Presentación de caso
Implant Setting and Vestibular Bone Board Repair
Instalación de implante y reparación de tabla ósea vestibular
0000-0001-5333-3640Mauricio Toro
1
, 0000-0003-4617-0040Tomás Yoma
2
, 0000-0002-8571-4429Alain Manuel Chaple Gil
3
*
, 0000-0002-2616-1510Eduardo Fernández Godoy
4
5
1Universidad de Chile. Facultad de Odontología, Departamento de Prótesis. Santiago de Chile, Chile
2Práctica Privada. Santiago de Chile, Chile
3Universidad de Ciencias Médicas de La Habana, Facultad de Ciencias Médicas “Victoria de Girón”. La Habana, Cuba
4Universidad de Chile. Facultad de Odontología, Departamento de Odontología Restauradora. Santiago de Chile, Chile
5Universidad Autónoma de Chile. Instituto de Ciencias Biomédicas. Santiago de Chile, Chile
ABSTRACT
Background:
The occurrence of a vestibular bone lamina dehiscence of a fresh alveolus becomes a challenge for rehabilitation treatment of dental implants.
Objective:
To evaluate prosthetic treatment and stability of periimplant soft tissues in an alveolus with advanced oral bone resorption immediately after extraction, by using single fixed prostheses on a dental implant.
Case presentation:
A 29-year-old female patient, without systemic disease, completely toothed, with a thick-scalloped gingival biotype, attended the clinic and her main reason for consultation was not being aesthetically satisfied with her right upper central incisor. Radiographic examination showed advanced oral bone loss, secondary to an infection of the root of the right upper central incisor. In a first surgical phase, the right central incisor was extracted using a traumatic technique with periotomes, and a dental implant was placed. A resorbable membrane was adapted to the vestibular defect and the particulate cortical bone allograft was then compacted into the site in order to fill the space between the collagen membrane and the dental implant. A screw-retained provisional restoration was performed using the extracted natural tooth. The emergence profile was established simply by adding fluid composite resin, until the desired contours were achieved. Radiological and clinical follow-up at six months showed favorable implant evolution. No mechanical or biological complications were observed during this observation period. The oral gingival margin was in a correct position.
Conclusion:
This technique allowed predictable aesthetic-functional outcomes and soft tissue stability in a thick-scalloped gingival biotype with a single fixed prosthesis.
Key words: dental implant; grafted extraction site; bone allograft; bone integration; alveolar repair
RESUMEN
Antecedentes:
La presencia de una dehiscencia de la lámina ósea vestibular de un alveolo fresco se convierte en un desafío en el tratamiento de la rehabilitación con implantes dentales.
Objetivo:
Evaluar el tratamiento protésico y la estabilidad de los tejidos blandos periimplantarios en un alveolo con reabsorción ósea bucal avanzada inmediatamente posterior a una extracción, mediante el uso de prótesis fijas unitaria sobre implante dental.
Presentación del caso:
Una paciente de 29 años de edad, sin enfermedad sistémica, completamente dentada, con un biotipo gingival festoneado grueso, asiste a la clínica y su principal motivo de consulta fue no estar conforme estéticamente en su incisivo central superior derecho. El examen radiográfico mostró la presencia de una pérdida ósea bucal avanzada, secundaria a una infección de la raíz del incisivo central superior derecho. En una primera fase quirúrgica, se extrajo el incisivo central derecho utilizando una técnica atraumática usando periótomos y se colocó un implante dental. Se adaptó una membrana reabsorbible al defecto vestibular y después se compactó el aloinjerto de hueso cortical particulado en el sitio para llenar el espacio entre la membrana de colágeno y el implante dental. Se realizó una restauración provisional atornillada utilizando el diente natural extraído. El perfil de emergencia se estableció simplemente agregando resina compuesta fluida, hasta que se lograron los contornos deseados. El seguimiento radiológico y clínico a los 6 meses mostró una evolución favorable del implante. No se observaron complicaciones mecánicas ni biológicas durante este periodo de observación. El margen gingival bucal estaba en una posición correcta.
Conclusión:
Esta técnica permitió resultados estéticos-funcionales predecibles y estabilidad de los tejidos blandos en un biotipo gingival festoneado grueso con una única prótesis fija.
Palabras-clave: implante dental; sitio de extracción injertado; aloinjerto óseo; oseointegración; reparación alveolar
Background
Subsequent tooth extraction, alveolar bone loss and structural changes of the soft tissues can be predicted. The numerous alterations in the alveolar process may lead to difficulties at the time of implant placement when a prosthetically driven implant position is required.1
The challenge in treatment is when the buccal bone plate presents a dehiscence type defect. Elian et al. described a facial-palatal socket classification where risks could be potentially assessed in regard to potential midfacial recession depending upon the existing socket condition.2 Type 1 sockets were classified as having the buccal bone plate and soft tissues completely intact; Type 2 where the soft tissue was present but a dehiscence bony defect existed, indicating the partial or complete absence of the labial bone plate; and Type 3 where a midfacial recession defect occurred, indicative of loss of the labial bone plate and soft tissues.
