Mi SciELO
Servicios Personalizados
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Ciencia y Deporte
versión On-line ISSN 2223-1773
Ciencia y Deporte vol.8 no.3 Camagüey sept.-dic. 2023 Epub 03-Sep-2023
http://dx.doi.org/10.34982/2223.1773.2023.v8.no3.003
Original article
Physical Therapy for Motor Symptoms in Patients with Parkinson’s Disease
1Universidad de Holguín. Facultad de Cultura Física y Deportes Holguín, Cuba.
Introduction:
Neurodegenerative diseases are the main cause of physical-motor disabilities, such as Parkinson disease. Despite the advances in health, this disease does not have a definitive cure; some of the main treatments include physical rehabilitation, with a neuroplasticity perspective. However, there is a trend to use conventional physical exercise instead of traditional forms, thus putting aside the potentialities of the latter.
Aim:
To set methodological parameters in traditional therapeutic exercises that enable better physical therapeutic care of patients with Parkinson disease.
Materials and methods:
The research has prospective, quasi-experimental, quantitative character practices in five patients (age 61±2.53 years), with a diagnostic of Parkinson’s disease (stages 1-2.5, according to Hoehn-Yahr), accounting for 20.8 % of the population.
Results:
After four months of implementation, the patients were observed to get up, walk, and sit again in less time, with a mean of 12.6±2.96s. An assessment of the Berg scale showed that 80.0% of the sample reached the low-falling-risk category, with a total score of 47.6±5.12 points.
Conclusions:
The application of statistical methods (Wilcoxon signed-rank test) demonstrated the existence of a significant difference between the measurements performed, thus confirming the positive effect of Lian Gong’s practice in patients with Parkinson’s disease.
Key words: Parkinson’s disease; motor symptoms; Lian Gong exercises.
INTRODUCTION
The term Parkinson's disease (PD) is used to refer to people suffering from Parkinsonism," a frequent and complex neurodegenerative disorder characterized by the presence of motor and non-motor symptoms associated with damage to multiple structures of the central and peripheral nervous system" (Saavedra, Millán, and Buriticá, 2019, pp 3). Roca, et al. (2002, pp 353) and Álvarez (2014, pp 16-19) said that the pathological anatomy consists of depigmentation and selective loss of dopaminergic neurons in the compact area of the black substance, with the presence of Lewy bodies. It is clinically characterized by four cardinal signs: resting shivering, bradykinesia, muscle stiffness, and posture instability.
The prevalence of this disease is estimated at 0.3% of the general population, of which 1% occurs in people older than 60 years. (Álvarez, 2014, pp 16-20). Based on estimations from data published in the Statistical Yearbook of Cuba (2020), the PD prevalence will grow in the next decade due to the aging of the Cuban population, with 20.4% over 60. By 2030, a third of the population will be composed of elders.
In that sense, PD must be acknowledged as a global process that not only affects the patient but also their families and population groups. It is a truly social, economic, political, and cultural, phenomenon, whose extent entails multiple consequences that should be dealt with by society (Moreira et al. 2019, pp 3)
Despite the advances in science and technology in the area of health, a definitive cure has not been found in the case of PD. Its main treatments are split into two groups: pharmacological and non-pharmacological. The latter includes education, nutrition, and therapeutic physical exercises, one of the pillars in the treatment of PD patients, which has been recently approved with detailed studies about the concept of neuroplasticity (Knaepen, 2010); (Rodríguez, 2021).
Several researchers have corroborated the extent of this concept, Corcos et al. (2013) showed the favorable effects of aerobic exercise and endurance training in PD patients, corroborating the findings of Ferreira et al. (2019) and Johansson et al. (2022). Meanwhile, scholars like Capato et al. (2019), Santos et al. (2019), and Cabrera et al. (2020) spoke of the inclusion of different balance training sessions, with satisfactory results. The effect of music during the training has been studied by Michels et al. (2018), Calabrò et al. (2019), and Pohl et al. (2020), as well as the utilization of means, such as water, by Carroll et al. (2017) and da Silva et al. (2018).
