy breast, by three-dimensional mirror inversion scanning. Patients typically must obtain prostheses (imported, dependent on supply chains and financing) based on their size―which provides only minimal customization.
On the other hand, but also in relation to breast cancer, ignoring the variation of the breasts in volume, height, width, shape or orientation during the planning and execution of autologous reconstruction leads to undesirable results. To avoid this, custom breast molds that satisfy the requirements of both the patient and the cosmetic surgeon are created9. These facilitate understanding and interaction with the patient, as well as flap modeling. The results show more symmetry, high reconstructive quality, less surgical time is required, avoids or reduces the need for symmetrization in the healthy breast and generates savings for the institutions23. According to Hummelink’s9 experience, these authors consider that it is necessary to increase the thickness of the mold developed, from 2 mm―thickness of the form―to 4 mm to provide greater resistance during its intraoperative use.
The results of this investigation, like other similar ones reported internationally5-10, contribute directly, in a mediate or immediate way, to the solution of existing needs in the areas of intervention. These have a positive impact on the know-how of the institutions involved and on the sustainability of the health system due to their effect on costs, income, energy savings, decentralization of solutions and supply management, introduction of new practices or methods of work management and relations with other organizations; and likewise, in profitability, personalization, quality of care and satisfaction due to the faster incorporation into the working life of specific patients, the decrease in morbidity and the increase in the quality of life. On the other hand, in the medium term, they have an impact―also positive―, on the positioning of the solutions and the penetration of new markets. The positive preliminary results and the increasing accessibility due to the decrease in the costs of materials and equipment will contribute significantly to the exponential growth of 3D printing technologies in medicine. In the era of personalization and minimal invasion, its use anticipates a potential change in the resolution of complex conditions. With it, in short, a new paradigm is established.
As limitations of the study, access to data should be pointed out due to the absence of some specific medical conditions sub-records that prevent knowing the exact needs of the manufactures, the lack of previous studies carried out in our environment, at least published, that allow to substantiate the relevance of the research, and, finally, the manufacture of solutions and prototypes only in PLA.
The results of this work demonstrate the feasibility of using solutions manufactured by three-dimensional technologies for the practice and teaching of biomedical sciences in Matanzas, and show the need to develop them. It is therefore imperative that managers and the medical community in general, begin to become aware and accumulate experiences to guarantee its optimal use. Its development will improve healthcare with a significant reduction in costs, favoring local production and eliminating dependence on foreign producers.