Motivated by the complexities of restore bone and function after loss of this structures, the aim of this article was to evaluate prosthodontic treatment and soft tissue stability in an extraction socket with advanced buccal bone resorption, through the use of implant-supported single fixed prosthesis.
Case presentation
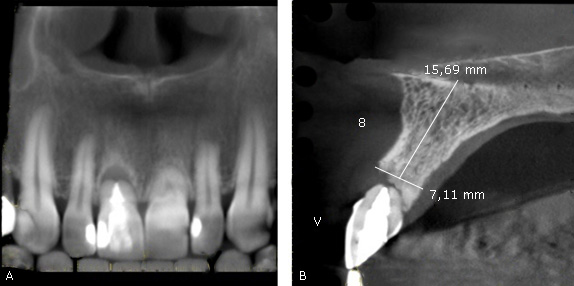
The patient was a 29-year-old female, without systemic disease, completely dentate, with a thick-scalloped gingival biotype.3 The radiographic exam showed the presence of advanced buccal bone resorption secondary to a root infection of the maxillary right central incisor (Tooth 1.1) (Fig. 1- A) and a large osteolytic area on the buccal aspect of the root (Fig. 1-B). The patient’s main complaint was aesthetic.
In a first surgical phase, the right central incisor was extracted using an atraumatic periotome technique (Fig. 2-A). Then, one implant was placed (Tapered Screw-Vent 3,7x13, Zimmer Biomet Dental, Palm Beach Gardens, FL) in the palatal plate of the socket with an average surgical torque of 40 Ncm. After this, a resorbable collagen membrane (BioMend Extend, Zimmer Biomet Dental, Palm Beach Gardens, Fl) (15mmx20mm) was adapted to the bone defect and placed in a position to recreate the buccal plate (Fig. 2-B). Subsequently, particulate cortical bone allograft (Puros Cortical Allograft Particulate, Zimmer Biomet Dental) (0,5 cc) was compacted into the site to fill the space between the collagen membrane and the dental implant (Fig. 2-C). Finally, a screw retained provisional restoration was performed using the extracted natural tooth (Fig. 2-D and 2-E). The emergency profile was established by simply adding composite (flowable), until the desired contours were achieved.
Six months after the implant placement, osseointegration was clinically confirmed. Radiographic and clinical follow-up after 6 months showed a favorable evolution of the implant (Fig.3A). No mechanical or biological complications were seen throughout this observation period. The buccal gingival margin was in a correct position. The osteolytic zone was a follow-up with controls and, the decision of the patient wasn't submitted to invasive treatment.
After several stages, the final restoration with a zirconium dioxide abutment and a full ceramic crown was obtained and cemented (Fig.3B).
Discussion
The dual zone is divided into two regions: the tissue zone and bone zone. The tissue zone is the labial-palatal dimensional change of the vertical region of tissue defined as ranging from the free gingival margin (0 mm) to the labial crest of bone mid-facially. The bone zone is the tissue apical to the osseous crest.4
This case report describes the resolution of an implant-supported rehabilitation with advanced buccal bone resorption. This case shows that minimally invasive extraction and grafting techniques satisfied the critical requirements needed for socket type 2 repair. This is particularly important in the aesthetic zone.4,5,6 The use of particulate bone graft and a resorbable collagen membrane is a predictable technique to manage the lack of the buccal plate in a thick-scalloped gingival biotype.7 Placing a bone graft into the residual gap around an immediate fresh-socket anterior implant with a screw-retained provisional restoration acting as a prosthetic socket seal device, allows to achieve predictable results in terms of implant success as well as soft and hard tissue new formation and stability. Others authors have had similar results with the same technique for reconstruction of the buccal plate. Sarnachiaro et al.8 reported a case series and demonstrates that placing a bone graft, absorbable membrane, and custom-healing abutment at the time of immediate postextraction implant placement results in radiographic reformation of the labial plate dehiscence defect at 6 to 9 months posttreatment. Several factors can influence the amount of labial plate thickness reconstruction such as the amount of labial plate loss, preoperative soft tissue inflammation, and periodontal phenotype.8,9,10,11,12
The use of a natural teeth to build a temporary crown over a dental implant is a widely used technique. It has a several advantages like return the natural anatomy of the teeth and allows create a desire emerge crown profile. The extracted teeth was cleaned and conditioning with phosphoric acid 37 % , after of this hybridized with dental adhesive and adapted with composite resin (A3) and polymerized. These two characters are too important for patients because they can recognize like an Own tooth without an adaptation period and for dentists too because is a versatile and quick technique.
Further research is required to assess the long-term stability of reconstructed labial plates of Type 2 sockets on CBCT (Cone beam computed tomography) with a larger number of patients. Additionally, the histologic evaluation of the reconstructed buccal plate would be important, as this would provide both qualitative and quantitative data on the type of tissues regenerated.
Conclusion
This technique allowed predictable esthetics/functional results and soft tissue stability in a thick-scalloped gingival biotype using a single fixed prosthesis.