In turn, the International Center for Neurological Restoration (CIREN) designed the Program for Patient Neural Rehabilitation, which has been implemented in Cuba with excellent practical results. So far, quite a few forms of implementing systematic physical exercise favor the development of motor alterations in PD patients. However, there is a trend to use conventional exercise and physical agents to the detriment of traditional ways in physical neural rehabilitation in patients with Parkinson's disease.
Accordingly, the authors were interested in finding ways to favor physical therapy for patients with Parkinson's disease. In that sense, this study aims to set methodological parameters in traditional therapeutic exercises that enable better physical therapeutic care of patients with Parkinson's disease.
MATERIALS AND METHODS
This research study has a prospective, quasi-experimental, and quantitative character. A population consisting of 24 patients diagnosed with Parkinson's disease in their health area in the municipality of Gibara, Holguin between December 2021 and March 2022. The sample included 5 patients (45-64 years old), mostly females (60%), selected intentionally (20.8 % of the population). The selection was based on the following criteria: Patients within stages 1 and 2.5, according to the HoehnYahr scale; willingness to take part in the research; authorization by the family physician to perform physical activities. Exclusion criteria: having complications or pathologies that limit physical activity.
To characterize and assess changes caused in the motor manifestations of patients with Parkinson's disease with the implementation of the proposal, a test was performed consisting in getting up, running 2.44m, and sitting again (Timed up and go, Rikli and Jones, 2013), and the Berg scale (Berg Balance Scale).
Statistical analysis: Descriptive statistics, absolute frequency, means, and standard deviation were used in this study. The normal rank distribution of data was calculated using the Kolmogorov-Simrnov, and inferential statistics (the Wilcoxon signed-rank test) was used given the nature of the distribution observed and the number of cases. The data were processed using IBM SPSS Statistic-22.
Ethics: This research study followed the Ethics Committee Standards at the Center for Physical Therapeutic Activity Studies, where all the participants signed a written consent statement, based on the principles of the Helsinki Declaration (2008).
RESULTS AND DISCUSSION
The criteria given by different authors and institutions familiar with this research topic were relevant to set the methodological parameters. Besides, it was conceived from the analysis of the physiological fundaments of physical exercise and its therapeutic role in dealing with neurodegenerative diseases, assessment of Lian Gong Shi Ba Fa exercises, and neural rehabilitation of Parkinson's disease. These parameters were laid out as follows:
The first treatment sessions are held from a standing position in patients with compromised balance, then other means will be used to support the patient.
This exercise is never to cause exhaustion.
Throughout the lesson, the teacher is to explain shortly the benefits of this activity.
Movements that require maximum joint extension must be performed up to the maximum extension of each patient, never pushing further.
The individuals will receive information that helps them gain more consciousness about their bodies and their sensations when exercising.
Exercises that require head and trunk leaning will be performed slowly, gradually increasing the extension. Never quick or sudden movements.
The work procedures and formations are frontal and gradual or step-by-step, to make learning easier. Besides, continuous exercising permits greater visibility of the teacher and the other way around.
The lesson may last up to 30 minutes, no more, with previous gradual and progressive time increases.
The technical errors will be corrected throughout the activity.
Each patient's requirement should be dealt with properly.
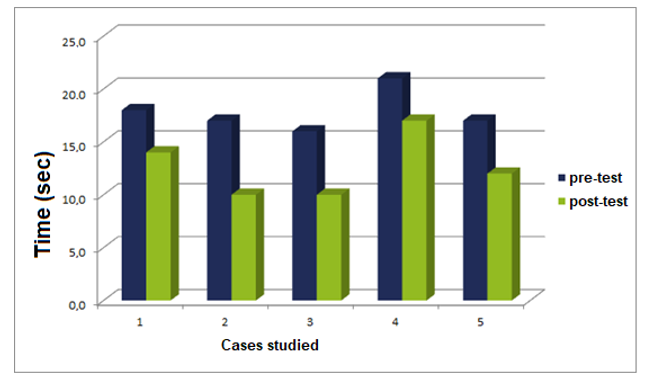
After four months of implementing the methodological parameters to the Liang Gong exercises in patients with Parkinson's disease, the tests (getting up, walking, going back to sit) showed a time decrease (Figure 1), with a mean of 12.6±2.96 s, 5.2 s less than during the pre-test, when the minimum was 10.0 s, while the maximum was 17.0 s. These results are similar to studies done by Da Silva and Israel (2018), who observed a 2.38 s decrease (pre-test 15.69± 5.55 s / post-test 13.31±2.83 s) upon the application of ground and in-water exercises for 12 weeks. Kurt et al. (2018) observed a 5.01 s decrease (pre-test 19.20±5.89 s / post-test 14.19±4.86 s) with the Ai Chi exercises for five weeks.
The findings of Calabrò et al. (2019) are also shown. They reported a 2s reduction (pretest 11±7 s / post-test 9±9 s) following the application of an exercise program on a treadmill for eight weeks. The data matched the reports of that study, which noted that the older the person, the greater time of execution of the test, with the appearance of the corresponding symptoms of Parkinson's disease.
The test's time of execution of 10s showed that 40.0 % of these individuals had few issues with balance and agility since separate individuals without problems make it in less than 10s. (Oliveira et al., 2016, pp 4); the other 60 % improved the values of the test, though still showed balance problems.
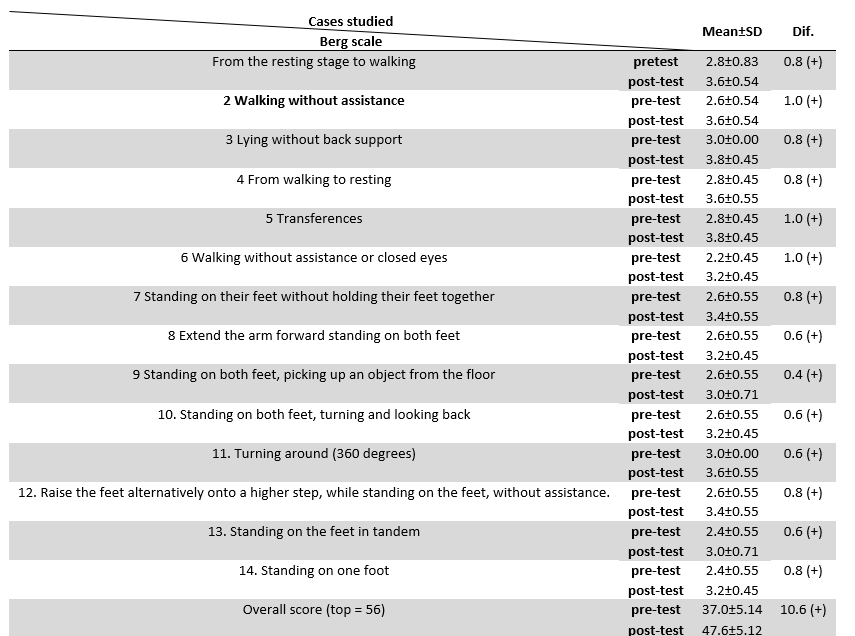
The assessment of balance deterioration during the functional activities expressed by the patients in the Berg scale (Table 1) following 80.0 % completion of the sample studied, was under the low fall risk category, whereas the rest stayed in the moderate risk of fall, with the highest score for this category (40 points). They showed a mean of 47.6±5.12 points.
The results achieved are linked to the studies conducted by Da Silva and Israel (2018), who had a 3.15-point increase (pretest 44.23±4.25 points / post-test 47.38±2.82 pt.), Kurt et al. (2018) achieving a 6.0-point decrease (pretest 35.0±19.0 pt. / post-test 41.0±18.0 pt) and Calabrò et al. (2019), who reported a 5-point decrease (pre-test 44±8 points / post-test 49±7 points).