Bibliographic references
1.
Papaspyridakos P, Tarnow DP, Eckert SE, Weber HP. Replacing Six Missing Adjacent Teeth in the Anterior Maxilla With Implant Prostheses: A Case Series. Compend Contin Educ Dent. [Internet]2018[access: 01/07/2019];39(6):e1-e4. Available in: https://pmlegacy.ncbi.nlm.nih.gov/pubmed/?term=Replacing+Six+Missing+Adjacent+Teeth+in+the+Anterior+Maxilla+With+Implant+Prostheses%3A+A+Case+Series1.
[ Links ]
2.
Elian N, Cho SC, Froum S, Smith RB, Tarnow DP. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104; quiz 6. [ Links ]
3.
Al-Sabbagh M, Xenoudi P, Al-Shaikhli F, Eldomiaty W, Hanafy A. Does Peri-Implant Mucosa Have a Prognostic Value? Dent Clin North Am. 2019 [access: 01/07/2019];63(3). Available in: https://www.ncbi.nlm.nih.gov/pubmed/310971453.
[ Links ]
4.
Basualdo J, Ivankovic M, Kuzmicic J, Fernández E. Atraumatic Extraction and immediate implant placement into infected site with the ice cream cone technique and L-PRF: A Case Report. Revista clínica de periodoncia, implantología y rehabilitación oral. 2018 [access: 01/07/2019]; 11(1). Available in: https://scielo.conicyt.cl/scielo.php?script=sci_arttext&pid=S0719-01072018000100043&nrm=iso4.
[ Links ]
5.
Attia MS, Mohammed HM, Attia MG, Hamid M, Shoeriabah EA. Histological and histomorphometric evaluation of hydroxyapatite based biomaterials in surgically created defects around implants in dogs. J Periodontol. 2018 [access: 01/07/2019];90(3). Available in: https://aap.onlinelibrary.wiley.com/doi/abs/10.1002/JPER.17-04695.
[ Links ]
6.
Le B, Borzabadi-Farahani A, Nielsen B. Treatment of Labial Soft Tissue Recession Around Dental Implants in the Esthetic Zone Using Guided Bone Regeneration With Mineralized Allograft: A Retrospective Clinical Case Series. J Oral Maxillofac Surg. 2016 [access: 01/07/2019];74(8). Available in: https://www.joms.org/article/S0278-2391(16)30115-X/pdf6.
[ Links ]
7.
Wang Y, Zhang Y, Miron RJ. Health, Maintenance, and Recovery of Soft Tissues around Implants. Clin Implant Dent Relat Res. 2016 [Access: 01/07/2019]; 18(3). Available in: https://onlinelibrary.wiley.com/doi/abs/10.1111/cid.123437.
[ Links ]
8.
Smith R, Tarnow D, Sarnachiaro G. Immediate Placement of Dental Implants in Molar Extraction Sockets: An 11-Year Retrospective Analysis. Compend Contin Educ Dent. 2019 [access: 01/07/2019];40(3). Available in: https://www.ncbi.nlm.nih.gov/pubmed/308295008.
[ Links ]
9.
Saito H, Chu S, Zamzok J, Brown M, Smith R, Sarnachiaro G, et al9.
. Flapless Postextraction Socket Implant Placement: The Effects of a Platform Switch-Designed Implant on Peri-implant Soft Tissue Thickness-A Prospective Study. Int J Periodontics Restorative Dent. 2018 [access: 01/07/2019]; 38(Suppl):s9-s15. Available in: Available in: https://www.ncbi.nlm.nih.gov/pubmed/30118528
9.
[ Links ]
10.
Chu S, Saito H, Salama M, Garber D, Salama H, Sarnachiaro G, et al10.
. Flapless Postextraction Socket Implant Placement, Part 3: The Effects of Bone Grafting and Provisional Restoration on Soft Tissue Color Change-A Retrospective Pilot Study. Int J Periodontics Restorative Dent . 2018 [access: 01/07/2019]; 38(4):509-16. Available in: Available in: https://www.ncbi.nlm.nih.gov/pubmed/29889914
10.
[ Links ]
11.
Chu S, Salama M, Garber D, Salama M, Sarnachiaro G, Sarnachiaro E, et al11.
. Flapless Postextraction Socket Implant Placement, Part 2: The Effects of Bone Grafting and Provisional Restoration on Peri-implant Soft Tissue Height and Thickness- A Retrospective Study. Int J Periodontics Restorative Dent . 2015 [access: 01/07/2019]; 35(6):803-9. Available in: Available in: https://www.ncbi.nlm.nih.gov/pubmed/26509983
11.
[ Links ]
12. Chu S, Sarnachiaro G, Hochman M, Tarnow D. Subclassification and Clinical Management of Extraction Sockets with Labial Dentoalveolar Dehiscence Defects. Compend Contin Educ Dent. 2015 [access: 01/07/2019];36(7). Available in: https://www.ncbi.nlm.nih.gov/pubmed/26247445
[ Links ]