The Kolmogorov - Smirnov confirmed data normality as homogeneous (p>0.05). Then the variables included in the study were described, and because of the nature of the distribution observed and the number of cases, it was better to use inferential statistics through the Wilcoxon singed-rank test for related samples, with a confidence level of the mean differences, of p>0.05. During the hypothesis contrast consisting of getting up, walking for 2.44m, and going back to their seats, the Berg scale measured 0.042 as a significance degree in the two tests, thus rejecting the null hypothesis (the mean differences between the pre-test and post-test was 0). Accordingly, there was a significant difference between both measurements.
CONCLUSIONS
The application of statistical methods confirmed the existence of a significant difference between the measurements performed, thus corroborating the positive effect of Lian Gong Shi Ba Fa practice during the physical therapy of patients with Parkinson's disease, with a progressive decrease in the deterioration of motor symptoms and recovery of balance through the functional activities.
REFERENCIAS BIBLIOGRÁFICAS
Álvarez Sintes, R. (2014). Medicina general Integral. Principales afecciones en los contextos familiar y social. (Vol.5) segunda edición. La Habana: Ciencias Médicas. https://temas.sld.cu/dengue/2022/11/10/medicina-general-integral-tomo-ii-principales-afecciones-en-los-contextos-familiar-y-social-vol-2-cuarta-edicion/ [ Links ]
Berrillo Caises, A. L., Rodríguez Díaz, J. C., Zayas Aldaya, D. de las Mercedes., González Garcés, Y., Torres Vega, R., Noris Romero, T. (2021). Intervención físico-terapéutica en la fase prodrómica de la ataxia espinocerebelosa tipo 2. EDUMED-Holguín. Universidad de Holguín. https://edumedholguin2021.sld.cu/index.php/edumedholguin/2021/paper/viewFile/510/253 [ Links ]
Cabrera, I., Jiménez, A. T., López, L., Rodríguez, J., Ortiz, A., & Valenza, M. C. (2020). Effects of a core stabilization training program on balance ability in persons with Parkinson’s disease: a randomized controlled trial. Clinical Rehabilitation 34(6): pp. 764-772. DOI: 10.1177/0269215520918631, https://pubmed.ncbi.nlm.nih.gov/32349543/ [ Links ]
Calabrò, R. S., Naro, A., Filoni, S., Pullia, M., Billeri Tomasello, P., Bramanti, P. (2019). Walking to your right music: a randomized controlled trial on the novel use of treadmill plus music in Parkinson’s disease. Journal of NeuroEngineering and Rehabilitation, 16(1).https://pubmed.ncbi.nlm.nih.gov/31174570/ [ Links ]
Capato, T. T. C., de Vries, N. M., IntHout, J., Barbosa, E. R., Nonnekes, J., &Bloem, B. R. (2019). Multimodal Balance Training Supported by Rhythmical Auditory Stimuli in Parkinson’s Disease: A Randomized Clinical Trial. Journal of Parkinson’s Disease, 10(1): pp. 333-346. doi: 10.3233/JPD-191752. https://pubmed.ncbi.nlm.nih.gov/31884492/ [ Links ]
Carroll, L. M., Volpe, D., Morris, M. E., Saunders, J., & Clifford, A. M. (2017). Aquatic Exercise Therapy for People with Parkinson Disease: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, 98(4), pp. 631-638. https://pubmed.ncbi.nlm.nih.gov/28088380/ [ Links ]
Corcos, D. M., Robichaud, J. A., David, F. J., Leurgans, S. E., Vaillancourt, D. E., Poon, C., Comella, C. L. (2013). A two-year randomized controlled trial of progressive resistance exercise for Parkinson’s disease. Movement Disorders, 28(9), pp. 1230-1240. https://pubmed.ncbi.nlm.nih.gov/23536417/ [ Links ]
Da Silva, A. Z., & Vera Lúcia Israel, P. (2018). Effects of dual-task aquatic exercises on functional mobility, balance and gait of individuals with Parkinson’s disease: a randomized clinical trial with a 3-month follow-up. Complementary Therapies in Medicine. Feb; 42: pp. 119-124. doi: 10.1016/j.ctim.2018.10.023 https://pubmed.ncbi.nlm.nih.gov/30670228/ [ Links ]
Ferreira, R. M., Alves, W. M. G. da C., Lima, T. A., Alves, T. G. G., Alves Filho, P. A. M., Pimentel, C. P., Cortinhas-Alves, E. A. (2018). The effect of resistance training on the anxiety symptoms and quality of life in elderly people with Parkinson’s disease: a randomized controlled trial. Arquivos de Neuro-Psiquiatria, 76(8), pp. 499-506. https://pubmed.ncbi.nlm.nih.gov/30231121/ [ Links ]
Johansson, H., Hagströmer, M., Grooten, W. J. A., & Franzén, E. (2020). Exercise-Induced Neuroplasticity in Parkinson’s Disease: A Metasynthesis of the Literature. Neural Plasticity, 2020 Mar 5;2020:8961493. Doi: 10.1155/2020/8961493. https://pubmed.ncbi.nlm.nih.gov/32256559/ [ Links ]
Knaepen, K., Goekint, M., Heyman, E. M., & Meeusen, R. (2010). Neuroplasticity-exercise-induced response of peripheral brain-derived neurotrophic factor: a systematic review of experimental studies in human subjects.Sports medicine,40 (9), pp. 765-801. https://pubmed.ncbi.nlm.nih.gov/20726622/ [ Links ]
Kurt, E. E.; Büyükturan, B.; Büyükturan, Ö.; Erdem, H. R. & Tuncay, F. (2018). Effects of Ai Chi on balance, quality of life, functional mobility, and motor impairment in patients with Parkinson’s disease, Disability and Rehabilitation, 40:7, pp. 791-797, https://pubmed.ncbi.nlm.nih.gov/28084851/ [ Links ]
Michels, K., Dubaz, O., Hornthal, E., & Bega, D. (2018). “Dance Therapy” as a psychotherapeutic movement intervention in Parkinson’s disease. Complementary Therapies in Medicine . 40. Pp 248-252. https://www.sciencedirect.com/science/article/abs/pii/S0965229918304175 [ Links ]
Moreira, L. R., Palenzuela, Y., Maciñeira, I. E., Díaz, L., y Torres, Y. (2019). Variables clínicas y epidemiológicas de pacientes diagnosticados con enfermedad de Parkinson. Universidad de Ciencias Médicas de Pinar del Río 15(3) https://revgaleno.sld.cu/index.php/ump/article/view/358/html [ Links ]
Pohl, P., Wressle, E., Lundin, F., Enthoven, P., & Dizdar, N. (2020). Group-based music intervention in Parkinson’s disease - findings from a mixed-methods study. Clinical Rehabilitation , 34(4): pp. 533-544. https://pubmed.ncbi.nlm.nih.gov/32070122/ [ Links ]
Roca, R., Smith, V. V., Paz, E., Losada, J., Serret, B., Llamos, N., Cardona, D. (2002). Temas de medicina interna. Tomo 2. La Habana: Editorial Ciencias Médicas. https://docs.google.com/file/d/0B7tMnat81BYsMTRjMDE1ZjItYTFhOC00NjVmLTk3YTAtNDEyNWQ5MDBhMDc5/edit?resourcekey=0-xQ8GtpuVkF1Xv2xSauPnJQ [ Links ]
Saavedra, J. S., Millán, P. A. y Buriticá, O. F. (2019). Introducción, epidemiología y diagnóstico de la enfermedad de Parkinson. Acta Neurol Colomb; 35(3): pp. 2-10. https://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-87482019000500002 [ Links ]
Santos, S. M., Rubens, A., Silva, da, Terra, M. B., Almeida, I. A., Lúcio, B., Ferraz, H. B. (2017). Balance versus resistance training on postural control in patients with Parkinson’s disease: a randomized controlled trial. European Journal of Physical and Rehabilitation Medicine, 53(2): pp. 173-183. doi: 10.23736/S1973-9087.16.04313-6. https://pubmed.ncbi.nlm.nih.gov/27879959/ [ Links ]
Received: April 11, 2023; Accepted: May 23, 2023











 texto en
texto en